Born on drugs: Babies from addicted moms are increasing at an alarming rate in California
This series was produced with the support of the USC Annenberg Center for Health Journalism Impact Fund.
Other stories in this series include:
Born on drugs: The goal is to keep kids with parents. Sometimes, that’s dead wrong
Born on drugs: Predictions about crack babies didn’t come true, offering hope for opioid era
Lawmakers vow to push stiffer regulations on addiction treatment in California

Dr. Lily Martorell-Bendezu checks an opiate-addicted baby’s heart and muscle tone in the neonatal intensive care unit at Riverside University Health System Medical Center.
(Photo Credit: Mindy Schauer, Orange County Register/SCNG)
Over the decade from 2008 to 2017, as the opioid epidemic took hold, the number of drug-exposed infants born per year nearly tripled in California
It was time for the newborn’s morphine.
Neonatal intensive care nurse Jeri Gibbons placed a dropper between his tiny lips and squeezed the clear liquid — often used to relieve cancer pain — directly into his mouth. His thin arms shot out, grasping at empty air — searching, perhaps, for the mother who was not there, who would likely never be there.
“You’re doing fine,” Gibbons whispered to the infant, swaddling him tightly in a blanket, as is recommended for babies experiencing drug withdrawal.
His mother, a young heroin addict, received no prenatal care. She gave birth in September and left the hospital a day later. There was a comfy chair near the newborn’s bassinet in the Riverside University Health System Medical Center’s neonatal intensive care unit — a chair where moms are encouraged to stay 24/7, to curl up, breastfeed and give their fragile babies the skin-to-skin contact that eases pain and boosts mother-baby bonding.
But the chair was empty. Mom never came. She never even gave him a name.
“We can try to be a replacement,” said Dr. Lily Martorell-Bendezu, the neonatologist at the medical center who specializes in treating drug-exposed babies. “But the voice, the smell. … We want them to be here for the baby, even if they won’t be able to keep the baby. It’s just better for the babies to be with their parents.”
A mom’s presence can cut a drug-exposed baby’s hospital stay in half, research has found.
That simple goal, to keep moms and babies together, informs the state of California’s entire approach to a problem that extends far beyond the hospital doors — to the fast-growing population of babies born exposed to opiates and other drugs.
Dr. Lily Martorell-Bendezu, a neonatologist at Riverside University Health System Medical Center, works with drug-exposed babies. (Photo Credit: Mindy Schauer, Orange County Register/SCNG)
Over the course of the generation-spanning “crack babies” to “heroin babies,” California and the nation have made legal and philosophical shifts, removing fewer drug-exposed children from their parents’ care and working harder to make fractured families whole again before terminating parental rights and putting children up for adoption.
But the process is complex, time-consuming and frequently frustrating, involving many moving parts and a shifting cast of characters — governmental and otherwise — whose judgments may be in direct conflict.
And the window of time parents get to put their lives back together — typically six months to a year — is far shorter than the time it takes to overcome addiction, parents and experts say.
“The health, well-being and safety of these infants may be jeopardized if they are sent home with parents with substance use disorders who do not have a system of support and are not in treatment or recovery,” the Government Accountability Office said.
Such concerns may be well-founded, data suggests.
While the number of kids in California’s child protection system plunged almost 50 percent between 2000 and 2018, the number of infants — younger than one year — shot up more than 9 percent.
More than 2,200 children have suffered fatal and near-fatal incidents in California since 2009. The overwhelming majority of these tragedies — more than 90 percent, according to a Southern California News Group analysis of data from California Department of Social Services — occurred while the children were in the care of their own parents and legal guardians.
When children died, the overwhelming majority — 77 percent — were from families who previously were involved with the child protection system, according to the state’s most recent figures.
When children were seriously injured, more than 60 percent were from families that had been on child protection system’s radar.
About two out of every three children harmed were age 2 or younger. More than half were babies, 12 months or younger. The data does not, however, specify what role substance use played in the tragedies — if any.
Public dilemma
The baby with no name is far from alone.
Nearly 50,000 drug-exposed infants have been born in California since 2000, a parade of human suffering that has touched families, communities and taxpayers. While healthy newborns typically stay in a hospital for a day or two after birth, drug-exposed newborns often need weeks of medical care. The initial extra cost to save these newborns ranges from $159,000 to $238,000 per child, according to research from Stanford University.
Nationwide, neonatal abstinence syndrome — the technical term for babies born in withdrawal — costs U.S. hospitals about $1.5 billion a year, researchers found. The overwhelming majority of these costs — about 80 percent — are borne by public insurance programs like Medi-Cal, and paid for with tax dollars.
Over the decade from 2008 to 2017, as the opioid epidemic took hold, the number of drug-exposed infants born per year nearly tripled in California, according to figures from the Office of Statewide Health Planning and Development.
But the epidemic hasn’t hit every community equally.
In some counties, including Merced and Stanislaus, drug-exposed births more than quadrupled. In Los Angeles, Riverside and San Bernardino counties, they’ve more than tripled. And in Orange, Santa Clara and Contra Costa counties, they’ve more than doubled.
But in Alameda — a county with what some experts say is the most effective family drug court in the state — drug-exposed births increased less than 2 percent.
Experts caution that the numbers — 5,050 drug-exposed infants born in California in 2017, or about 14 new babies every day — offer only a partial snapshot of the problem. Because there’s no mandatory drug screening for mothers and infants in California, many drug-exposed births are likely happening under the radar. That’s especially true among wealthier women with private insurance, experts say.
Also missing in this data are the mothers who quit cold turkey when they discover they’re pregnant, only to return to the needle, or pipe, or pills, as soon as the baby is born.
“The harm done is understated tremendously,” said Sidney L. Gardner, president of Children and Family Futures, a national nonprofit based in Lake Forest that studies the intersection where child welfare, addiction treatment and court systems meet.
Gardner describes a “pyramid of harm.” At the top are the comparably small number of child fatalities, resting atop a vast base of kids impacted by drug exposure who may eventually suffer injuries and learning difficulties related to the drugs their mothers ingested.
“There’s a disability side that is, I think, horrifyingly understated, undercounted, misunderstood or deliberately set aside,” Gardner said.
Sid Gardner, is president of Children and Family Futures. (Photo Credit: Jeff Gritchen, Orange County Register/SCNG)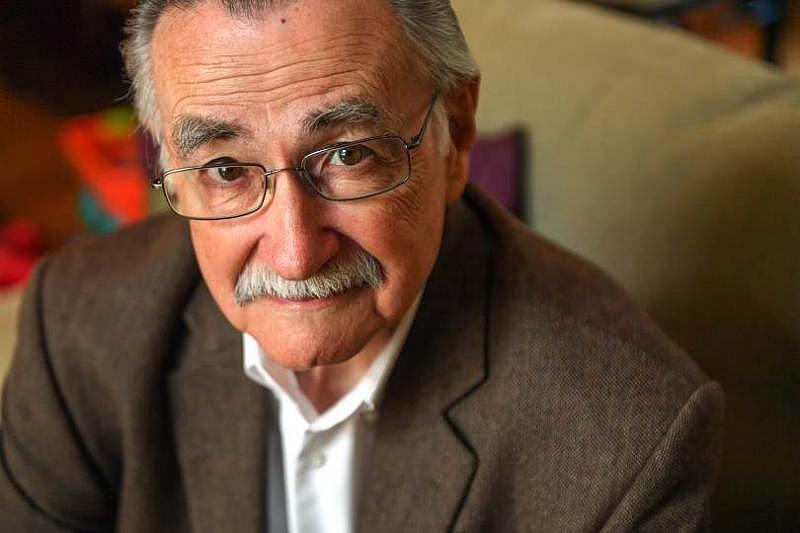
The federal Child Abuse Prevention and Treatment Act (CAPTA) requires states to draft “plans of safe care” for substance-affected infants — which means probing family circumstances and connecting them to services that ensure the child’s safety.
That law was amended in 2016 by the federal Comprehensive Addiction and Recovery Act (CARA). It now requires that “plans of safe care” created for drug-exposed infants specifically also address the substance abuse treatment needs of their parents.
But the federal government hasn’t been specific about precisely what that means, and states are interpreting it in different ways. California maintains that the safety plans it has always drawn up for children satisfy the new federal requirements, but Gardner disagrees: California fails to follow these children far enough into the future as they grow, and so can’t address learning and behavioral problems that might not manifest until elementary or secondary school.
“We’re going to see those kids over and over again,” Gardner said. “We’re going to spend a lot of money on them. These babies cost hundreds of thousands of dollars. Some of these are million-dollar babies.”
Over the past decade alone, Medi-Cal has spent about $111 million on care for drug-exposed infants, according to data from Department of Health Care Services. Gardner said that’s just the tip of the iceberg.
Lucky one
At the Riverside University Health System Medical Center’s neonatal intensive care unit, baby Andrew — the nurses often call unnamed baby boys Andrew — was doing well, all things considered.
His eyes were open and watchful, even as a tube snaked up his nose and wires bristled from his skin. He wasn’t trembling. He wasn’t irritable. He wasn’t refusing food or crying the inconsolable, kitten-like cry that’s common to babies in opioid withdrawal.
On a 30-point scale — with 30 being the worst — Andrew was at about 7, which meant his morphine dose could be dropped by 10 percent every two days until he was weaned off the drug.
To the staff, his future looked promising.
“People line up to adopt infants like him,” said nurse Tammy Johnson.
Indeed, he was luckier than many drug-exposed infants in California who did have names:
- Reginald Jules was born — and died — on July 7 from maternal methamphetamine use, according to records kept by the Los Angeles County medical examiner.
- Baby Girl Ford was born — and died — on June 26, with “maternal cocaine intoxication” as one of the causes.
- Everett Deshazer was born — and died — on April 2, from “placental abruption and toxic effects of methamphetamine from intrauterine exposure.”
While the number of drug-exposed babies has commanded wide attention, the number of young children who die or are injured due to drug exposure has not.
More than 100 children younger than 5 have died from drug exposure since 2006 in California, according to data kept by the California Department of Public Health and other agencies. Another 52,519 young children were rushed to hospital emergency rooms after drug exposure, and 6,102 were hospitalized, according to the data.
Government grinds into gear
Martorell-Bendezu, the neonatologist, has two children of her own. She has authored papers about how to best care for drug-exposed infants. Her empathy for them — and for their addicted parents — runs deep.
“What they have is a disease,” she said, noting changes in the brains of addicts. “They crave this. They need this (drug) to be OK. It’s not as though they’re doing it on purpose; they can’t help themselves.
“It’s easier to understand when you look at it that way.”
While some states classify — and prosecute — prenatal substance abuse as criminal child abuse, California does not. Instead, communities are trying to do what Riverside County is doing — building a safety net for these women and their babies, a protected space where there are no handcuffs and no judgment, only help.
Riverside’s program is held up as a model by the California Health Care Foundation. Myriad agencies are working together to reach drug-addicted, pregnant women before they deliver. They offer a broad range of support, from medication-assisted treatment to prenatal care to services that can stabilize their often chaotic lives.
“We want them to see that they don’t need to be afraid,” Martorell-Bendezu said of addict moms. “We want them to understand we’re here to help them, and to help them stay together” with their children.
In the infant ICU, the help is, literally, hands on.
Every three hours, at least, someone picked up the baby with no name. The more often, the better; the importance of human touch to a baby’s well-being cannot be overestimated. The hospital has a volunteer cuddlers program, but more cuddlers are always in demand.
But with the mother absent, the baby with no name became a ward of the state of California. And as is required when tests show an infant is “pos-tox” — drugs were found in his system — Child Protective Services was notified.
And, with that, the complex machinery of the state’s child welfare system rumbled to life.
In California, parental drug use is not by itself grounds for taking a child away. The state is to provide the services and support necessary to keep parents and children together — even parents with onerous problems like addiction.
Sometimes, it works.
Melanie Quijano, Tonika Reed, Catie Kovelman and Jordan Lemke contributed to this report.
[This story was originally published by The Orange County Register.]

