
Gergana Koleva
Contributor

Contributor
What effects do misleading advertising, poor oversight of the food, drug, and sports industries, and other forms of consumer fraud have on health? In my blog on Forbes.com, I examine the relationships between financial incentives, questionable business- and bio-ethics, and consumer safety. I previously covered these topics for Aol's Daily Finance, after having written about banking and investing for MarketWatch and American Banker. Follow me on Twitter: @gerganakoleva
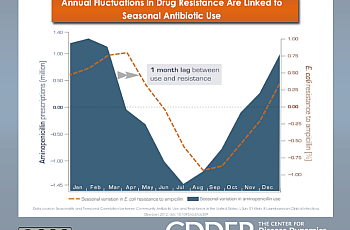
Physicians who see patients outside of hospital systems, such as those working in private offices, contribute disproportionately to the spread of antibiotic resistance because they are more likely to prescribe drugs unnecessarily, a first-of-its-kind nationwide study that looked at patterns of antibiotic use and drug-resistant infections has found.

In the world of public health, no scenario involving infectious disease is too far-fetched. How often can scientists predict what virus is going to emerge and survive long enough to take hold around the world? How rapidly can governments gear up and prepare to deal with a pandemic? And should we worry about such things at all, or is the era of fast-spreading infectious diseases behind us?

<p>Can vaccines be more useful for some people than for others?</p>
Hospitals across the country are using near-total discretion in the way they disclose infections that occur as a result of surgeries, cause over 8,000 deaths annually in the U.S., and cost an additional $10 billion per year to the healthcare system, a new study underscoring the need for public reporting standards has found.
<p>A confluence of factors including an inflexible regulatory enviroment that discourages research and discovery, a paltry research pipeline for drugs for the most serious illnesses, and a tendency for physicians to unnecessarily prescribe antibiotics for routine aches and pains is largely responsible for the rise of antibiotic-resistant infections in humans, speakers at a major conference on infectious diseases this week announced.</p>

<p>An ambitious plan to reverse New York’s growing prescription drug epidemic is causing a rift between legislators and health care providers, pitting a proposed computer system that would require doctors and pharmacists to meticulously scan patients’ medical history for patterns of abuse against arguments by two professional associations that increased monitoring would backfire.</p>

<p>Regenerative Sciences, a medical company that pioneered a procedure to treat orthopedic injuries using patients’ own stem cells, is fighting the Food and Drug Administration tooth and nail over a claim that human cells should be federally regulated as drugs, in a landmark case that has far-reaching implications for the future of regenerative medicine.</p>
<p>The American Red Cross, the largest supplier of donated blood in the U.S., was fined $9.6 million after federal inspectors found hundreds of blood safety violations at 16 of the organization’s 36 blood collection centers nationwide.</p>

Sodas, sports drinks, and other sugar-sweetened beverages appear less tempting to consumers when labels show caloric information in terms of minutes of jogging rather than as absolute calorie counts, new research from two leading public health universities suggests.

The U.S. Food and Drug Administration will no longer consider withdrawing its approval for the routine use of penicillin and tetracyclines in food-producing animals, despite mounting evidence that traces of these drugs in retail meat reduce the effectiveness of antibiotics in humans, the agency quietly announced in the Federal Register the Thursday before Christmas.