The Health Divide: Why aren’t we talking more about the unequal toll of dementia on Black families?

(Photo via Getty Images)
After spending 20 years in prison, Mr. Brooks had one main goal: he wanted his mother to live long enough to witness the positive changes in his life.
While incarcerated, Brooks worked hard to better himself. He earned his GED and obtained several skill certifications.
After his release, he went to see his mother, but she barely recognized him. His mother was suffering from a progressive form of dementia.
“I received both a blessing and a curse. The blessing is that my mom lived long enough to see me free, but the curse is that she barely remembered who I was,” Brooks said.
Brooks, who declined to share his first name, was one of many African Americans who shared their story at the “Loving those with dementia/Alzheimer’s” breakfast at Healing Grace Baptist Church in Milwaukee a couple weeks ago. The event aimed to help people better understand the impact of dementia on a person’s thoughts and behaviors. It also provided practical and holistic ways to show love and care for those affected by dementia and offered resources for caregivers.
Approximately 6.7 million Americans aged 65 and older have Alzheimer's, a figure that is expected to more than double by 2060 to nearly 14 million adults. While anyone can develop dementia, the disease affects women and African Americans at significantly higher rates than white individuals, according to the Centers for Disease Control and Prevention. The number of African Americans with Alzheimer’s is projected to increase fourfold by 2060.
“If you are African American, there is a possibility that you have a friend or family member who has been affected by dementia. I want you to understand that you are not alone in this journey; numerous resources and services are available to support you during this challenging time,” said Shanelle Snowden, who runs Legacy Home Health Services, a home health agency in Milwaukee that assists individuals and families facing these difficulties.
Many Blacks suffer in silence
Snowden, the keynote speaker at the dementia breakfast, spoke from personal experience. At a young age, her mother was diagnosed with early-onset dementia.
She described the significant challenges her family faced in obtaining quality care. With everyone contributing, they successfully supported their loved one, though it often caused a lot of stress and strong emotions. In 2016, after her mother died, Snowden sought to honor her legacy by addressing the shortcomings in qualified services within the industry. She established her home health care agency, which provides specialized care for dementia patients.
Snowden emphasized that for caregivers of those with dementia, listening to and learning from their perspective is essential. She urged them to avoid correcting their perception of reality. The goal is to ensure their comfort.
Although Blacks are twice as likely as white Americans to develop dementia, Snowden said many Blacks suffer in silence when caring for a loved one with dementia because of the limited resources available and people not knowing how to find support. (The Center for Health Journalism hosted a webinar last year for reporters seeking to go deeper on these issues.)
Dementia significantly affects both the Black community and women, with women facing the greatest impact. Out of the nearly 7 million people aged 65 and older living with Alzheimer's in the United States, almost 4 million are women.
Around 14% of Black individuals over 65 suffer from dementia, compared to 10% of white individuals. This disparity is likely underestimated, as many Black individuals either go undiagnosed or do not seek medical attention required for a proper diagnosis.
“Many of us endure our struggles in silence due to a variety of factors, including the stigma surrounding dementia and feelings of isolation, guilt, and lack of awareness about the challenges of caregiving,” Snowden said.
The challenging nature of dementia's progression often leads caregivers to burn out because they avoid seeking help or don’t know where to go for it.
Caring for someone with dementia presents significant challenges, mainly due to stress and drastic changes in behavior, such as mood swings and forgetfulness. As the disease advances, many caregivers become full-time providers, sacrificing their careers and lives because their loved ones cannot be left alone.
In a moving story published last year by AP, Kat Stafford told the story of Constance Guthrie and her daughter, Jessica, who put her own life on hold to care for her mother, who has Alzheimer’s.
“When you think about how I spent so long trying not to repeat this cycle of poverty, now I’m sitting in a place where I make a pretty good salary, and yet I’m not setting myself up for the future that I know that I should have,” Jessica told Stafford.
The struggle can be magnified when caregivers reflect on their loved one before their diagnosis. The changes can manifest as angry outbursts and aggressive behaviors, including shouting, verbal threats, cursing, physical violence, and property damage — behaviors that do not reflect their identity.
Dementia is a condition that arises when healthy neurons and nerve cells in the brain cease to function and begin to deteriorate. This process significantly impairs cognitive abilities such as reasoning, memory, problem-solving, and judgment. As a result, individuals with dementia often encounter feelings of embarrassment, frustration, and condescension, which can manifest as anger or unkind behavior. Understanding these dynamics is essential in addressing the challenges faced by those living with dementia.
Black individuals are underrepresented in clinical trials
Among Black Americans aged 70 and older, over 21% are living with Alzheimer’s. The Alzheimer’s Association reports that 65% of Black Americans know someone with dementia.
However, less than half feel confident finding culturally competent care. Even more concerning is that half of those surveyed have faced discrimination while seeking care for a person living with dementia.
Daniel Bateman, an assistant professor of psychiatry at the Indiana University School of Medicine and a scientist at the university's Center for Aging Research, said there are hypotheses explaining the higher rates of dementia in Black populations.
“There are higher rates of diabetes, hypertension, high cholesterol, heart disease, and diabetes in African Americans compared to whites. All of those are risk factors for Alzheimer’s and dementia,” Bateman told USA Today.
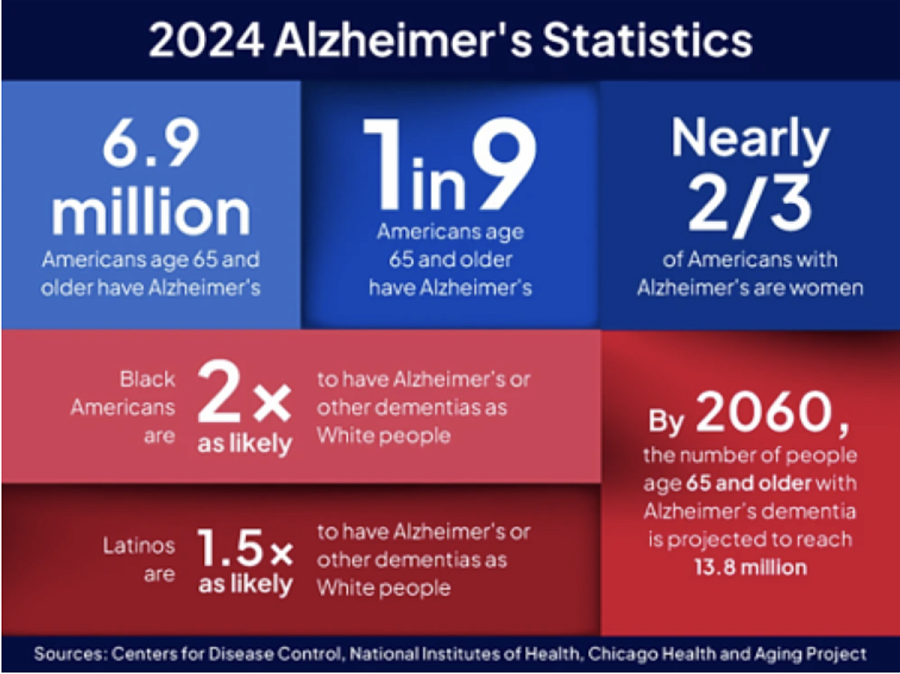
(Graphic via USAgainstAlzheimer’s)
Researchers have connected changes in the brain to certain forms of dementia and are investigating why these changes happen in some people but not others. For a small number of people, rare genetic variants that cause dementia have been identified.
Further research is investigating the role of various stressors, including limited educational opportunities, exposure to poverty, violence, environmental pollutants, early life adversities, less access to health care, and systemic racism.
Alzheimer’s disease is the most prevalent form of dementia, accounting for 65% of diagnoses in the U.S. Other forms include vascular dementia, Lewy bodies dementia, frontotemporal dementia, and mixed dementia.
A 2018 study found that African Americans have a higher incidence of all five types of dementia, particularly after a stroke. Snowden emphasized that the high rates of dementia in the African American community have been difficult to research, mainly because Black individuals are often underrepresented in clinical trials, research studies, and screenings that help facilitate earlier diagnoses.
Snowden and others have suggested that more media attention on these issues could encourage greater participation from African Americans in clinical trials. Such coverage could also combat the stigma associated with the disease. If dementia is not openly discussed within the community, the media could play a vital role in fostering that much-needed dialogue.
There’s a common misconception that dementia only affects older individuals. While the majority of those diagnosed are older adults, according to the Alzheimer’s Society, one in three of those diagnosed with Alzheimer’s before age of 65 are considered to have early-onset Alzheimer’s disease. Young onset dementia is uncommon, and because of its ability to mimic other health conditions, the symptoms are often overlooked.
Snowden said while dementia can seem like a daunting disease where a person feels alone, faith can be a powerful resource for caregivers.
“Turn to prayer when you are feeling overwhelmed, and remember caregiving is an act of love,” she said.

