The Health Divide: STD rates are increasing, and not just among young adults has been sent

(Photo by Ricky Carioti/The Washington Post via Getty Images)
The numbers are alarming. Cases of chlamydia, gonorrhea, and syphilis increased 7% from 2017 to 2021, reaching 2.5 million cases, according to the Centers for Disease Control and Prevention.
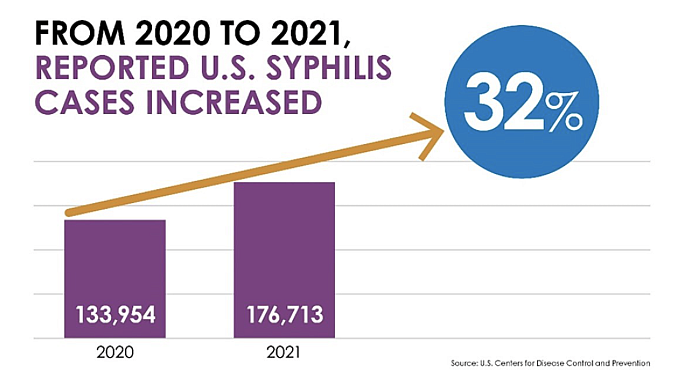
Syphilis infections surged a whopping 32% in just one year, from 2020 to 2021.
These numbers are scary because the data reflects only reported cases. The numbers are likely higher because many cases go undiagnosed, placing even more people at risk. After all, they don’t know they are infected.
Sexually transmitted infections (STIs) are increasing in the United States, and this trend has persisted for several years.
One important point often overlooked in media discussions is that STIs affect every segment of the population. The only individuals not impacted are those who abstain from sexual activity.
While individuals under the age of 25 and gay and bisexual men represent the highest number of cases — accounting for half of the total — STI infections among adults aged 55 and up more than doubled in the U.S. from 2012 to 2022.
Syphilis cases among those 55 and older rose seven-fold in 10 years, while gonorrhea increased nearly five-fold and chlamydia tripled.
In addition to a rise in STIs among seniors, racial and ethnic groups such as African Americans, Hispanics, and American Indians/Alaska Natives experience higher rates of STIs compared to their white counterparts.
One in five Americans has an STI
African Americans face disproportionately higher rates of STIs compared to other racial and ethnic groups in the United States.
In 2018, African Americans made up 42% of the 37,968 reported new HIV cases.
In 2022, 31% of reported cases of chlamydia, gonorrhea, and syphilis occurred among non-Hispanic Black or African American individuals, despite this demographic representing only 12.6% of the U.S. population.
Several factors are driving these disparities, including limited access to quality health care, lack of comprehensive sex education, racism, and socioeconomic challenges, according to the CDC.
Health care experts and organizations dedicated to reducing the spread of STIs face significant challenges in promoting safer sex. When an organization launches a new billboard promoting condom use, they often face backlash from parents who respond with statements like, "How dare you encourage my kids to have sex?"
It’s also a common misconception that committed couples or those in monogamous, long-term relationships are immune to STIs. However, health specialists emphasize that everyone must prioritize their health. Knowing one’s status through testing is essential.
"Everyone should think about having a conversation with their partner around STD testing coming from a place of concern and care," Savita Ginde, a women's health specialist, told USA Today.
If older adults believe they are immune to STIs, they should consider the case of Tracey Whitmore, a woman I first interviewed in 1996 and who served as a programming assistant for an HIV/AIDS program in Milwaukee.
Whitmore educates African Americans about the importance of practicing safer sex and knowing their HIV status. She speaks from personal experience rather than relying on charts or studies.
She was diagnosed with HIV on August 6, 1996, after contracting the virus from her longtime boyfriend, whom she believed was in a monogamous relationship with her.
They had unprotected sex twice.
She didn’t know his HIV status, and said she struggled with what she called “condom negotiation” — the crucial conversation that should take place before sex regarding protection. Many women worry that bringing up the topic of condoms will ruin the mood or cause their partner to feel mistrusted, leading to fears of rejection.
At that moment, Whitmore felt powerless. However, after her diagnosis at 36, she now dedicates much of her time to educating others about the importance of practicing safe sex. Her experience represented a growing trend: older women contracting sexually transmitted diseases like HIV, chlamydia, gonorrhea, and syphilis.
Whitmore shared her story to highlight the fact that middle-age and older adults are at risk of STIs and need to discuss their sexual history.
“This generation rarely considers using protection because they came of age at a time when sex education in school did not exist, HIV was virtually unheard of, and their main concern in seeking protection was to avoid pregnancy,” wrote Janie Steckenrider, associate professor of political science at Loyola Marymount University, in her 2023 comment piece “Sexual activity of older adults: let's talk about it.”
Education must be a part of the equation
Many urban areas with high STI rates are advocating for people to know their status.
When pre-exposure prophylaxis (PrEP) became available to help prevent the spread of HIV, there was a significant initiative to encourage individuals to know their HIV status. Health clinics began offering free testing and low-cost or no-cost medication to help protect those at risk.
To address the increase in STIs, health officials are considering making doxycycline available to sexually active individuals who don’t use condoms. The inexpensive antibiotic, which has been on the market for 50 years and is commonly used to treat various infections, is being evaluated by the CDC.
In June, the CDC issued recommendations for using doxycycline as a preventive measure, akin to a morning-after pill for STIs, for at-risk gay and bisexual men, men who have sex with men, and transgender women.
To be effective, doxycycline must be taken within 72 hours after risky sexual contact.
While medications show promise, education is imperative in addressing STIs. The media plays a pivotal role in informing the public about the rising threat posed by STIs as well as the resources available. Consistent reporting and profiles and features highlighting organizations and people who are dedicated to mitigating the spread of STIs is an essential part of the health beat.
Given that 20% of the US population has an STI, and those numbers are continuing to rise, this is an area ripe for more coverage.

