Health Series: How American Indians fit into the Affordable Care Act
S.E. Ruckman reported this story as a fellow in the 2014 National Health Journalism Fellowship, a program of the USC Annenberg School for Communication and Journalism.
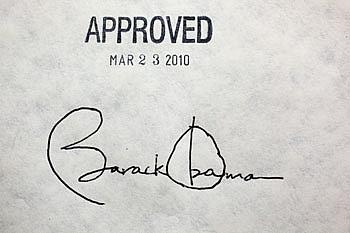
President Barack Obama's signature on the health insurance reform bill at the White House, March 23, 2010. (Official White House Photo by Chuck Kennedy)
Native Times’ special contributor, S.E. Ruckman, pitched a three-part series for a National Health Journalism project from the University of Southern California (USC)’s Annenberg School of Journalism that was initially entitled, "Obamacare in Indian Country." After working on the series, Ruckman narrowed the focus to the Affordable Care Act’s (ACA) enrollment figures and how individual Indians fit into that picture. She rounds it out by seeking the mainstream’s take on how ACA has manifested in Indian country. The following is an introduction to her multi-part series.
Finding the exact number of American Indians enrolled for federal health care insurance seemed like a natural question. One federal agency reports point out that many minorities defer from self-identifying on their Affordable Care Act (ACA) application, so totals are not an easy assumption even with numbers attached. In short, the practice of omitting race information is common across federal agencies and occurs in just over 31 applications per 100, according to a U.S. Department of Health and Human Services (HHS) report on ACA enrollment data. With this in mind, experts say that roughly 1.3 percent of federal ACA applicants were classified as “multi-racial” when race was disclosed, muddying the waters even further.
In a federally-facilitated marketplace (FFM), determining American Indian/Alaska Natives (AI/AN) ACA numbers are inexact and exclude Indians who live in state-based marketplaces in 14 states. In the federal market, Indians who enrolled in ACA markedly trail behind other minorities like Blacks, Latinos and Asians although some 2.7 million Americans identify as AI/AN in U.S. Census figures. Hawaiian/Pacific Islanders are an even smaller group and have an ACA enrollment figure of 3,282, the same report shows. Both Indian and Hawaiian ACA enrollment is below one percent of all Americans.
Zeroing in on official Indian ACA enrollment numbers (FFM or otherwise) did not divulge any extra ethnic information. Tribal diversity, for example, was a statistic that was not calculated. Numbers for the state of Oklahoma, while giving AI/AN enrollment tallies (listed at just over 1,300), did not include any insight into tribal affiliation for the state’s 38 federally recognized tribes. This is typical for Oklahoma (a non-Medicaid expansion state) since their version of “Indian country” involves varying tribal jurisdictions and allotment parcels rather than official reservations that exist in states like New Mexico, South Dakota and Arizona where reservation names can provide clues about specific cultural specificity.
During a series of tribal listening sessions conducted by health officials in Okla. during 2014 there “seems to be a misunderstanding at the federal level that all tribes are on reservations,” according to Oklahoma’s official summary on the six meetings. This is undeniably true but the prevailing perception is all Indians live on reservations, some officials said.
Across the country, Indians live urban, interwoven into different social fabrics as a result of earlier (arguably unsuccessful) federal programs that sought to familiarize Natives with the larger society. In other cases, Indians live in rural areas and are remarkably isolated even in populations where they constitute the majority of a local landscape.
Not only did the Native Times (NAT) wonder how many Indians (individuals and families) enrolled in the new health care marketplace, but it also sought what factors may hinder Indians from enrolling whether perceived (cultural) or real (income) obstacles. It soon became necessary to look at how Indian entities sought to bridge any gaps. NAT asked for input from health boards, state officials and Indians who enrolled in ACA.
One significant factor to lukewarm enrollment is the federally-funded Indian Health Service (IHS). Members of federally recognized tribes with a tribally-issued enrollment card or Certificate Degree of Indian Blood (CDIB) are eligible for health care services that are funded annually by federal monies. This creates another variable statistical wild card since many who identify as Native fail to meet tribal enrollment requirements set by any tribe. If they enroll in ACA, their cultural affiliation will be impossible to calculate.
For those with a tribal card, IHS’ imprint is indelible. For some, from the moment of birth to an end-of-life-scenario, the Indian health depository is at once a monopoly and an oligarchy. Within IHS, management, care and operations are primarily provided by Natives at the roughly 150 facilities by around 15,000 employees. This design all but ensures that most of Native peoples’ health care choices are concentric. In the instances where tribes operate their own facilities, the difference can be quantum.
The IHS healthcare umbrella operates with about $4.3 billion a year, according to agency budget figures. The Indian arm of the HHS provides free dental, radiology, laboratory, inpatient (limitability applies), outpatient, optometry and other forms of health care to Native people. With no bills that follow, its existence means that most Indians eschew traditional health insurance unless it is provided by an employer, tribal or otherwise. In some cases, Indians can be covered under provisions outlined by the Federal Employees Health Benefits Program (FEHB) under provisions of the Indian Health Care Improvement Act (IHCIA). But even that is limited for real data. In 2013, roughly 10,000 Indian tribal employees in 53 tribes participated in the health benefits program. This does not mean, however, that all 10,000 are tribally-enrolled.
Within the move to enroll Natives through the ACA, other factors exist. Indians are eligible to enroll outside of scheduled enrollment periods, have the option of not choosing ACA and may qualify for federal credits that make their health plan premiums affordable. But marketing a new health initiative to a susceptible population could be best characterized as hit or miss. What works in rural areas may not work in urban areas while overall income and a basic mistrust of the federal government looms large.
This series will look for the real total of American Indians enrolled in ACA and how various regions across Indian country sold the new health initiative to their Native people. What became clear is that outreaches either worked or federal guidelines worked against potential enrollees. What started as a quest for ACA’s Indian numbers morphed into feeling out the new health initiative through Native eyes.
This article was originally published on Native American Times

