In first year, exchange grappled with Latino enrollment challenges
María G. Ortiz-Briones wrote this series for Vida en el Valle as a 2014 California Endowment Health Journalism Fellowship. Other parts of this series include:
Covered California director Lee pleased with enrollment process
Not long after Covered California opened for business last October to sign up residents for the controversial Affordable Care Act, it ran into problems and headaches that were more pronounced in the state's Latino community.
Miriam González — along with thousands of uninsured Latinos — was confused, afraid or daunted by the complexity of the new health care reform and how it would affect them. Others preferred information in Spanish or that sign-ups be done in face-to-face meetings.
That trepidation caused major headaches for Covered California officials, who saw underwhelming Latino enrollment through the end of 2013. Of 500,108 Californians who enrolled and selected health insurance plans by Dec. 31, only 74,090 Latinos (or 18 percent of the total) had enrolled.
Covered California's goal was to enroll 265,000 Latinos during the six-month open enrollment period. In the first three months, only 28 percent of them had signed up.
In California, where Latinos are now a plurality of the population at 40 percent and represent 61 percent of the state's uninsured, the under-enrollment figures were troubling.
When the April 15, 2014 deadline arrived, Latino enrollment came in at 28 percent (305,106) of the overall total. That surpassed official projections by 40,106.
What happened? California has been a leader in health care reform, and was the first state to create a health benefit exchange following the passage of the federal health care law in 2010.
How did Covered California get Latinos like González, a stay-at-home mother with two children, to overcome their hesitancy?
Vida en el Valle examines the rollout of the Affordable Care Act, problems that came up and how Covered California worked to solve them.
Latinos didn't know enough
Last October, González knew about the Affordable Care Act, but she didn't feel she had enough information to persuade her to take the next step to obtain health insurance.
Her children are covered through Kaiser Permanente's Child Health Program. Her husband has health coverage through his work. González, a 26-year-old Fresno resident, was the only one not covered.
She was the perfect candidate for the Affordable Care Act, which was designed to help reduce health disparities, especially in communities of color.
The part-time Fresno City College student was confused about the federal program.
"I knew it as Obamacare," she said. "The (Covered California) commercials weren't drawing me in."
Then, she took part in a focus group and survey for the Latino community.
"They were trying to figure out how to get more Hispanics" to enroll, said González. "I wasn't the only one that was worried about how this is going to work and how we are going to afford it."
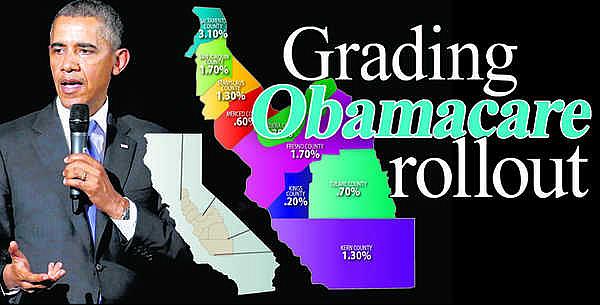
In the San Joaquín Valley, there were 250,000 residents (65,000 of them in the Fresno area) who qualify for subsidies, according to Covered California. In Sacramento, 130,000 qualify for subsidies.
González and other Latinos were included in those numbers.
According to a September 2013 analysis by Families USA, approximately 1.2 million Latinos would be eligible for subsidies through Covered California.
But, Latinos didn't know enough.
"People were afraid of the price you have to pay. We can barely afford to pay rent," González said of not knowing how pricey the premiums could be or if they qualified for any subsidies or tax credits.
A few weeks after taking part in the survey, González talked to her husband and told him, "We need to figure out how to register myself online."
González' story is one of the many scenarios that played a role in the lower-than-expected Latino enrollment in the early months.
"Even for my husband, it was kind of complicated to do it online," González said of the confusion of shopping for health insurance on the Internet.
For González, it was the face-to-face help of an enrollment counselor at Centro La Familia Advocacy Service in west Fresno that finally got her enrolled.
"It was much better. We tried to do it online, but we were not understanding how registration worked," González said of in-person enrollment.
González said the enrollment counselor explained how co-payments and deductibles work, and showed them a list of health plans that she could select.
González chose a Silver 87 HMO health plan with Kaiser Permanente. With tax credits, her monthly premium is $183.75.
In April, González received a letter from Covered California. "Our records show that you have paid your initial premium payment. Look for an enrollment packet from your health insurance plan to arrive soon," the letter said.
Early Latino enrollment disappointing
Compared to the rough start of the federal health insurance market place, Covered California had a smoother launch and the overall enrollment numbers were very encouraging for state's exchange officials.
However, Latino enrollment was lower than expected.
Covered California officials banked on language-specific outreach to boost those numbers. Sixty percent of its enrollment counselors, 13 percent of licensed insurance agents and 10 percent of its service center representatives spoke Spanish.
For Sandra García, a 58-year-old woman from Poplar in Tulare County, an informative workshop at the Tulare Community Health Clinic in Tulare provided her with information in Spanish.
"They gave a workshop on the steps to enroll, what were the requirements and what steps had to be completed and how long it would take," said García in Spanish.
Before the workshop, many of García's co-workers thought that in order to enroll in Obamacare, they had to spend all day in the process and miss work. García, who works in the fields, didn't know she could make an appointment to enroll.
Thanks to in-person enrollment, García enrolled in an Anthem Blue Cross silver plan that has a $500/$1,000 deductible. Her plan became effective on March 1.
As part of improving Latino enrollment, Covered California improved its Spanish-language website after conducting focus groups. Officials learned the "best language" was not being used.
In the state, 28.8 percent of the population speaks Spanish only.
Covered California also changed its marketing strategy in the Central Valley, adding billboards in Spanish to target immigrant communities.
Originally, Covered California was not planning on using billboards. Instead, their Latino marketing focused on social media, radio, and television ads.
"We saw the ads on television and we were scared because we didn't know how it works," said García. "We didn't know what to expect. We were confused."
Another challenge Covered California faced in the Latino community was the issue of immigration status.
In the first months of open enrollment, Covered California executive director Peter V. Lee reached out to the Latino community through Vida en el Valle and encourage "families with mixed status" to apply for health coverage.
Many Latinos feared that their personal information including their legal status would be shared with immigration officials once they are done signing up for health insurance.
Lee reiterated that information provided to Covered California was going to be used only for insurance purposes.
García said many of her acquaintances were worried that "la migra" (immigration) was going to take people away if they enrolled in Obamacare.
"At work you would hear one thing and then others would said a totally different thing," García said of the confusion in families with mixed status.
Covered California also introduced a Spanish-language enrollment application form which became available on its website at the end of December and could be printed and completed in paper form.
The form was one of the efforts to make sure Spanish-speaking consumers enrolled during the last months of open enrollment.
With the New Year, Covered California intensified efforts to reach Spanish-speaking residents with television advertising. It also mailed out 1 million informational flyers in Spanish.
García's experience shows that Covered California was on the right track to improve Latino enrollment.
Outreach, education, enrollment challenges
Covered California awarded $37 million in grants to community organizations to conduct outreach and education programs among individuals and small businesses.
The grants went to universities, nonprofits groups, health foundations, and unions.
The grants were part of the $43 million in federal funds that Covered California received for two years. The remaining $6 million will be used to expand outreach and education strategies this year.
Health advocates had said early on that outreach and enrollment for minority communities would face many challenges, especially in hard-to-reach rural areas.
Some of the challenges faced by certified educators, enrollment counselors and insurance agents included lack of information, delays of certification process, as well as technology problems.
When Mario Alfaro, a Covered California certified educator with Planned Parenthood Mar Monte in Fresno, started doing outreach and education, he tried to be visible in community colleges to get the "young invincible" educated because a large majority of students were underinsured or uninsured.
During his outreach efforts, Alfaro saw there was "lack of information in college campus." Students, he said, relied on rumors instead of facts.
Brenda Ordaz, a CHIRLA representative and a trained Covered California navigator, agreed with Alfaro about the miscommunication about the Affordable Care Act.
Another obstacle was that certification for enrollment counselors and insurance agents was time consuming.
"It took a long time for us to get our background check on time," said Josie Sánchez, program manager with Fresno Healthy Communities Access Partners of being certified as enrollment counselor for Covered California. "We couldn't help people."
Another challenge was technology.
Sánchez said it wasn't easy for many people to set up a user account with Covered California.
"For someone who is not used to computers, is not easy," Sánchez said.
Many people didn't know how to upload the required documents for online registration, she said.
"People didn't understand the plans either," said Sánchez, who spent time with clients to explain. "It wasn't easy to make a decision."
Sánchez said many were not familiar with terms such as deductibles, co-insurance, copayments, premiums, etc.
Like Sánchez, Ordaz saw that people didn't understand basic insurance terms such as deductibles, premiums or co-pay not only in the Latino community but elsewhere. That meant she and others had to educate people.
"Some of them were afraid of the health care system," said Lizeth López, Clínica Sierra Vista outreach and enrollment programs manager.
The non-profit clinic partnered with several community organizations to collaborate on ACA enrollment events in Fresno, Kern and Inyo counties.
López said the last months of open enrollment period were very busy at Sierra Vista. Enrollment counselors there completed more than 10,000 applications during open enrollment.
With a team of 45 bilingual outreach and enrollment staff, López said the biggest challenge her team faced during the open enrollment period was the malfunction of Covered California's website.
"That was the hardest," she said, adding that, when the site worked well, enrollment applications could be completed within half an hour.
The big reward, said López, was "opening the doors" to health insurance access.
Tana Elizondo, agent and co-owner of Hanford-based Central Valley Life and Health Benefits, Inc., one of the challenges was waiting for certification.
Elizondo, one of three agents in the state who have been selected to sit on the SHOP advisory committee for Covered California, believes in the mission to increase the number of uninsured California residents with health insurance.
"We are a diverse population, and many just here in the Central Valley," Elizondo said.
Legislation aims to improve future enrollment
As Covered California tried to fix problems with the state exchange, state Sen. Norma Torres, D-Pomona, introduced legislation in February to diversify the group's board of directors. Gov. Brown signed the bill, which goes into effect on Jan. 1, 2015.
"Accountability starts at the top," said Torres of the need for the bill after Covered California's initial marketing efforts aimed at Latinos floundered during the first three months of open enrollment period.
Torres was vocal about the poor job Covered California did to enroll uninsured Latinos, including Spanish-speaking uninsured as well as the younger population of uninsured people during the first months of the enrollment period.
Torres said having diversity in the board "is a step in the right direction to solving many of the problems that have created obstacles for consumers and families who are trying so hard right now to get health coverage."
The California Legislative Latino Caucus and the Latino Coalition for a Healthy California supported Torres' bill.
Xavier Morales, executive director for the Latino Coalition for a Healthy California, said Latino enrollment requires "a deep cultural understanding of the unique conditions that our community faces."
"The composition and membership of the board should reflect the needs of consumers," Torres said.
This is the first of a two-part series on the Affordable Care Act rollout in California and Latino enrollment. This article was originally published in Vida en el Valle.

