Washington state is missing chances to find deadly birth defect’s cause
JoNel Aleccia, a health reporter for The Seattle Times, reported this story as a project for the Dennis A. Hunt Fund for Health Journalism and the National Health Journalism Fellowship, programs of USC Annenberg’s Center for Health Journalism.
Other stories in the series include:
FDA agrees to review folic acid for corn flour to halt birth defects
Wash. state to tell families about genetic studies of fatal birth defects
State changing vitamin rule in wake of birth-defects probe
FDA weighs adding folic acid to corn masa to halt birth defects
Flawed tracking may mask birth-defect clusters across U.S.
FDA’s ‘terrible policy error’ blocks simple step to prevent fatal birth defects

Sally Garcia hugs her daughter Josefina, who was born healthy. Her first daughter, Maria, died in 2012, part of a cluster of babies with birth defects. Hispanic women, at greater risk for having babies with neural-tube defects, make up 60 percent of local cases. (Erika Schultz / The Seattle Times)
[Click here to read the Spanish version.]
Sally Garcia still doesn’t know what went wrong with her baby.
“I hoped that when she was born she would be perfect and nothing would be wrong,” recalled Garcia, 26, of Prosser, about an hour outside of Yakima. “They pulled her out and my mom started to cry. That’s how I knew she wasn’t OK.”
Dark-haired and dark-eyed, Maria Rosario Perez lived 55 minutes that Friday afternoon before she died of complications of anencephaly, a rare and fatal birth defect. A nurse had just enough time to make casts of the baby’s hands and feet so the family would have something to keep.
About two in every 10,000 babies in the U.S. are born with anencephaly each year. It occurs when the neural tube, which forms the brain and spinal cord, fails to close early in pregnancy.
What happened to Maria was a rare tragedy, a fluke, doctors said.
But records show at least 40 other mothers have lost babies to the disorder in Yakima, Benton and Franklin counties since 2010 — a rate as much as five times higher than the national average.
State and federal health officials have been trying for two years, without success, to identify what’s behind one of the largest documented clusters of anencephaly in U.S. history. A lack of folic acid, a B vitamin, raises the risk, and anencephaly is generally more common in Hispanic women, but exactly why the rate is so high in Central Washington has confounded state experts.
“It’s a high priority for our department,” said Dr. Kathy Lofy, Washington’s health officer.
But a Seattle Times investigation finds that even as cases continued to climb, health officials tasked with solving the mystery may have missed opportunities for answers.
And, as the government review of the cluster moved forward, state Medicaid officials didn’t change rules that limited women’s access to free folic-acid supplements, including in the three affected counties, where up to 80 percent of births are paid for by the state.
Outside experts said the probe underscores both the difficulty of investigating birth-defect clusters, which are rarely unraveled, and the need for vigorous effort.
“I judge that it will be unlikely that we’ll find anything that will be compelling — and I think we need to give it a try,” said Peter Langlois, a senior epidemiologist for the Texas Birth Defects Registry, who is advising Washington officials.
The interviews, tests and outreach aren’t required, but all are included in standard protocol developed by researchers from the Centers for Disease Control and Prevention (CDC).
“It breaks my heart that there’s not been more productivity,” Allison Ashley-Koch, a professor of medicine and biostatistics at Duke University, said of the investigation. She is compiling the largest genetic study of anencephaly in the world and has followed the Washington cluster.
Two years ago, Ashley-Koch said, she and her colleagues contacted CDC officials, offering to help collect biological samples and analyze potential environmental contaminants. Such analysis could offer insight into the disorder.
“Basically, they just said, ‘Thank you, but no thank you,’ ” Ashley-Koch said. “If we don’t get in there and start collecting some samples — whether it’s my group or the CDC — I just feel like it’s an opportunity missed if we don’t learn from this.”
Sally Garcia keeps casts of Maria’s hands and feet. Prosser funeral director Carlen Majnarich said she buried several babies with anencephaly this year. “It’s very hard,” she said. “All of those lost hopes for a child.” (Erika Schultz / The Seattle Times)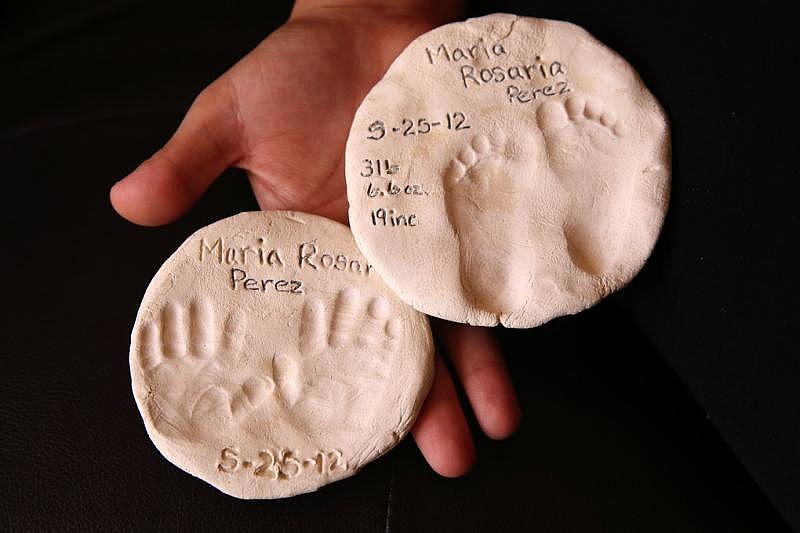
CDC officials and Cathy Wasserman, the state epidemiologist in charge of the investigation, said they don’t recall Ashley-Koch’s offer. But Wasserman said state officials have relied on a panel of experts and pursued every avenue deemed important.
“I think we’ve been pretty diligent on this issue,” she said. “We’re trying to be thorough in responding to community concerns. It’s kind of going as I would expect it to go.”
Still, more than three years after her baby died, Sally Garcia has no answers.
“Something’s going on and someone needs to tell us,” said Garcia, who shares a crowded apartment with her husband, Santiago Acosta, 30, an agricultural worker, and her three children, Calvin, 8; Daniel, 2; and Josefina, 10 months.
“I would like for them to actually take the time and find out what’s going on.”
A nurse sounds alarm
Washington’s cluster was discovered after a nurse, Sara Barron, noted in 2012 that two babies with anencephaly were born within weeks of each other at the 25-bed community hospital in Prosser, PMH Medical Center.
“They lived only hours and the devastation felt by the parents as well as the staff in our small facility was palpable,” Barron, 59, now a nursing instructor at Washington State University, recalled in a pending paper. “I could hardly believe it when the delivering doctor said another patient was expecting the same outcome.”
Dr. Lisa Galbraith was one of the doctors. As a medical resident in Southern California, she had delivered 1,000 babies, and only one with anencephaly. In Prosser, the obstetrician oversaw care of Garcia’s pregnancy and others affected by the disorder, including some that ended in miscarriage, or were terminated.
“I had a total of four or five babies with anencephaly over the course of two years,” recalled Galbraith, 42.
Garcia learned of her baby’s birth defect after an ultrasound. Another doctor, not Galbraith, advised her to abort the pregnancy, but Garcia refused.
“I always had hope,” she said.
Disturbed by the spike, Barron notified state health officials, who reviewed birth records and found nearly two dozen cases in the three-county area in the previous three years.
The CDC launched a study that examined medical records of 27 women, including Garcia, who had babies with neural-tube defects in the counties from 2010 to 2013. Their records were compared with those of 108 women with healthy pregnancies. The analysis showed the rate of spina bifida, one type of defect, was far lower than the national average, but the rate of anencephaly was much higher.
Dr. Lisa Galbraith, an obstetrician, cared for Sally Garcia. As a medical resident in California, Galbraith delivered 1,000 babies, only one with anencephaly. In Central Washington, she saw four or five cases in two years. (Erika Schultz / The Seattle Times)
That’s where the study stopped. No women were interviewed — or told they were among dozens in the region who’d lost babies to a rare birth defect. At the time, CDC officials said they lacked funding for a “boots on the ground” epidemiological study.
State makes a pledge
With the rate still rising, Washington state health officials launched an investigation in June 2014, tapping a 16-member advisory panel of medical experts, researchers and community members. The group pledged to find ways to reduce the number of cases, improve reporting and determine whether more investigation was necessary to find the cause — or causes.
“Everyone is doing what they can and more,” said Dr. Christopher Spitters, a panel member and health officer for the Yakima Health District. “The inability to pinpoint one or more culprits certainly is not for lack of trying.”
Washington health officials have analyzed existing reports on contaminants such as nitrate levels in drinking water and pesticide use in agriculture, and considered whether there could be genetic markers for women more likely to have babies with neural-tube defects. But they have collected no blood samples, performed no genetic tests and conducted no examination of water, soil or pesticide levels in the region — and have no plans to do so.
The advisory committee has agreed with Wasserman’s conclusion that further tests aren’t warranted by existing evidence. “We are a state health organization; we are not a research organization,” Wasserman said.
Ashley-Koch and other experts countered that collecting and analyzing samples, particularly of new cases as they occur, would be vital to identifying any common exposure.
In January, state officials began interviewing mothers of infants with neural-tube defects, including spina bifida. So far, they’ve interviewed 15 women, including 11 of the 41 women who lost babies to anencephaly, Wasserman said. Seven more potential interviews have been identified since April, including three mothers of babies with anencephaly, but health officials are still following up, she said.
They will compare the answers with those from healthy control-group members, according to CDC protocol. Results should be available by spring.
“I think that there is an urgency,” Wasserman said. “I don’t think the time it’s taking is unusual.”
Experts in birth defects, epidemiology and health communication say the problem may not be with what health officials have done — but what they haven’t done.
“I would suggest that there seems to be a gap in the research so far,” said Linda Neuhauser, a clinical professor at the University of California, Berkeley, School of Public Health, who specializes in community-health interventions. “They haven’t actually gone in and interviewed (all) the people yet … Because if you don’t have that, you don’t have some windows into possible causes.”
Sally Garcia, who is eager to share her story to help others, said she’s disappointed at not being contacted.
“Nobody has actually talked to me,” she said.
The omission is by design. State officials plan to talk only to women with due dates within two years of fall 2014 in order to include them in the study. That method excludes Garcia, whose daughter was born in spring 2012.
Women pregnant a few years ago might not recall the information solicited in the survey, such as the foods they ate, the medications they took and other details, Wasserman said. Because their comments might not be accurate, they could skew the study results, a view supported by a poll of the advisory committee.
“They didn’t feel that we should go back and try to get interviews,” Wasserman said. “This was a decision that was made by the group.”
But with 41 women involved, the experience of each one is potentially valuable, said Dr. Lowell E. Sever, a retired CDC birth-defects expert who has studied neural-tube defects in Washington state.
“Interview everyone you can get your hands on,” said Sever. “You can have information that’s valuable, even if it’s not scientifically valid.”
Even those who fall within the study limits may be missed. Researchers get women’s names and phone numbers from health-care providers, then send letters to the last known addresses. But in some cases, the women are difficult to find.
If researchers call 10 times and get no answer, they’ll stop trying, Wasserman said. Other ways to reach the women, including email, social media and home visits, have not been pursued.
Outreach workers unaware of effort
With no known cause for the cluster, health officials are focusing on raising awareness about the importance of women taking folic acid before pregnancy. Wasserman points to updated websites, “blast fax” messages to health-care providers, and presentations about the cluster to area hospitals, health conferences and state meetings.
The state ran 3,000 public-service radio spots about folic acid between May and July this year and distributed 12,000 brochures to community colleges, clinics, nail and hair salons, and other sites, she said. They held public forums in Sunnyside and Kennewick in 2014, and plan to give out more materials at obstetric and primary-care conferences next year.
In addition, county health officials have worked with the nonprofit group Vitamin Angels to obtain 5,670 bottles of free folic-acid supplements for women served by the Yakima and Benton-Franklin health districts — but also the Moses Lake Community Health Center, 100 miles from the cluster region.
“I think we’ve been really responsive to the community,” Wasserman said. “We’ve been able to get out the prevention messages about the one thing we know that can prevent neural-tube defects, which is folic-acid supplementation.”
It’s not clear, however, whether health workers and their clients have gotten the message.
The 2014 Sunnyside forum, for instance, was attended by about two dozen people — and local residents were outnumbered by health-care advocates and members of the media.
In March, a member of the advisory panel said community health workers in the three counties were “poised and ready to help,” but had “not seen anything regarding materials around this topic,” according to meeting minutes.
In April, members of the Washington State Democratic Central Committee demanded a “more thorough” investigation in a resolution sent to the state health department, saying, in part, that a folic-acid awareness effort was “not noticeable.”
In June, when Dr. Jennie McLaurin, an expert in migrant and community health, gave a talk in Yakima, she found little evidence of intervention. “The outreach workers there were unaware of any efforts,” said McLaurin, a former advisory-panel member.
And while county officials obtained some free folic-acid supplements, state Medicaid officials have been limiting coverage for the vitamins that can prevent neural-tube defects. Under Washington law, the state’s Apple Health Medicaid plan covers the vitamins only after a woman is pregnant — too late to prevent neural-tube disorders, including anencephaly.
Groups such as the March of Dimes first raised the issue a year ago. But the state Health Care Authority, which oversees Medicaid, said last month it was considering a change only after inquiries by The Seattle Times.
“We just held her”
For the families affected by the rare birth defect, their private tragedies are far more than a public health debate.
Steve and Valerie Branch, of Yakima, had never heard of anencephaly until an ultrasound revealed devastating problems with their unborn daughter in the fall of 2012.
“It sort of took our breath away,” said Steve Branch, 32, a compliance officer with a local fruit-packing firm. “It was a lot to try to process. I was just confused.”
The couple, who already had two young children, struggled with the news. From the start, though, they never thought of terminating the pregnancy.
The Branch family keeps mementos — a bracelet, a dress, a snip of hair — from their daughter Gianna’s short life. Steve Branch said he wishes the cluster were a “higher priority” for the state. (Erika Schultz / The Seattle Times)
“It was still our child. I could feel it moving,” said Valerie Branch, 33, who works as an administrator for a group of doctors opposed to assisted suicide.
Gianna Jessie Branch was born Jan. 25, 2013. She lived five hours, long enough for family and friends to say hello — and goodbye.
“My mom got a little dress and we just held her,” Valerie Branch recalled. “She still looked like what our other kids looked like.”
The couple learned from news reports, not state health officials, that Gianna’s death may have been part of a larger problem, Steve Branch said.
State health staff interviewed Valerie Branch this year. Beyond that, however, the couple has heard nothing.
When the Branches decided to have another child, a boy born in September, the lack of information complicated the decision, they said. Tests confirmed early the child was healthy, but Steve Branch said he worries about other families.
“It seems like it should be a higher priority,” he said. “If nothing else, I would like to see more discussion, more transparency for the families going through this.”
As the anencephaly cluster has grown, so have worries in the wider community. Dr. Portia Jones said she has fielded increasing questions about the birth defects at her family practice at Community Health of Central Washington in Yakima.
“I would say that probably a third of women who are contemplating pregnancy either know someone or have heard of someone affected by the cluster,” she said.
“Smoking guns” hard to find
No one disputes that investigating a birth-defects cluster is difficult, and often futile. It’s challenging to collect the data and even tougher to prove a cause, said Sever, the retired CDC birth-defects expert who lives in Seattle.
“The problem with birth defects is that, with very few exceptions, there are no smoking guns,” said Sever.
Those exceptions, though, have been significant: the discovery of the link between the anti-nausea drug thalidomide and limb malformations in babies in the 1960s, or the tie discovered in 1999 between a common antibiotic, erythromycin, and a condition in newborns called hypertrophic pyloric stenosis that causes forceful vomiting and can lead to serious complications.
Sever first reported high rates of anencephaly in Benton and Franklin counties in a 1988 paper that explored possible links with the nearby Hanford nuclear site, but found none.
“What the community has now is a cluster superimposed on higher background rates,” he said.
Even such spikes can be tough to figure out, and health officials can be reluctant to invest the resources. Washington officials said they haven’t tallied the costs of the investigation so far.
One notable exception was in Texas, where a cluster of three anencephaly cases within 36 hours at a Brownsville hospital in 1991, followed by more, prompted immediate public and political action that led to the Texas Birth Defects Act of 1993 and the state’s robust birth-defects registry, which tracks anomalies.
Years of research there yielded no clear cause. But scientists did find the problem could be traced, in part, to the lack of folic acid in the diets of the mostly Hispanic women. Obesity and diabetes appeared to be factors, as did exposure to grain molds.
Langlois, the Texas epidemiologist who is on the Washington panel, has looked into 120 clusters over two decades. So far, Washington’s effort “feels like the normal course of an investigation,” he said.
But experts like Sever and Ashley-Koch said state officials should consider partnering with researchers already working on the problem to help contact families and gather valuable data.
Every two weeks, Sally Garcia buys fresh flowers at the local Food Depot to take to her daughter’s grave. (Erika Schultz / The Seattle Times)
“For some of our families, that’s one of the greatest comforts they get,” Ashley-Koch said. “They don’t have the luxury of having their child with them, but the fact that they participate in research makes them feel like the child’s life was meaningful.”
Finally, state lawmakers should be encouraged to take the problem seriously, the experts said. In Texas, just three babies with anencephaly sparked enough outrage to overhaul the state’s birth-defects reporting system. In Washington, with one of the largest documented clusters in the nation, the budget for birth-defects surveillance is just $275,000, and that includes $200,000 shifted from other health-department accounts, Wasserman said.
Lawmakers at the local, state and federal levels did not return requests seeking comment about the problem.
“I think the state of Washington over time has taken a hands-off position to birth defects,” said Sever. “Without political will, nothing gets done.”
[This story was originally published by The Seattle Times.]
Photographs by Erika Schultz/The Seattle Times.

