Extreme Heat Killed 14 People in the Bay Area Last Year. 11 Takeaways From Our Investigation
Molly is one of the recipients of the 2018 Impact Fund, a program of USC Annenberg's Center for Health Journalism.
Other stories in this series include:
How Hot Was It In California Homes Last Summer? Really Hot. Here's the Data
Investigation Finds Home Can Be the Most Dangerous Place in a Heat Wave
Even in San Francisco, Heat Is Turning Deadly. That's Not Something Colleen Loughman Expected.
It's getting (dangerously) hot in Herre
Being outside can be dangerous, especially at school
What you need to know about LA’s urban heat problem
Sweltering in nursing home, 95-year-old succumbs to heat, as climate endangers most vulnerable
The danger of urban ‘heat islands’
New Rule Would Require Employers to Protect Indoor Workers From Heat Illness
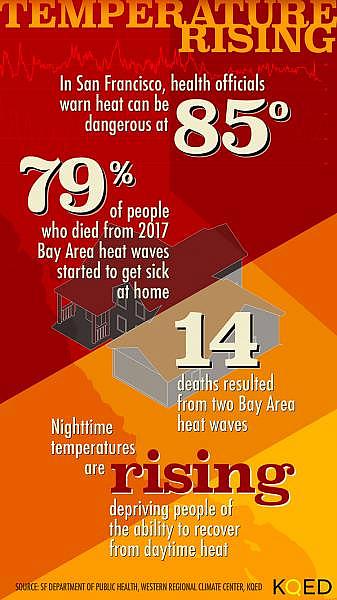
Even in cool, coastal California, extreme heat sickens and kills people. In 2017, extreme heat killed 14 people in the Bay Area. Over Labor Day weekend, six alone died in San Francisco. The heat also sent hundreds more to the hospital.
In July, August, and September this summer, we measured heat in 31 homes, in four counties, across the state. We found that in every home, it was hotter inside than outside -- even after the sun went down -- depriving people of the ability to cool off at night. Within two decades, scientists predict extremely hot days in the Bay Area three to four times more often than in recent years.
Heat waves don’t have to end in death; heat illness is preventable. But no rules require doctors to track it. Nothing in landlord-tenant law establishes a broad right to cooling. No laws set standards for local responses when temperatures spike, even though climate change means warmer nights and more intense heat waves.
Climate-driven heat isn’t simply sending more people to hospitals. It’s changing our relationships to the built environment, through big decisions and little ones. And as systems evolve, Californians are mostly on their own as they try to cope with a familiar, but growing, danger.
1. Even 85 degrees can be dangerous for Bay Area residents.
People who live in cooler climates can get heat sick at lower temperatures, partly because they can't adjust quickly. And nighttime temperatures are rising, depriving people of the ability to cool down.
2. 'It takes almost two weeks for your body to acclimate to the heat.'
Naveena Bobba is the deputy director of public health for San Francisco. She says because heat waves tend to come and go in a matter of days in the Bay Area -- far too quickly for the body to acclimatize -- that means heat continues to build up in the body day after day.
3. Cities and counties aren't sure of the best actions to protect people.
"Right now, unfortunately, we don't know" whether cooling centers, text alerts or targeted messaging works, says Arizona State University climatologist David Hondula. “We have hunches about what works, and those hunches are probably not totally wrong, but it would be really nice to validate those hunches with some some data.”
4. Heat illness itself is underdiagnosed, undertreated, and undertracked.
Symptoms get missed: at home, people may not associate symptoms with heat exhaustion; in emergency rooms, doctors unfamiliar with heat stroke may take time to diagnose it. Beyond that, asthma, lung trouble and heart disease worsen, and complications from diabetes and obesity are more frequent when temperatures rise.
5. Heat illness and death are preventable.
Even undercounted, heat kills more people each year than any other disaster. But unlike earthquakes or fast-moving fires, heat can be forecasted by weather experts. Public health officials can issue warnings, and communities can set up ways to check on vulnerable people and cool them down. Cities and counties can promote cool rooftops through ordinances, plant more trees, and work with building owners to seek retrofit funding for double-paned windows or insulation.
6. Despite an abundance of solutions, Californians are on their own.
Many of the ideas that could help reduce the health risk for Californians are not close to the top of the agenda for policymakers. Many Bay Area counties haven't updated their emergency plans to account for the warming from climate change. Finally, health departments have little funding to address heat.
7. Heat risk deepens the divide between the "cool haves" and the "hot have nots."
Very old and very young people are the most vulnerable. So are people on certain medications, and who have pre-existing conditions. Environmental and social conditions also raise risks for poorer people, for people without air conditioning, among Latino and Black communities, and in segregated cities, which tend to have less in the way of tree canopy.
8. Of Bay Area residents who died in last year's heat, 79 percent began to get sick at home.
Official statistics are at least a year from being public, so we asked counties for unofficial totals, pulled death certificates and requested coroner’s reports. Of 14 people who died in the heat waves last year, 11 began to have symptoms at home.
9. Homes where we placed sensors stayed too hot to allow people to recover from heat.
Homes we tested in Contra Costa and Santa Clara counties got hotter inside than out, and held onto heat longer. At night, houses might be 15-20 degrees warmer than outside. That’s a problem for people who can’t afford or don’t have air conditioning, says the Public Health Institute’s Linda Rudolph. “When the nighttime temperatures don't go down, which is what's increasingly happening with climate change, it's harder for them to get that kind of physiological rest period.”
10. Air conditioning helps, but may be out of reach.
Heat Investor-owned utilities including PG&E are adopting “time-of-use” pricing, to charge for electricity based on when demand peaks – which is late afternoon. According to sensors we placed in homes, that’s exactly when homes start to overheat. UCLA sustainability researcher Stephanie Pincetl says this pricing plan will make cooling older residences more expensive for people who already can’t afford their bills. “Really what we need to do is have much better buildings,” she says.
11. Glassy new condo or beat-up hotel -- neither are made for heat.
According to a San Francisco Department of Public Health analysis, expensive newer condos and older Single Room Occupancy high-rises around Market that once catered to seafarers and gold prospectors are both poorly-designed for a warming world. Our measurement of SROs found they were all significantly hotter than outside, all of the time. Residents told us heat left them few options: head to the basement, or leave the building.
Editor's Note: Amel Ahmed contributed research and reporting to this story. This reporting is supported by a grant from the USC Annenberg Center for Health Journalism Impact Fund.
[This story was originally published by KQED Science.]

