When Profit-Driven Clinics Kick “Noncompliant” Patients off Dialysis, Is Anybody Watching?
This story was originally published by Mother Jones with support from our 2023 National Fellowship.
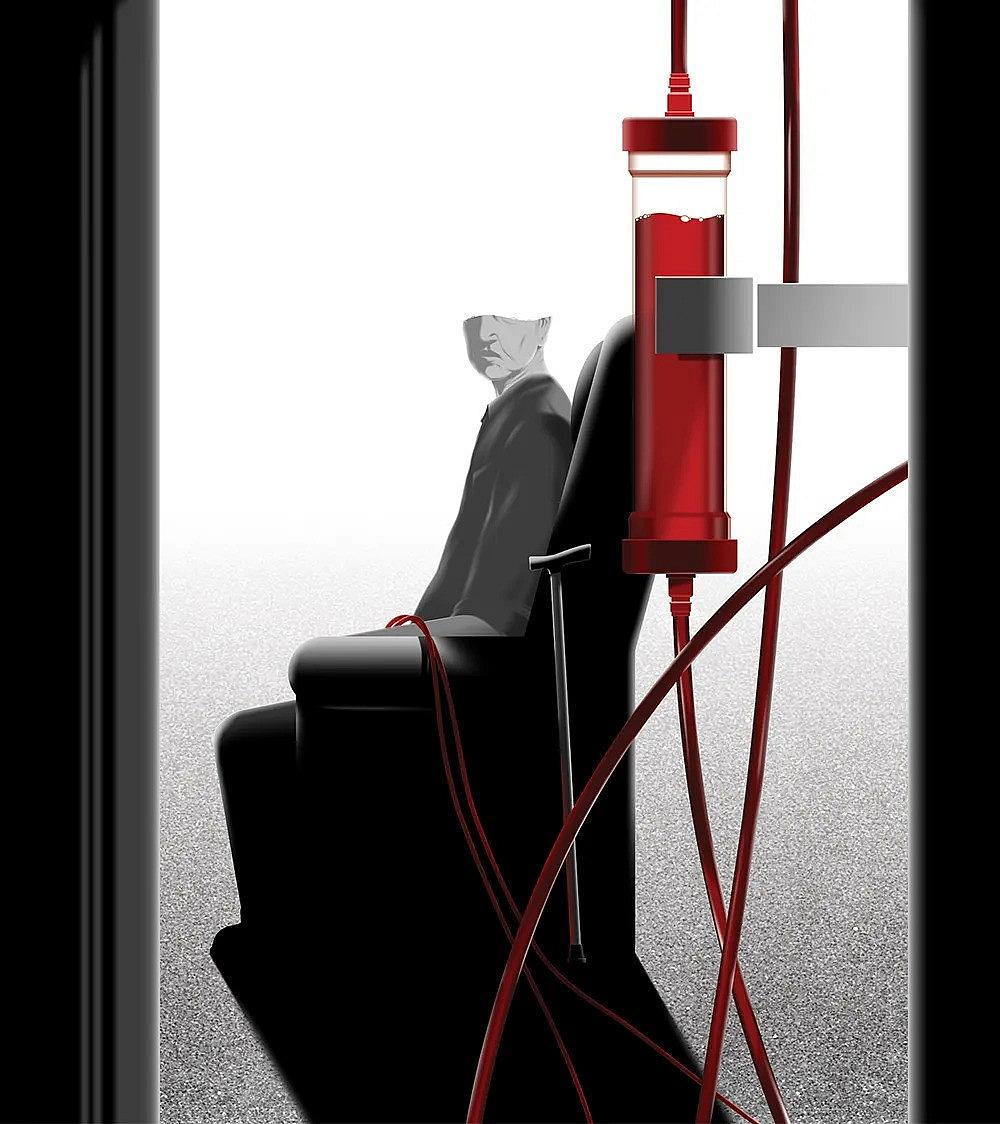
(Anson Chan/Mother Jones)
Tommy Alba could be a pain in the ass.
It’s how he ran two bustling cafes in coastal Virginia. His linebacker physique and booming baritone, with more than a hint of a childhood New Jersey accent, could make him intimidating. Even Lorene Alba, who adored her baby brother, said he wouldn’t take no for an answer. This obstinance served him well, not just in business, but also for the dialysis treatment he received after his kidneys failed in 2011. He lacked health insurance, and his diabetes and high blood pressure had gone undiagnosed for years, working quietly in concert to destroy his kidneys.
For at least four hours, three times a week, in a dilapidated strip mall on busy Jefferson Avenue in Newport News, staffers at a dialysis clinic attached Tommy to machines that removed toxins from his blood, a process that often left him weak and exhausted. While his life had once revolved around his cafes, the machines that mimicked the work of his kidneys were now at the center of everything. Without dialysis, his doctor told him, he would die within days. Tommy’s clinic was one of nearly 3,000 US dialysis centers run by a company called DaVita. Together with rival Fresenius, the two corporations control more than three-quarters of dialysis centers in the United States.
Hemodialysis requires intense poking and prodding: Large-bore needles connect the veins in a patient’s neck, arm, or wrist to a device that draws their blood, detoxifies it, and then returns it to their body.
Because the treatments are so frequent, needle insertion points can become open wounds. Combined with a weakened immune system, this leaves patients vulnerable to infection—which, according to one study, is the third leading cause of death for dialysis patients, accounting for 1 in 10 fatalities. This is why the Centers for Medicare and Medicaid Services (CMS) publishes hundreds of pages of infection control regulations for dialysis clinics. Some are basic, like mandating that clinic staffers wear a fresh pair of gloves to treat each patient. Others are more complex, like the protocols for sterilizing chairs and equipment.
So when a nurse came pre-gloved to insert a needle into Tommy’s arm, he would insist she change into a fresh pair. Nor did he hesitate to speak up if he wasn’t sure equipment had been sterilized properly. He viewed cleanliness as the bare minimum; his safety depended on it. For staffers at his DaVita clinic, it seemed more like an imposition, made worse because Tommy was not a model patient. He had a hard time sticking to a healthy diet, and he occasionally missed appointments. Tommy knew they thought he was trouble. He told his sister he could hear them gossiping behind his back.
Federal rules prohibit dialysis providers from retaliating against patients because of complaints or “noncompliance.” So Tommy was shocked when, one August day in 2021, a DaVita rep told him he was no longer welcome because he’d brought a gun into the clinic and threatened people. Except Tommy insisted he had done no such thing.
He did legally carry a firearm; as a restaurant owner, Tommy dealt with large amounts of cash. But he knew guns weren’t allowed in dialysis, so he would leave his gun locked in the trunk of his aging Escalade. After one session, a technician helping Tommy load his walker into the vehicle spotted the shiny black pistol and immediately reported it to the clinic director. The director, Tommy and Lorene surmised, had spun a tall tale to get rid of a difficult patient. “This is just because you’re trying to shut me up,” Tommy said.
Banishment from the facility was bad enough. But after getting the boot, Tommy struggled to find another clinic for regular treatment. His only other option was to wait until his body was so chock-full of toxins that the local ER would treat him—an approach that kept him alive, if barely. About four months later, Tommy suffered a major heart attack and received an emergency double bypass. He got dialysis in the process, but the hospital couldn’t find an outpatient facility to continue his treatment after discharge, so he returned to the emergency-only dialysis. Amid the continuing pandemic, local hospitals were swamped with Covid patients and he couldn’t always find an ER that would treat him. One January morning, Lorene found her brother unable to get out of bed. By the time the paramedics arrived, he was worse. “I can’t breathe,” Tommy rasped.
Those were his last words. The EMTs tried CPR. It didn’t help. Tommy was declared dead shortly before noon. The official cause was “suspected acute pulmonary edema” due in part to “chronic renal failure and suspected lack of dialysis.”
“He suffered so much at the end, for no reason,” Lorene says.
In the decade preceding Tommy’s death, according to federal data obtained by Mother Jones, more than 5,000 Americans were kicked off dialysis and nearly 1,000 of them died within a year—the official causes of death were not available. The data showed striking racial disparities. One-third of dialysis patients in the United States are Black, but Black patients account for more than half of all involuntary discharges.
At first glance, the terminations look legit. Dialysis clinics seem to be following the strict rules CMS puts in place to make involuntary discharge a last resort. Clinics can’t reject people for being difficult, or for doing the things Tommy did—missing treatments, skipping medications, or ignoring dietary restrictions. They may only cancel patients whose “behavior is disruptive and abusive to the extent in which the delivery of care to the patient or the ability of the facility to operate effectively is seriously impaired.” If clinics follow the rules, and the government enforces them, the only people who should be discharged are the very rare ones who cause an immediate and profound danger to patients and staff.
But according to the experts I spoke with, enforcement by End Stage Renal Disease Networks, the quasi–government agencies tasked with overseeing regional dialysis clinics, often amounts to a rubber-stamping. The networks, which review involuntary discharge requests, usually take the clinics at their word—they’re not obligated to verify the clinic’s story with the patient, and seldom do. As a result, said Nieltje Gedney—who was a member of the ESRD network covering West Virginia, Virginia, Maryland, and Washington, DC, up until her death last fall—they have no way to judge the truth of the allegations.
Gedney was also an advocate and a dialysis patient. Through her work with Home Dialyzors United, a group that encourages a move toward home treatment, she heard at least weekly from dialysis patients facing involuntary discharge for disallowed reasons, she told me during a focus group I convened as part of my reporting—because they were too difficult, too sick, or too bad at following doctors’ orders.
While solid numbers are unavailable, dozens of people I’ve interviewed—advocates, patients, and industry professionals—say dialysis clinics regularly violate the rules, sometimes with fatal results. Unjust discharges happen “often,” says Jennifer Vavrinchik, co-founder and chief operating officer at the National Dialysis Accreditation Commission, which evaluates clinics’ CMS compliance. Social media groups for dialysis patients are rife with stories of people who claim that they got the boot unfairly. An elderly woman with dementia says she was discharged after repeatedly becoming agitated during treatment. After a Black trans woman complained about her treatment by clinic staff, the medical director said her hormone therapy and blood pressure medication were making her delusional, then kicked her out. Other patients’ families have contacted me directly, including the daughter of an elderly, legally blind, wheelchair-using North Carolina man who says he was told to sign a paper discharging him for making threats, even though the form was impossible for him to read. “It’s murder. It’s outright murder,” says another patient, from Maryland, who asked that their name be withheld for fear of retaliation. They were involuntarily discharged in late 2021, when clinic staffers claimed—falsely, the patient insists—that they were violent and disruptive: “Most of these patients, like myself, haven’t done anything.”
Arlene Mullin knows these situations all too well. Her advocacy work over the past quarter century has uncovered countless dialysis patient records she says were full of fabrications by clinic employees. Until the late 1990s, Mullin worked as a dialysis technician for a small clinic in Seattle. After a corporate chain bought the clinic and others like it, she and her co-workers saw corners being cut in the name of profit. Cheap medical tape that gave patients rashes and infections replaced higher-quality tape. Nurses and technicians had to care for more patients at a time, leaving them less able to help those in distress. Feeling she could no longer ethically care for patients, Mullin resigned.
Mullin wrote that “inhumanity is alive and thriving in the industry called dialysis.”
What she witnessed was part of a national trend. Around the same time, nephrologists (kidney specialists) and patients began raising concerns about the corporate takeover of dialysis, sparking a 2000 Senate committee hearing led by Chuck Grassley (R-Iowa). Mullin submitted a formal statement noting that “inhumanity is alive and thriving in the industry called dialysis.” In the wake of the hearing, she dedicated herself to reforming the industry. She founded a small nonprofit, where she volunteers as an advocate for patients experiencing problems with dialysis care. Mother Jones obtained hundreds of her case notes, as well as thousands of emails, faxes, hospital summaries, government and court documents, and more. Her two decades of records tell a chilling story in which patients as young as 11 are denied services based on flimsy or trumped-up charges.
In most cases, the problems begin when a patient complains about their care and, instead of addressing the concerns, the clinic retaliates. Patients told Mullin they’d been called “bitch” and subjected to other derogatory comments during pretreatment weigh-ins. Some claimed technicians became more aggressive when sticking them with the massive dialysis needles, causing undue pain. Others said they were assigned to clinics they couldn’t get transportation to. (In response to questions from Mother Jones, a DaVita spokesperson noted in an email that involuntary discharges make up a small segment of their patient population. “In the rare instance discharge must take place, it is as a last resort…and is done in compliance with state and federal guidelines.”)
In a March 2019 email to Mullin, then–Drexel University nephrologist Jesse Goldman wrote that once a clinic’s staff decide they “want to terminate a patient they are skilled at having multiple employees document a one-sided story. The story is always exaggerated. Not only is the documentation used as ‘evidence’ for the ejection but it also makes [it] more difficult to place patients in the future since the extreme narrative scares away future units from taking a chance.”

The goal, Mullin says, is to eliminate patients who hurt the bottom line.
This isn't about health care. It's about profit.
Kidneys may not be as sexy as the heart and brain, but they, too, are working to keep us alive at every moment. This pair of fist-size organs nestled in the sway of the pelvis regulates bodily fluids and removes excess waste, acids, and other toxins from the blood using a tangle of complex structures with exotic-sounding names like nephrons, glomeruli, and calyx. A person with two healthy kidneys has plenty of filtering power at their disposal. But about one in seven Americans (an estimated 37 million people) have some form of chronic kidney disease. More than 807,000 have kidney failure, or end-stage renal disease. Black Americans are four times more likely than white people to have it. A person with kidney failure has three options: get a transplant, do regular dialysis, or let nature run its course. With spare kidneys in short supply, 97 percent of end-stage patients end up on dialysis.
The giant, noisy machines to which they find themselves tethered three days a week for an average of four hours have only been around for a half-century. When Seattle Artificial Kidney Center built the first few machines in the early 1960s, demand for dialysis far exceeded supply. The God Committee, a small group of mostly men profiled in a classic 1962 Life magazine article, was tasked with choosing the lucky few who would receive treatment. They almost invariably picked white, male, Christian, and relatively young patients—those whom they deemed the most important to save. But even these often more privileged patients couldn’t necessarily afford the treatment, which cost, in today’s dollars, roughly $150,000 a year.
That began to change in October 1972, when Congress passed a law requiring Medicare to cover the costs of care for people with kidney failure. With the government paying the tab—and an increase in kidney failure driven by a rise in risk factors such as hypertension, diabetes, and an aging population—demand surged and a thriving industry was born. More than 550,000 Americans now receive regular dialysis at one of the country’s 7,638 outpatient clinics—more than the number of Burger Kings.
Until the 1990s, most clinics were independently owned and operated, run by hospitals, individual nephrologists, and nonprofits. But investors—who saw the opportunity to lower costs based on economies of scale, and the potential for a steady influx of patients and limited interference from antitrust regulators—began buying and consolidating existing clinics into regional and national chains. Two companies in particular, Denver-based DaVita and Germany’s Fresenius, gobbled up smaller competitors. Today, the two hold a combined 80 percent market share and report multibillion-dollar annual profits.
All of this consolidation has not been good for patients. Independent clinics purchased by for-profit chains, according to one 2019 study, saw a 10 percent jump in mortality rates, and the patients, on average, spent almost three additional days each year in the hospital. To maximize profits, says retired nephrologist Robert Allan Bear, clinics treat as many patients as they can as quickly as possible—“production line dialysis,” as he puts it. US hemodialysis sessions last three to four hours on average, but four to five hours in Australia and Japan, where patient survival rates are higher. Small efforts, such as removing toxins and fluids more slowly (which helps protect fragile patients but requires longer use of the machine) and thoroughly disinfecting each station between uses, eat up more time, cutting into profit margins. Higher-paid nurses have been replaced with lower-cost technicians and assigned more patients per shift. Dialysis chains, another study found, have about a third as many nurses per patient as small, independent clinics do.
In California, such issues have prompted one health workers union (SEIU-UHW) to sponsor a series of contentious ballot measures that would require, at minimum, that a nurse practitioner or physician’s assistant be present during dialysis treatment, and would force clinics to report infection data to the state. “Both DaVita and Fresenius are stuffing billions of dollars into shareholders’ pockets,” David Miller, the union’s research director, told a local news station. “They run giant margins compared to other parts of the industry, so we think there’s more than enough resources to improve patient care.”
They love to paint a false narrative to make you the bad guy,” one patient says. “They’re the bad guy. They’re the monster, but they want to turn it around.”
“There are obviously business interests at play, and that has a whole series of effects on the manner in which dialysis care is provided in the United States,” says Bear, who is Canadian. “The CEOs of those companies have freely admitted that their major concern is to create shareholder value.” By consuming more staff time and attention, challenging patients hurt the bottom line of clinics, which get reimbursed for butts in seats and needles in arms. And more than 120,000 new kidney failure diagnoses a year give corporations a steady supply of patients who might be more compliant and easier to get through treatment quickly.
This profit motive makes involuntary discharge a very American problem. In countries such as Australia, Canada, and New Zealand, the vast majority of clinics must accept everyone. Involuntary discharge “would not be tolerated in the Canadian health care system,” Bear says. “There would be outrage beyond description.”
When Clarissa Pickett went on dialysis in 2017, in her 40s, she looked like the kind of patient clinics want. “I’m very compliant,” she remembers. “I’m very proactive about my care. And I was raised to do the right thing.”
But two weeks in, she developed an infection in her arm that turned into life-threatening sepsis. This made her fastidious about infection control and led her to question her treatment team. Like Tommy, if she didn’t see a tech put on fresh gloves, she asked them to do it in front of her. When a clinic doctor recommended thyroid medication, Pickett researched the drug. Concluding that the side effects would likely outweigh the benefits, she decided against taking it. Sometimes Pickett had to be disconnected from her machine to urinate. “The staff didn’t like that because they saw it as more work. They would always tell me, ‘You’re so needy,’” Pickett says. But “I’m going to keep saying something about it. I’m going to keep raising hell.”
In 2019, when Pickett went in for a dialysis session at a clinic in another town, a technician told her she was nothing like what her chart indicated. It was then she discovered her medical records contained falsehoods about her being aggressive and belligerent. “They love to paint a false narrative to make you the bad guy,” Pickett says. “They’re the bad guy. They’re the monster, but they want to turn it around.”
In early 2020, she was handed a document at her dialysis session: Due to her behavior, her dialysis center would only treat her for 28 more days. Lucky for Pickett, a friend referred her to Mullin, who helped contest the termination and found her a new provider.
Few are so fortunate. CMS regulations stipulate that when discharging someone, a patient’s clinical team must attempt to place them at another clinic. But when the company treating you owns so much of the market, there are few realistic options. If a rival provider does exist in your area, no law says they have to accept the referral. This makes the regulation toothless, Mullin says, and gives clinics the power to cherry-pick the most profitable patients. Indeed, only one-quarter of terminated patients find their way back to regular dialysis at a clinic, according to CMS records I obtained with a public records request. That’s a big problem, says Kevin Tucker, a nephrologist and vice president of education for the Mass General Brigham health care system: “Clinics screen patients exceedingly carefully to try to weed out patients whom they feel may be disruptive to care.”
Of course, some patients do cause serious problems. That’s why involuntary discharge exists, and why courts have upheld the right of doctors to protect themselves. In 1979, a California woman in her 30s with long-standing addictions to heroin and barbiturates sued a dialysis clinic in Oakland for discharging her, claiming her doctor, nephrologist John Weaver, was “the man between me and death.” Weaver countered that the woman would show up to treatment high, yell and curse at staff, and occasionally pull out her IV, spraying the room with blood. Sometimes she exposed herself. An appeals court ultimately agreed that Weaver was not legally obligated to care for this patient. Other legal rulings have upheld a physician’s right to terminate a patient’s treatment as long as it’s not discriminatory or abandoning them without immediate or lifesaving care.
“In my mind, being on dialysis is a privilege,” says Michael Allon, a nephrologist at the University of Alabama, Birmingham. Even so, he says, finding new clinics for banned patients is worth the effort because not doing so is massively expensive. Emergency dialysis cost $2.2 billion in 2017, according to an analysis in the Journal of the American College of Emergency Physicians. Another study calculated monthly savings of $5,768 per person when undocumented, uninsured immigrants were moved from emergency dialysis to thrice-weekly scheduled dialysis.
This is why Allon and a few End Stage Renal Disease Networks launched a “second chance” dialysis program. The small effort works with persistently disruptive patients to place them at new facilities after a cooling-off period, in which they get dialysis at the University of Alabama and spend time with a social worker. “When they recognize the consequences and they are willing to change, with all the caveats that I said, it is reasonable to give them a second chance,” Allon says.
Perhaps the bigger problem is that such a program is necessary. In his nephrology practice in Alberta, Bear saw plenty of patients prone to outbursts and disruptive behavior. What he didn’t see over his four-decade career, he told me, was a single involuntary discharge. He attributes this to lower patient-to-staff ratios. The bulk of care in Canadian dialysis clinics is performed by highly paid and well-trained nurses, Bear says. Technicians are responsible for maintaining the machines, not attending patients. This, and the absence of profiteering, he says, has rendered involuntary discharge nearly nonexistent.
The United States might consider taking a page from Canada’s book. It also could do a better job of vetting involuntary discharges. CMS could hire and train people to interview patients at risk of termination, fact-check the clinics’ claims, and mediate disputes. Simply by enforcing existing rules, the agency could prevent difficult patients from being blacklisted.
Darren Schmidt, a nephrologist at the University of New Mexico, told me he has run remote clinics whose patients, if involuntarily discharged, would have no other alternative. Which is why he’s been speaking with his peers about the problem and lobbying CMS to strengthen its involuntary discharge process. “CMS has no concerns at this time that dialysis corporations are misusing involuntary discharge,” an agency spokesperson noted.
Mullin told me she has gotten little response, despite decades of agitating, from either elected officials or CMS. In her view, involuntary discharge is a civil rights violation. Dialysis termination can be deadly, she says—patients are usually too sick and ill-equipped to fight—and the disproportionate impacts on Black patients make it discriminatory. Lorene Alba saw how the status quo worked out for Tommy. Now, two years after his death, she’s convinced he would still be here if he hadn’t been kicked off dialysis unjustly. He would still be Tommy—her lovable, pain-in-the-ass baby brother—but he would be alive.

