Genetic Incidentalomas
Brandon Alspaugh is worried. He's an interventional radiologic technologist at South University in Charlotte, NC, taking human genetics in preparation for physician's assistant school. When he got to the end of my textbook, where I ask students to e-mail me their concerns, he wrote the following:
"Dr. Lewis,
Coming from the medical field, I worry that personal genomics, while useful in terms of screening for genetic disease, will come to have the same effect as full-body CT scans, where the amount of noisy data generated will drown out the important bits. As with atypical anatomy, a person might spend a month chasing down a suspicious allele only to find it's a normal variant of a beneficial gene."
Brandon's describing a new breed of incidentaloma, looking for one sign of abnormality that turns up what could be another. I went in for a CT scan of my lungs, for example, and the doctor fretted over my polycystic liver. A friend had it much worse. She volunteered to be a control in an Alzheimer's imaging trial, and her scan revealed two brain aneurysms!
The term "incidentaloma" was coined to describe an adrenal tumor (hence the "oma") found on a scan looking for something else. More recently, incidentalomas are arising as collateral damage from the sequencing of the human genome and the genetic testing it has spawned. We now have too much information, and too few people (genetic counselors) to translate what we do know.
The founding fathers (there were no mothers in the famed "amino acid club") who deciphered the genetic code back in the 1960s would not have predicted genetic incidentalomas; surely all DNA was translated into protein. Over the years, the percentage fell, precipitously, so that now we know (or suspect) that a mere smidge under 2% of the genome actually encodes proteins – a little like a John Grisham novel in which much of the story turns out to be, if not irrelevant, then not central to the main story.
Genetics is about variation, not just disease, and I fear that because of this, a direct-to-consumer genetic testing company, anxious to spew as much information as possible at its clientele, could indeed impart a sequence or two that is innocuous, as Brandon the astute student suggests. And genetic incidentaloma-ism extends to well known protein-encoding genes. I saw this the day after I heard from Brandon, when a nurse-midwife at the practice where I provide genetic counseling called me, alarmed at a lab result for a patient.
"What's SMN? The blood test results came back with a risk of 1 in 632 for SMA, based on SMN copy number. What's that?"
If the nurse-midwife didn't recognize it (and why would she?), I feared, the patient certainly wouldn't. And so I explained that SMN is the gene "survival motor neuron" and various versions of it are implicated in the most common type of spinal muscular atrophy (SMA),a recessive disease in the same general incidence ballpark as cystic fibrosis – 1 in 38 of us is a carrier. (I elected not to get into copy number variants, a recently-recognized form of mutation.)
I knew that more widespread testing for SMA was beginning because of pending legislation (The SMA Treatment Acceleration Act) "to authorize the Secretary of Health and Human Services to conduct activities to rapidly advance treatments for spinal muscular atrophy, neuromuscular disease, and other pediatric diseases, and for other purposes." Some three dozen labs offer carrier testing at GeneTests.org.
I also knew about SMA from a young hospice patient I'd visited in a nursing home. She was 7, a long-term survivor for this disease known as "baby ALS" that is usually fatal by age 3. (Also see Families of SMA.)
So should the midwife tell the patient, who must have signed something but likely has no idea her blood was tested for SMA, her carrier risk? Would the patient understand that the test indicates her risk is well BELOW that of the average person for something that she probably doesn't know exists? Does alerting and possibly alarming many people justify the additional SMA cases that screening might prevent by detecting potential parents who are both carriers? After all, this is the approach that has nearly vanquished Tay-Sachs disease. (See A Brief History of Genetic Testing.)
A slippery slope looms.
How far are we from personal genome scans that yield long lists of risks, some meaningful, some not? Who will develop the criteria for what is meaningful, for what a patient should know? Should a health care practitioner disclose ALL genetic information so as not to be paternalistic, or shield the patient from test results to "do no harm?" What happens when a genetic risk identified today declines with a future discovery? (Not everyone taps into 23andMe on a daily basis to check for updates.) Or should a patient indeed be told absolutely everything, in case there is something he or she can do, environmentally speaking, to alter genetic destiny?
As with all matters scientific, the more we learn, the more we find out that we don't know. It will be interesting to see how the impending avalanche of genetic incidentalomas plays out.
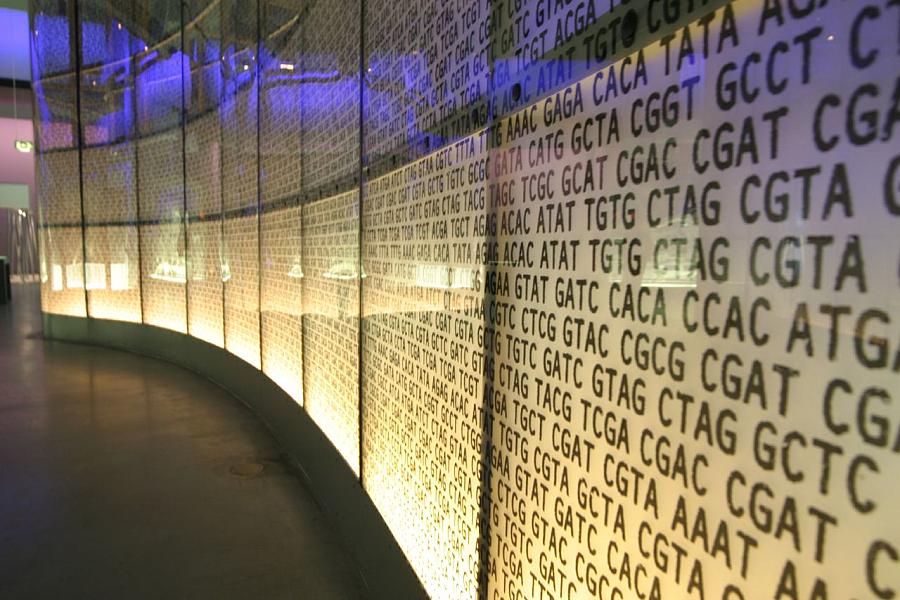
Photo credit for exhibit from London Science Museum: John Goode via Flickr

