To Get California Covered, People First Have to Enroll

The national narrative surrounding the Affordable Care Act’s implementation has revolved around opponents’ attempts to discredit the law and the Obama administration’s botched rollout of HealthCare.gov – where people can shop for policies on what’s known as the Health Insurance Marketplace.
Meanwhile in California, a state that has set up its own marketplace (also called an exchange), the effort to get people signed up for insurance has proceeded with little partisan rancor, and at a quickening pace.
Of the estimated 5.3 million people eligible for health insurance through the exchange, Covered California announced this week that from October 2013 through the end of December 2013, 500,108 individuals had enrolled in Covered California health insurance plans. For the same period, 584,000 were determined to be likely eligible for Medi-Cal.
Enrollment in November was more than double what it was in October, and December enrollment -- 400,096 -- was nearly four times that of October and November combined. At anything close to the December rate, Covered California should easily meet its stated goal of getting 700,000 people insured by March 31 -- the end of open enrollment, and the last day one can sign up for coverage without incurring a tax penalty.
Nonetheless, millions of Californians remain uninsured. The number stood at 7 million in 2012, according to the California Health Care Almanac. Over the next few months, ReportingonHealth.org will examine major issues that keep Californians from signing up, especially those with lower incomes.
CoveredCA.com, the state exchange’s website, has been relatively problem-free, especially when compared with the troubled federal site. But even with a functioning online health insurance portal, a sizable chunk of the uninsured, in California and elsewhere, don’t have broadband access at home, and there are only so many libraries.
In a June 2013 study, the Public Policy Institute of California found that 69 percent of people in the state had broadband Internet access at home, and of the 31 percent who don’t, most are likely on the lower end of the income scale, and thus far more likely to be uninsured. So, the people who need CoveredCA.com the most are the least likely to be able to access it easily.
This same demographic is also more likely to be eligible for Medi-Cal, the state’s Medicaid program, which has been expanded under the ACA. CoveredCA.com determines if a consumer is Medi-Cal eligible, so it’s imperative to reach across the digital divide.
Outreach to low-income Californians has met with mixed success, with enrollment in the Latino community lagging far behind its proportion of the population. Latinos are less likely to have computers. And another issue facing Latinos is the language barrier; according to data cited by Covered California, 28.8 percent of California households are primarily Spanish speaking.
“The success of the California health exchange, known as Covered California, depends on robust enrollment of Latinos, who make up about 60 percent of the state’s uninsured population and are generally younger and healthier than other potential enrollees,” notes Kaiser Health News journalist Anna Gorman in a recent article.
Yet the most recent data from Covered California shows that only 5.5 percent of enrollees through December 2013 were primary Spanish-speakers, and only 18.7 percent self-identified as Latino (this percentage could be slightly higher or lower as this answer was not required) — hardly surprising, given that Covered California only released a Spanish-language paper enrollment form on Dec. 30. Courtesy of Covered California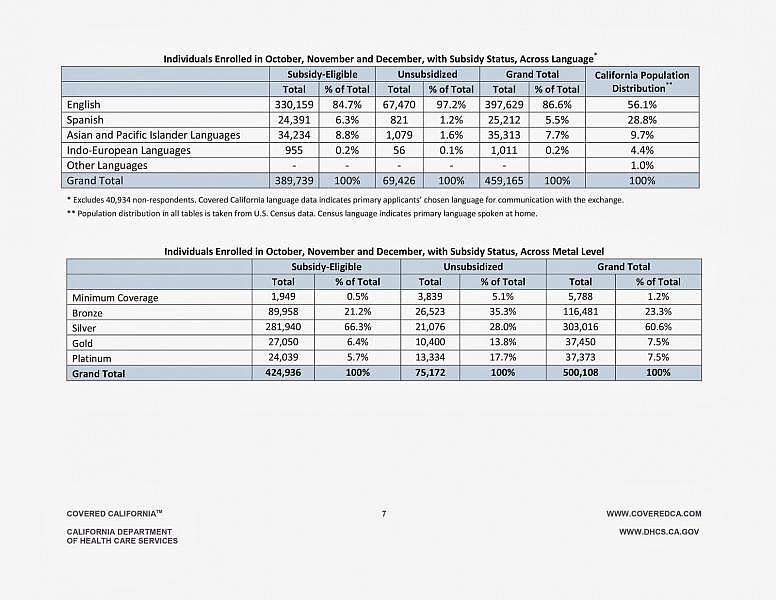
In addition to that oversight, other questions remain. Has messaging about health insurance sign-ups reached Spanish speakers? Are there enough Spanish-speaking people to help with enrollment? In this blog, we will explore the efforts to enroll this population and try to better understand why they’ve apparently been stymied.
Covered California has what its communications team calls multiple “paths to enrollment.” In addition to the website, people can seek help to enroll from nonprofit community clinics; certified enrollment counselors (CECs), who work out of certified enrollment entities; county eligibility workers, who are employees of county health and other social service agencies; and certified insurance agents.
Different rules govern exactly how these assisters can help people sign up for insurance. For instance, individual CECs receive a $58 bonus for each person enrolled, and cannot advocate for one coverage plan over another, only display all of the options available to the applicant. Certified insurance agents are not paid by Covered California, but receive a commission from the insurance company for each sale -- just as with any other insurance policy sale.
The state is still in the process of training CECs and insurance agents and will soon launch a navigators training program to help more people sign up. In upcoming posts, we’ll look at what that training entails and if demand for sign up help is being met. You’ll hear from the enrollers on the front lines, as well as Californians trying to get coverage.
Image by hang_in_there via Flickr

