Venturing Into A Wildly Unregulated Branch of Medicine: Fertility Treatments

My generation also came of age alongside reproductive technologies: in-vitro fertilization (I.V.F.), frozen sperm, donor eggs, and surrogacy. I vividly remember reading front-page stories about the first test-tube baby born in Britain (in 1978) and about the first donor-egg baby born (in 1984). These advances were so extraordinary that my girlfriends and I began to believe that almost anything would be possible by the time we were ready to have kids…that is, if we chose to have kids.
I can recite from memory the names and ages of the celebrities who first seemed to beat the biological clock: Photographer Annie Leibovitz (twins at 52), supermodel Cheryl Tiegs (baby at 52), actress Geena Davis (twins at 48). Now, it seems just about every other 40-plus female in Hollywood has conceived through I.V.F.
Bombarded by these relentless endorsements for older motherhood, many middle-class, educated, Gen-I.V.F. women like myself started thinking, “Wow, science is finally beating Mother Nature.” We reassuringly told each other, “It’s okay to delay motherhood while we pursue our careers. If we run into trouble, well, there are always fertility treatments.” Science and technology became our New God.
My own fertility story has four chapters.
Chapter One: Ambivalent about motherhood and thrilled to be ensconced in a meaningful career, I married in my mid-thirties and five years later started trying to make a baby the old-fashioned way.
Chapter Two: A four-year odyssey into assisted reproductive technology (A.R.T.), which 99 percent of the time means I.V.F. With A.R.T., the sperm and egg are handled outside of the womb (A.R.T. does not include straight hormone therapy or intrauterine insemination). Most A.R.T. requires very expensive injections, via needles to the abdomen, thigh or buttock, aimed at controlling your body’s hormones and stimulating your egg production. Notoriously, they can also fuel horrible mood swings and alter your personality.
During the years I underwent I.V.F., I met women so addicted to the hope the science offered that they’d endured as many as 18 rounds of treatment. My husband Michael and I abandoned the I.V.F. treadmill after four failed cycles, including one emotionally devastating miscarriage and another in which my ovaries produced no eggs at all.
For the most part, this $4-billion-a-year biotech industry is not invested in providing appropriate patient education that can help women and couples determine when to cease treatments, or support them in coming to terms with the indescribably painful fate of their biological childlessness. Still reaching for the stars ourselves, Michael and I continued on to Chapter Three: The Donor Egg Phase.
At this point a third party was introduced into the sacredness of the conception process, deeply challenging not only our values, but also our core sense of identity. We talked endlessly about ethics, spirituality and the excruciating realization that we were actually considering buying another woman’s eggs, commodifying her.
Still, sad to say, despite trepidation, disabling bouts of insomnia and self-flagellation, our obsession to procreate prevailed. Slowly but surely, we became that thing: Fertility Junkies. We began working with a donor egg agency, spending endless hours online, often surreptitiously logging on at 3 a.m., addictively “shopping” for the perfect egg mother; maybe one who would look a little bit like me.
After several more months of tears and insomnia, we chose an attractive 21-year-old who then had to undergo rigorous testing. When the nurse finally called to report that this donor was infertile, we were stunned.
“Okay,” Michael and I told each other, “This is an omen from the universe telling us to stop.” But we didn’t. Instead we started fanatically trolling the Internet again. We found another seemingly good fit — a 28-year-old mother who had donated to another couple only six months earlier. The clinic synchronized our hormone levels and prepared her ovaries to generate quality eggs and my uterus to develop the kind of lining that an embryo (or two) wants to call home. But one day before the embryo transfer was scheduled to take place, much to our incomprehension and shock, the doctor called to inform us that none of our donor’s dozen eggs had fertilized.
“There is something obviously wrong with her,” he said, lending his industry’s own strange brand of support. “Given the drugs she was taking, she should have produced many more eggs and they should have fertilized. I would not recommend using her again, but I do hope you will try another donor cycle. You are a perfect candidate.”
At that point, maimed and almost immobilized by grief, I slunk into a depression that kept me in bed for months. Somehow, I don’t know how, we initiated Chapter Four of our saga: the path to parenthood through adoption. Michael’s and my seven-year-long journey to have a child ended the moment we laid eyes on our newborn son, Sammy. As he snuggled next to his birth mother in a hospital bed, a maternal force as great as a tsunami welled up inside of me, and I gave thanks that he had finally arrived through the spiritual cocoon of my long-recited prayers. At the same time, I couldn’t quite comprehend that he was actually “my son” and I was now “his mother.” In an instant, we all assumed new identities that would bind us together for life.
Like wide-eyed pioneers, Michael and I had ventured into a wildly unregulated and subterranean branch of medicine. Most of the information circulating about I.V.F. predominantly focuses on its successes; there is virtually no counterbalance to inform us about high failure rates, its devastating effect on couples, or its bioethical conundrums.
Fortunately, former infertility patients and advocates are beginning to talk about all of this publicly, and the first independent forum to crack open the myths and hidden realities of infertility and the power of science to reverse it, The Cycle: Living A Taboo, took place in New York City in September 2013.
My next post will outline the 10 things I wish someone had told me before I embarked on my ride through hell.
Image by Kit4na via Flickr
A version of this post originally ran in Lilith magazine and has been used with permission.
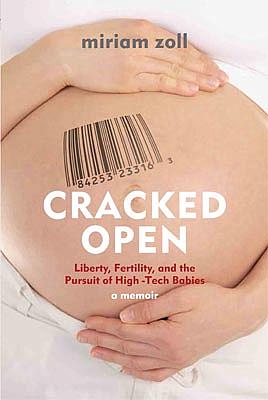
Miriam Zoll is an award-winning writer and author of Cracked Open: Liberty, Fertility and the Pursuit of High-Tech Babies, founding co-producer of the Ms. Foundation for Women’s original “Take Our Daughters To Work Day,” and a board member of Our Bodies Ourselves and Voice Male Magazine.

