In Mississippi’s fractured mental health system, it’s the haves vs. the have-nots
Data: Center for Population Studies at University of Mississippi/ Graphics: Katherine Mitchell, Mississippi Center for Investigative Reporting
By Shirley L. Smith
Mississippi Center for Investigative Reporting
Mississippi’s poorly constructed mental health system gives mental health providers insufficient funds to provide court-ordered, community-based services, and a poorly conceived Medicaid system cuts into their revenue stream, said Richard Duggin, chief executive officer of Region 7 Community Counseling Services center in West Point.
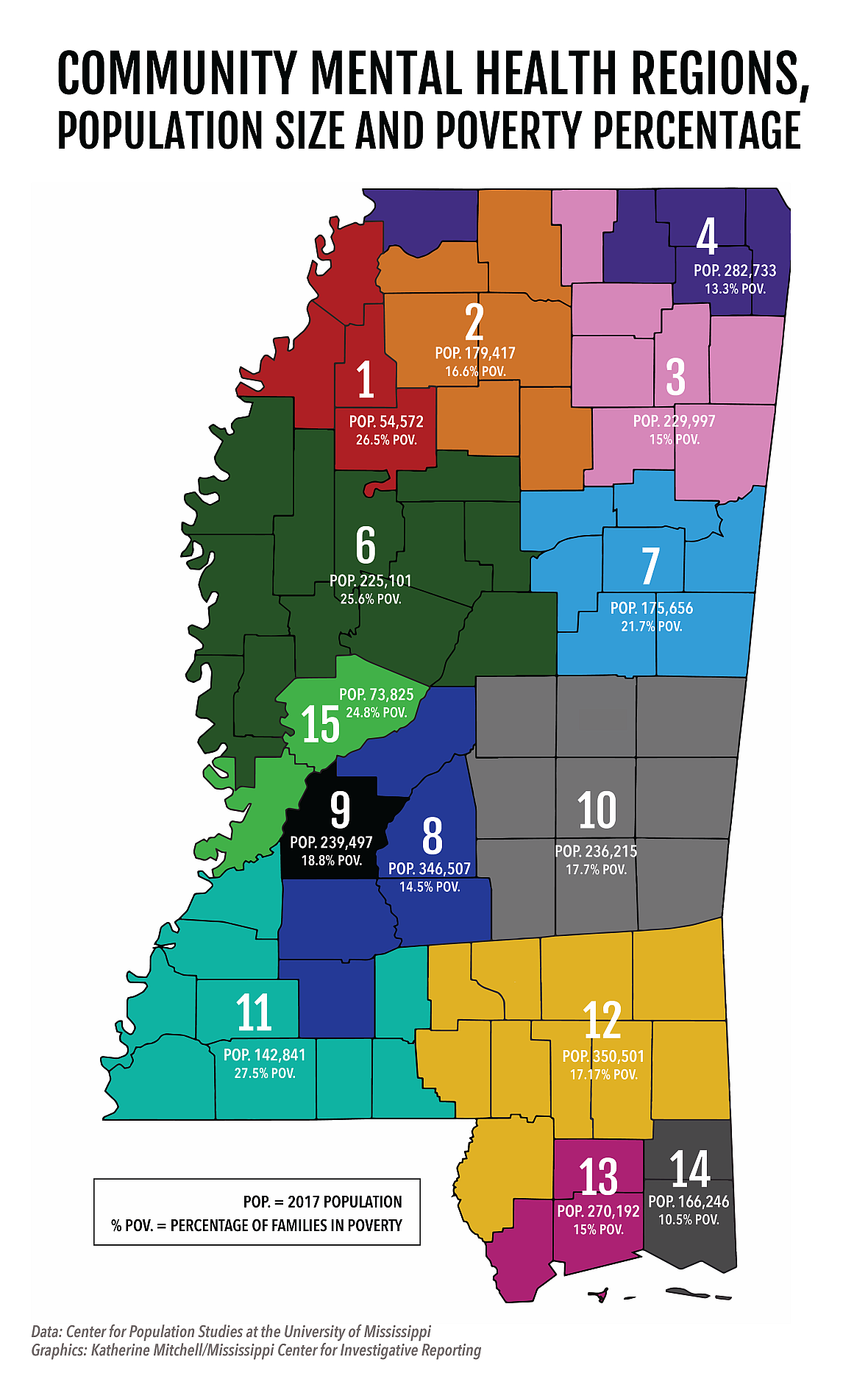
“Not all community health centers get funding for (crisis-diversion services), partly because of the inequities in the funding provided by the counties they serve,” Duggin added. In his seven-county regional Community Mental Health Center in northeast Mississippi, more than a fifth of families – and a third in one county alone (Noxubee) -- live in poverty.
Mississippi’s Legislature delegated the responsibility of providing community-based mental health services to 14 independent regional Community Mental Health Centers. A 15th center – Region 5 – closed over financial troubles.
Last year, the centers provided over $33 million in uncompensated indigent services to underinsured and uninsured individuals, said Phaedre Cole, president of the Mississippi Association of Community Mental Health Centers.
Officials at several community centers said revenue shortfalls and disparity in government funding from a fragmented mental health system, along with limited resources in the state’s rural areas, is making it difficult for some centers to remain viable and provide much-need mental health services.
The fallout from this has been devastating.
A significant number of Mississippians with mental illness are cycling through jails, emergency rooms and psychiatric hospitals because the treatment and support services they need at the community level to manage their illness do not exist or they are insufficient.
And the lack of adequate community-based services is also costing the government more money.
“The most expensive ways to deal with mental health are emergency departments, inpatient hospitalization and the criminal justice system including using the police as first responders. So, if you can keep people from repeating that cycle, it saves the state and county money and it makes for healthier communities,” said Debbie Plotnick, Mental Health America’s vice president for mental health and systems advocacy.
Plotnick said it can take eight to 10 years for people who developed a mental illness in childhood to get a proper diagnosis. As a result, their condition worsens, making it hard for them to finish school or maintain employment, so by the time they reach adulthood they are not only poor but disabled, and they qualify for Medicaid.
Mental illness does not just affect those with the disease, “it destroys families,” said Jackson psychiatrist Dr. Marshall Belaga. “You have more divorces and abuse, and children cannot learn as well if they are in an unstable environment.”
“If you address the issues before people are repeating these expensive cycles and before they become disabled, they are less likely to need public benefits, because they continue working and going to school,” Plotnick said.
This requires having an adequate infrastructure in the community to provide individuals with treatment and support before they reach a Stage 4 crisis that can be detrimental to their life and lead to hospitalization, incarceration and homelessness, she said.
Disability advocates say Region 8 Mental Health Services community center, located in the metro area, provides such an infrastructure. It has managed to keep innocent people with mental illness out of jail, and it is a model of what can be done with adequate funding, resources and intervention services.
Region 8 implemented a Crisis Intervention and Diversion program in partnership with local private hospitals, law enforcement agencies, the courts and jails to ensure no individual in the region is held in jail solely because of a mental health issue, said Emile Craig, the region’s director of administration, in a statement. He said Region 8 also trains law enforcement officers and other community partners on how to interact with people with mental illness.
“Since we started the program in 1998, not a single individual in any of our five counties has been held in jail for a mental health issue,” Craig said.
The crisis services are just one component of Region 8’s success in helping people receive care in the least restrictive environment, the other is the coordination between Region 8 and all of its inpatient and outpatient services, he said.
Region 8 serves 18,000 people and includes two of the wealthiest and fastest-growing counties in the state – Madison and Rankin.
Unlike some counties, Region 8 has the benefit of having a Crisis Stabilization Unit, a short-term, inpatient acute care facility that stabilizes people in crisis, said Dave Van, Region 8’s executive director. “We also have local contracts with private acute care facilities for the placement of individuals that are determined to be mentally ill if our Crisis Stabilization Unit is full.” He said some counties also do not have private facilities that provide acute psychiatric care.
One of the main reasons people have a mental health crisis is because they do not comply with their medication or they are uninsured or underinsured and cannot afford their medication, Craig said. “Region 8 works with pharmaceutical companies and local pharmacies to help ensure that each individual we serve is able to obtain needed medications regardless of their financial resources or access to adequate health insurance coverage.”
Angela Ladner, executive director of the Mississippi Psychiatric Association, said, “Region 8 is offering more than the required core services, and I think they are doing a nice job presently. It’s what all the mental health centers should do.”
Providers at other community centers are just as dedicated, she said, but until they get appropriate funding, they will not be able to provide the same level of services as Region 8.
The issue is the inconsistency in care
Mississippi’s Department of Mental Health disburses state and federal grants to the community centers, but they must apply for them. The centers also receive funding from the counties within their region. Some centers may have other sources of revenues like private grants and donations, Cole said.
"Generally speaking, I believe each (community center) does a great job of providing services,” Cole said in a statement. “Each of us has our own unique, local challenges and advantages in addition to the challenges inherent to a rural, impoverished state such as Mississippi, (for example) general lack of health insurance coverage, spotty public transportation and a shortage of mental health professionals.”
Seventy percent of the community centers’ revenues come from Medicaid, private insurers and out-of-pocket payments from clients, said Cole, who is also the executive director of Life Help in Region 6, which serves 12 counties nestled primarily in the Delta, one of the poorest and most rural regions in Mississippi.
Micah Dutro, legal director of Disability Rights Mississippi, said he also believes the centers generally provide good care. The issue is the inconsistency in care.
That issue was at the core of a Sept. 3, ruling against the state by U.S. District Court Judge Carlton Reeves. He found that Mississippi has been unnecessarily institutionalizing thousands of people in psychiatric hospitals who could have obtained treatment in the community, but the state’s community-based services are inadequate. Reeves ordered state officials to work with a special master – a person appointed by the court to make sure judicial orders are followed – to expedite and prioritize community-based care.
Officials at several community centers located in the rural, less populated, economically distressed areas of the state, say they do the best they can with the resources they have available.
“We can’t provide more services without funding,” said Duggin, whose Region 7 is in a mostly rural area.
‘Whole new level of complexity’ affects client care
In 2011, Mississippi’s Division of Medicaid implemented a managed care program giving several private insurers the authority to manage reimbursement claims. Duggin and other providers say the managed care program often refuses to pay for certain necessary services.
For instance, the Day Treatment Service in Mississippi is not an inpatient program as it is in other states, said Sandy Rogers, the executive director of Communicare in Region 2, which serves 13,000 people in six rural counties, but Medicaid and the managed care companies often refuse to pay for this service, because they say that people do not need this level of inpatient care.
Matt Westerfield, the director of communication for the Mississippi Division of Medicaid, said Medicaid will not pay for certain services like Day Treatment if it is provided on the same day as another service that Medicaid deems as duplicative.
“The mental health care system was already overly complex before the managed care program was instituted, and the managed care program added a whole new level of complexity that affected client care,” Duggin said.
Last year, the community centers served over 110,000 Mississippians, according to the centers’ association 2018 Economic Impact Statement.
Most of the people served by the community centers are poor or have low incomes, and they either have insurance through Medicaid or they are uninsured because they do not qualify for Medicaid, Dutro said.
The state can solve this problem by expanding Medicaid to allow more people to obtain insurance and increasing reimbursement rates, he said.
“Medicaid is 72.6 percent of our revenue,” Duggin said. Additionally, he said, “We spent $3.1 million in 2018 in indigent services to children, youth and families who could not afford mental health treatment services or supports.”
The Warren Yazoo Behavioral Health center in Region 15, located in west central Mississippi, also absorbs the cost of people with no insurance. “We provided over $980,000 worth of uncompensated indigent services last year to adults, children and youth,” said Bobby Barton, executive director of Region 15, which served 3,600 people in 2018. He said the region provides services regardless of people’s ability to pay, “but now it’s starting to hurt.”
“The main thing is we would like sufficient funds to reimburse us for all the indigent services we provide,” Barton said.
Region 2’s other major challenges are its geographic location, getting clients to appointments because many lack transportation and a dearth of psychiatrists, Rogers said.
Medicaid provides non-emergency transportation, but Rogers said it is not dependable and “readily available in all areas in our region.” Although she said Region 2 provides in-home services for people who do not have transportation, this service puts a strain on their operation, because they are short-staffed, and it consumes a lot of manpower hours. If Medicaid would reimburse for mileage, that would help defray the cost, Rogers said.
To help fill the void left by a shortage of psychiatrists in the region, Rogers said they use psychiatric nurse practitioners.
In 2017, the American Medical Association Master File/MMS reported that Mississippi has the second lowest number of psychiatrists in the country with 4.86 psychiatrists per 100,000 people compared to the national average of 9.35.
Dr. John Mitchell, director of the Office of Mississippi Physician Workforce, said the relatively few psychiatrists in the state are concentrated in the metro area where Region 8 is based.
The Physician Workforce is working with the DMH to develop a psychiatry residency program at Mississippi State Hospital to increase the number of psychiatrists in the state. “Statistics have shown that people stay within a 50- to 100-mile radius of where they did their residency. So, if you train more, you have the potential to retain more,” Mitchell said.
‘Bad rap’ or well-intended system ‘gone awry’?
Under pressure from the federal government, the state increased its community-based services over the past few years, but Judge Reeves said, Mississippi still “operates a system that unlawfully discriminates against persons with serious mental illness.”
DMH expanded its mobile service teams known as PACT from two in 2014 to 10 in 2018. These teams provide ongoing intervention services to people with serious mental illnesses, but the rural areas cannot sustain PACT teams because of their limited workforce. DMH officials said in fiscal year 2020, that began July 1, the DMH will be providing funding for the same kind of direct mobile service in Regions 1, 2, 7, 11 and 14 through a new program called ICORT, Intensive Community Outreach and Recovery Teams. Like PACT, these teams operate 24-hours a day and go directly to clients, but they require less staff. The DMH piloted the ICORT program in Region 2 in October 2018.
Joy Hogge, executive director of the Mississippi-based Families as Allies disability advocacy organization, says parity in the state’s mental health system can only be achieved by building a better infrastructure that will offer more support, training and backup technical assistance to the community centers, and allow them to share electronic health records and track the services that each center offers.
Jackson psychiatrist Belaga, who recently retired from St. Dominic Hospital after 10 years and joined Hinds Behavioral Health Services in Region 9, also says a statewide electronic medical record system is necessary to keep track of patients and ensure that they do not fall through the cracks.
Belaga explained that if someone experiencing a mental health crisis goes to the emergency room or is brought there by a law enforcement officer or a loved one, the doctor cannot check to see if the person has received treatment at a Community Mental Health Center, because medical records between the centers and the hospitals are not shared. Consequently, doctors at the hospital cannot develop “a cohesive treatment plan,” he said.
“I have seen people coming to the emergency room 18 times for the same psychiatric complaint,” Belaga said.
If the DMH developed a statewide electronic medical records system, he said, it would allow emergency room doctors to access patients’ medical histories, see what medications they are on and contact their regional community center to get them connected with the support services they need to help them remain stable and avoid hospitalization and future crises.
Van from Region 8, who has been in the mental health field for 30 years, said, “Our out-patient community mental health system in the state of Mississippi may be somewhat fragmented, but for the most part, I think the system is getting a bad rap.”
Van said the mental health system was created with good intentions by legislators in the mid-1970s to give local officials and residents the authority to determine the best way to address the specific needs of their community.
Ladner said the design of the system was well-intended, but it has gone awry.
“I would correlate the current mental health system to charting a course to a destination, but not providing everyone with a map on how to get there, but we still expect you to get there, but not everybody will make it,” Ladner said.
Report for America corps member Shirley L. Smith is an investigative reporter for the Mississippi Center for Investigative Reporting, a nonprofit news organization that seeks to hold public officials accountable and empower citizens in their communities.
Email her at Shirley.Smith.MCIR@gmail.com.

