To screen or not to screen
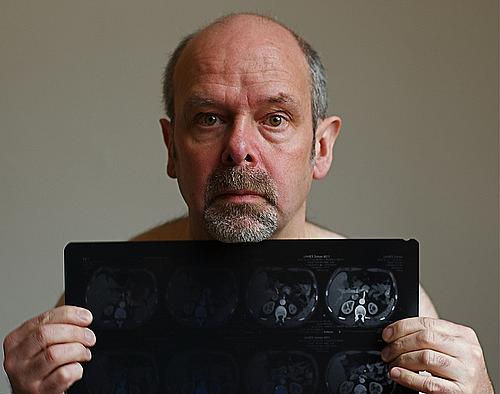
Man holds a CT scan that revealed his bowel cancer.
I began hearing from people who I hadn’t been in touch in years after posting my first “Cancer in Context” blog entry, roughly two months ago, in which I wrote that I have stage 4 lung cancer. Initially, friends sent condolences. Some expressed fears about their own lifetime smoking habits, asking me if I thought they should get screened for the deadly disease.
I’m not a doctor, so I suggested they consult with one. Surprisingly, for those my age, which is 50, the answer to the screening question is probably no. The American Cancer Society (ACS) just updated its guidelines at the beginning of the year, and I did not meet the criteria for a lung cancer screening.
I recently spoke with Dr. Leonard Lichtenfeld, the Deputy Chief Medical Officer for the ACS. I told him how I wished I had undergone screening earlier, thinking my cancer would have been caught before it could spread to my bones and my brain.
“I would not have screened you,” he said bluntly.
According to the ACS criteria, it is appropriate for active and former pack-a-day smokers aged 55 to 74, with no signs or symptoms of lung cancer, to get screened. Former smokers must have quit in the last 15 years. The ACS stresses that active smokers who are 55 or older should not use screening as a substitute for quitting. The decision about whether a person should get screened should be made with their healthcare provider, the ACS said.
The ACS guidelines do not recommend screening for non-smokers, or for young people who smoke. That’s because the incidence of lung cancer is relatively low among people younger than 50, though the incidence increases rapidly after age 60. One reason for the caution is that a low-dose computed tomography scan and subsequent tests can be harmful.
In 2004, the U.S. Preventive Services Task Force (USPSTF) said evidence was insufficient to recommend for or against screening for lung cancer in people who did not have symptoms. The panel has not updated its recommendation since 2004.
In Lichtenfeld’s blog, “Dr. Len’s Cancer Blog,” he wrote about the topic after the new guidelines were released.
Lichtenfeld told me that his own doctor had detected a 3-millimeter nodule on his lung several years ago, but he declined further testing. Lichenfeld has never smoked and he felt that the risk of getting cancer from the CT scan outweighed the possibility that the nodule was actually cancerous.
“The testing process is not benign,” he said. There’s the scan itself, a low-dose computed tomography, possibly followed by a biopsy that can cause the lung to collapse. The patient may undergo a bronchoscopy to look into the lung, or even get a recommendation to have chest surgery.
Lung cancer, which is nearly always fatal, is the leading cause of cancer death in the United States. The ASC estimates that there were roughly 226,000 newly diagnosed lung cancer cases in the United States in 2012, and 160,000 succumbed to the disease. The incidence of lung cancer, however, is on the decline in the United States.
When it comes to screening, effectiveness depends on the type of cancer and if the patient belongs to a high-risk group. Pap smears are a well established effective test for cervical cancer. There is solid evidence supporting screening for colorectal cancer, while prostate cancer screening has a mixed record, he said.
There is still substantial debate about when it is appropriate to use mammograms to screen for breast cancer, Lichtenfeld said. The ACS is reviewing its own recommendation. But as of today, their guidelines suggest regular breast cancer screening beginning at age 40. By contrast, the USPSTF recommends biennial screening mammography for women aged 50 to 74.
Today, there is a desperate need to develop a screen for ovarian cancer, which has no symptoms until it is in its late stages, he added.
“There has been confusion in the public and in the profession about what the right thing to do is when it comes to cancer screening,” Lichtenfeld said.
“The reason is because it’s very difficult for the average physician, let alone the average person, to sort through all the scientific issues and all the debate that’s going on. We have not done the best job of answering the questions people have. I wish we had done a better job.”
This article has been reposted with permission from the Thompson Reuters blog "Cancer In Context."
Image by Menage a Moi via Flickr

