The Health Divide: Marginalized communities overlooked in addiction treatment, and food insecurity rises
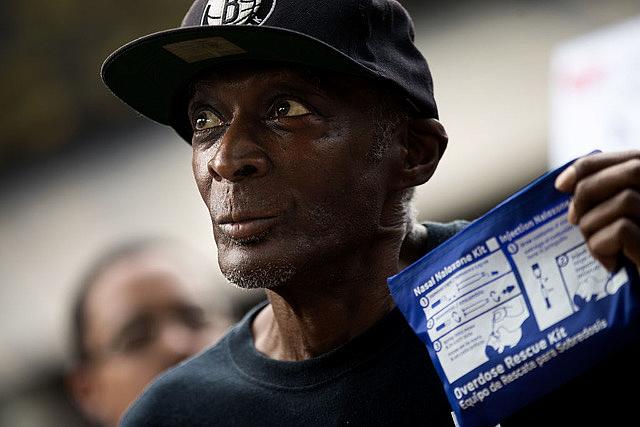
Getty Images
Women, teens and Black adults miss out on lifesaving addiction meds
Even as overdose deaths continue to rise, only about 1 in 5 adults with opioid use disorder receives medications that reduce cravings and ease withdrawal symptoms, according to a study in JAMA Network Open.
“Despite this being the worst overdose epidemic in history and having medications readily available to treat opioid addiction, too few people receive medications for opioid use disorder, and there are ongoing and worsening disparities in who receives them,” Dr. Sarah Wakeman of Mass General Brigham, who wasn’t involved in the study, told HealthDay’s Denise Mann.
Women, Black adults, unemployed people and those living in rural areas were less likely than others to receive medicines such as buprenorphine and methadone, the researchers found. The study tracked medication use in 2021.
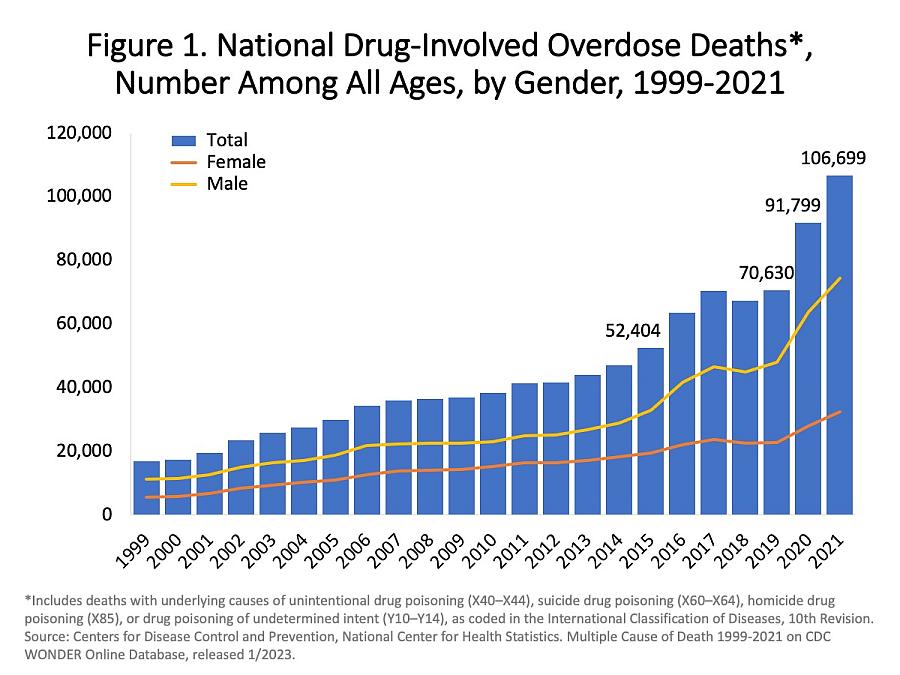
Centers for Disease Control and Prevention, National Center for Health Statistics.
Three million Americans suffer from opioid use disorder or had it in the past.
“Addressing disparities in medication for opioid use disorder uptake should be prioritized in program, policy and clinical initiatives,” wrote the study authors.
Telehealth treatment significantly improved the chances a person would receive a prescription, the authors noted. Additional state financing and mobile methadone clinics would also help improve access, study author Dr. Wilson Compton told HealthDay.
Narcan, which reverses the effects of opioid overdose, will soon be available over the counter.
Another approach that can save the lives of people who’ve overdosed is to provide oxygen. At the Los Angeles Times, Emily Alpert Reyes details how a nonprofit is dispatching teams with oxygen tanks, medication and other supplies to Skid Row.
Narcan is a lifesaver but it can take minutes to act. Oxygen can stabilize people, including those who overdose on non-opioid drugs that do not respond to Narcan.
Adolescents are also missing out on effective treatments because many detox facilities don’t treat teens, reports Markian Hawryluk at KFF Health News.
Red Cross welcomes gay blood donors — with exceptions
In what a Red Cross spokesperson called “one of the most significant changes in blood banking history,” many gay and bisexual men will now be allowed to donate blood.
The change “marks the end to a decades-old ban rooted in discrimination and bias,” David Stacy, vice president of government affairs at the LGBTQ advocacy Human Rights Campaign, told NBC News’ Benjamin Ryan.
Early in the AIDS epidemic in the 1980s — when gay sex was still illegal in many states and good screening tests for HIV were not available — men who had sex with men were banned from donating to keep the infection out of the blood supply. But with improved blood testing and a changing political landscape, many considered the ongoing ban discriminatory and self-defeating in the face of frequent blood shortages.
Now, guidance from the Food and Drug Administration has “caught up to the science, at least for the most part,” writes Jen Christensen at CNN.
According to the new guidelines, people of any gender or sexual orientation will still be deferred from donating if they have had a new sexual partner or more than one sexual partner and had anal sex in the past three months. This is meant to limit possible donations from people who are newly infected with HIV and don’t realize it yet; HIV tests can miss the virus during the first month of infection.
People who’ve recently had sex with someone who is HIV positive, as well as people taking pre- and post-exposure prophylaxis for HIV, will also be also deferred. The FDA thinks the prophylaxis meds might cause HIV-infected blood to erroneously test negative.
The new policy “makes blood donation more inclusive, and it also keeps the blood supply safe,” Red Cross communications specialist Rodney Wilson told CNN.
But Jason Cianciotto, vice president of communications at the HIV/AIDS service organization GMHC, said the new rules unfairly exclude people who use condoms in those specific sexual situations, and confuse the government’s messaging that prophylaxis keeps people safe from HIV.
Wilson said the Red Cross hopes to eliminate the HIV prophylaxis deferral in the future.
“There’s still work that can be done to make blood donation even more inclusive,” he admitted.
Food scarcity increases as COVID-era benefits lapse
About 3 million more people don’t have enough to eat after the expiration of pandemic-era food stamp access, reports Chris Gilligan at U.S. News & World Report.
According to the U.S. Census Bureau’s Household Pulse Survey, which covered late June and early July, 12.1% of respondents said they didn’t have enough to eat in the preceding week.
That’s a rise from 10.7% at the end of February, when the COVID-related expansions to the Supplemental Nutrition Assistance Program came to an end.
Food insufficiency was highest — over 15% — in Mississippi, Oklahoma, Tennessee, and Georgia.
What we’re reading:
- “Henrietta Lacks settlement hailed by experts as a step toward correcting medicine’s racist history,” by Annalisa Merelli, STAT
- “Amid lack of accountability for bias in maternity care, a California family seeks justice,” by Sarah Kwon, KFF Health News
- “For Black folks, medical mistreatment starts young,” by 2023 National Fellow Alexa Spencer, Word in Black
- “Systemic racism continues to cause preventable deaths,” by Lisa O’Mary, WebMD
- “Maternal care deserts overlap with lack of abortion access, analysis shows,” by Nicole Wetsman, Dr. John Brownstein and Dr. Benjamin Rader, ABC News
- “Why promising new Alzheimer’s drugs may not work as well in Black Americans,” by Margo Snipe, Capital B
- “How heat makes health inequity worse, hitting people with risks like diabetes harder,” by Yuki Noguchi, NPR

