Treatments of physical and mental health are coming together
Los Angeles Times staff writer Anna Gorman reported aspects of this story while participating in the 2012 National Health Journalism Fellowship, a program of USC's Annenberg School of Journalism. Other stories include:
Medical clinic workers struggle with burnout
Diabetes is a stubborn adversary
Crucial Test for an Outpost of Healthcare in South L.A.
Healthcare crisis: Not enough specialists for the poor
How a 'million-dollar patient' got off a medical merry-go-round
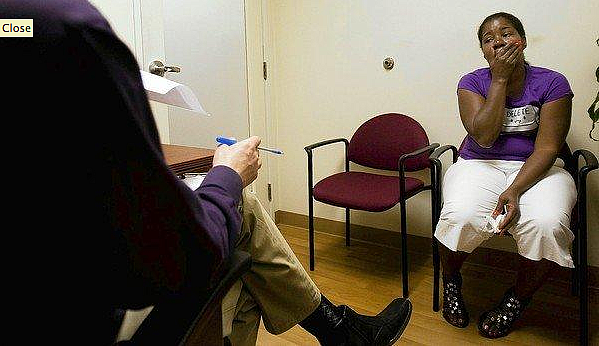
A patient talks about her depression to therapist Neil Martin at T.H.E. Clinic in South Los Angeles. “It’s so linked, physical and mental health,” Martin said. (Gina Ferazzi, Los Angeles Times)
Many days, the sheer weight of Iszurette Hunter's clinical depression becomes more than she can lift. She clings to her bed in her South Los Angeles home. Important obligations slide away, including keeping appointments with doctors who are trying to control her asthma and high blood pressure.
"I don't have no desire," she explains.
As the nation seeks to extend healthcare coverage to millions of new and in many cases chronically ill patients, one of the great parallel challenges to controlling costs and improving delivery of care will be managing the mental health problems of people like Hunter.
Already, about 2 million patients a year receiving care at government-subsidized community health centers also must be treated for depression, anxiety and other mental conditions, according to the National Assn. of Community Health Centers.
Officials expect many newly insured patients arriving at doctor's offices and urban and rural clinics to have mental health complications. Beginning next year, some 2.3 million additional people may require mental health services through Medicaid, the public health insurance program for the poor, according to a study published in the American Journal of Psychiatry. Failing to diagnose and treat mental problems early can lead to far costlier visits to emergency rooms and hospitals later.
"People who are depressed or anxious or having other problems are less likely to get preventative or other primary care," said Roderick Shaner, medical director of Los Angeles County's Department of Mental Health. "Their illnesses become greater in acuity before they are seen."
Traditionally, primary care doctors and mental health practitioners have tended to treat the same patients with little coordination, experts say. Now, driven by the federal healthcare overhaul, officials in L.A. County and around the nation are confronting the financial and health consequences of poor collaboration.
County health departments are training physicians to better identify depression and other mental health problems. Doctors and therapists are sharing more information with each other about their patients. And health centers like To Help Everyone, or T.H.E., Clinic, where Hunter is treated, are expanding their mental health services.
The Affordable Care Act also expands mental health benefits and requires new health insurance plans to require depression screenings. During a speech last week, President Obama said improving diagnosis and treatment for people with mental illness is essential.
"It's not enough to help more Americans seek treatment," he said. "We also have to make sure that the treatment is there when they're ready to seek it."
In a small exam room at the South Los Angeles clinic one afternoon, Manuel Mares told the doctor his head was pounding, he felt dizzy and he had been vomiting. The previous month, Mares said, he had been to the emergency room three times with similar symptoms. Doctors there performed various exams but found nothing physically wrong. Mares said they diagnosed him with anxiety and prescribed medication.
Fidgeting and talking fast, Mares, 47, said he felt desperate. He hadn't worked in a year because of a shoulder injury. His wife had recently had surgery and his son's asthma was flaring up. "It's like when you begin to put water in an empty cup and you put drop by drop in the cup until there is no more capacity," he said. "There has to be a limit."
Many of the clinic's patients have depression, which can cause symptoms such as headaches and cramps. They find it difficult to overcome because of other pressures such as getting a job, buying food and finding a place to live, Martin said. "Their problems are multifaceted," he said. "It's so linked, physical and mental health."
Martin says he tries to break the cycle of despair by identifying his patients' most pressing problem and working toward a solution.
That's crucial to keeping patients healthy and reducing demands on the most expensive parts of the healthcare system, officials say. "When you are depressed, your pain is worse," said Derrick Butler, associate medical director at T.H.E. Clinic. "When your pain is worse, you're more depressed."
Around the U.S., doctors and nurse practitioners typically spend just 15 minutes with patients — scarcely enough time to assess immediate physical ailments, let alone mental health issues, said John Bartlett, a senior advisor in the mental health program at the Carter Center.
"It's a huge unrecognized problem," Bartlett said. "And it really makes them continue to suffer.... Their medical conditions just don't get better."
At T.H.E. Clinic, having a therapist available means staff members can compare notes on patients' physical and mental health, and counseling can begin more quickly, said nurse practitioner Sandeep Lehil. "If you send them somewhere else, you never know if they are going to follow up," she said.
One of Martin's patients, Robert Brown, 52, is homeless and sleeping at a shelter. He sees a doctor for his diabetes and glaucoma and also suffers from depression and bipolar disorder. Brown recalled he was a "wreck" when he first came to the clinic and felt like walking in front of a bus. After counseling sessions and medication, he told Martin during a recent visit, "I won't say I'm happy, but I'm content."
On a Friday morning, a new patient, Cindy Ayers, 56, visited Martin. She had been referred after a medical visit the previous week. Her foot tapped nervously.
"Cindy, how can I help you?" Martin asked.
She was a heroin addict, Ayers said, and had been sober for years. Recently she relapsed and was hospitalized. She was feeling anxious.
After Ayers completed a written assessment, Martin said, "Your anxiety level is very high, and your depression level is high." Martin asked whether she was feeling suicidal. Ayers shook her head no.
"I want you to promise me you're not going to do that," he said.
"No, sir. I promise. I want to be alive.... I just want to be normal."
"We're here for you," Martin said. "One day at a time."

