Battle of the Breasts
Are you confused, angry and, frankly, pissed off as you watch sumo-sized egos battle out the mammogram issue? How will it affect you and your loved ones? What actually is the thinking behind the new United States Preventative Services Task Force recommendation to NOT screen women in their forties for breast cancer? Is it as nonsensical as it sounds? Doc Gurley gives you a common sense, plain-language explanation of the ins and outs of this complex issue. She's a practicing board-certified internist who's also published cost-effectiveness research. Check out these 16 crucial facts, so you can make informed decisions for yourself, your health, and the health of those you love.
It's a battle of the healthcare titans. On one side, the United States Preventative Services Task Force (USPSTF) and its new recommendations to stop mammogramming women in their forties, and even to stop doing self-breast-exams. And, on the other side, the Susan G. Komen Foundation, the Mayo Clinic, Health and Human Services Secretary Kathleen Sebelius, the American Cancer Society, and the American Society of Clinical Oncology, who have all dissed that new set of recommendations. What's at stake? Your insurance coverage for mammograms aged 40-49, your breasts, your health, your peace of mind.
Hey, it's a big deal. The words "breast cancer," alone, are enough to make the ground shudder for lots of us. So the last thing we need or want is an earth-churning battle between colliding sumo-sized egos. Which leaves many of us wondering - what exactly is behind this mega-med conflict?
Here's the Doc Gurley common sense, plain language answer to that question, with 16 crucial facts for you to know for interpreting these behemoth battles about your breasts. Please feel free to forward it to any woman (or person who care about a woman) who might be interested in this topic:
The Facts:
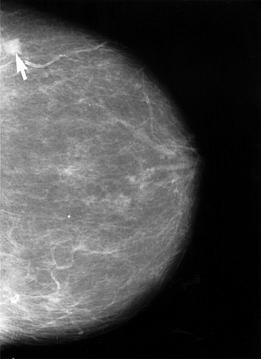
1) When it comes to routine mammograms, we're talking about screening people with NO symptoms. Any breast lump, pain, discharge, dimpling, or rash needs a thorough evaluation - that's a completely different topic.
2) We're talking about screening people with average risks - NOT anyone with genetic, family, or other history that puts them at increased risk - also a completely different topic.
3) Mammograms save lives. That's a proven and re-proven fact. They're far from perfect, but here are the numbers, by age group: "For ages 40-49, the analysis of the results by the USPSTF showed a 15% reduction in breast cancer mortality, which was similar to the risk reduction for women aged 50-59 while the risk reduction was 32% for women aged 60-69."
4) Mammograms are relatively cheap.
5) Mammograms, as a procedure, have very few serious health complications (but ouch. Really, people. Big ouch.)
6) You have to screen a lot of people to save one life. We're not talking about finding a cancer here, we're talking about saving a life. That's a much higher standard - one that shockingly few medical tests reach. What is the exact number? Here are the nay-sayer's own figures, based on mathematical models (using numbers from clinical trials): "the USPSTF estimates that averting 1 death from breast cancer requires screening 1,904 women aged 40 to 49 years; 1,339 women aged 50 to 59 years; or 377 women aged 60 to 69 years." The number-needed-to-screen to save one life may sound big to some people, but it's actually similar in size to other screening tests. Notice the relatively similar size of the number for women aged 40-49 (screen 1,904), compared to women aged 50-59 (screen 1,339).
7) But if you're one of these screened women, you MAY get a false-alarm. In other words, mammograms, as a test, have some "noise" to them. There are false positives ("we found something" - but it turns out not to be cancer) as well as, more commonly, false negatives ("your mammogram is clean," but that doesn't mean you can't have a tiny silent tumor that doesn't show on mammogram). How do you factor in the "noise"?
8) A cost effectiveness model adds in the costs of doing all these mammograms, PLUS the costs of all the tests for the false positives, to calculate the price of saving a life.
9) It is the FALSE POSITIVES that add a bunch of cost - because they usually end up with a surgical biopsy.
10) In addition, there is the idea that some breast cancers that are found might not have killed anyone. Kind of a radical idea, huh? And not an idea you'd want to bet your life on. But the (relatively big) cost of treating those presumed "overdiagnoses" are also charged against the costs of saving that one life.
11) Even with all of that added in, mammogram screening is cost-effective. UNTIL you add in the "harm" factor. That's the amount of self-reported anxiety and distress and pain that women feel from worrying and waiting and being procedurized for a false positive. THAT's the number that makes mammograms in a woman's 40's seem "harmful." In fact, it is THE key part of the USPSTF ("the nay-sayers") justification for saying doctors should only screen every two years: the idea is that every 2 year screening will halve the rate of "harm."
12) The big assumption that checking half as often will halve the "harm" of false positives is a truly false assumption (sorry, USPSTF). See, if you have some schmutz that's going to show up on your mammogram - regardless of whether it shows up in your 40's or 50's - that schmutz isn't going to appear half as much just because you're checking less often. Think about it. Your breast gets a bit dense in one spot. Sure, some of that comes and goes. But what we're talking about is the persistent kind of "spot," especially when it comes to tumors that presumably would not have killed you after all (and those add a lot of cost and anxiety to this model). Your body makes a smudgy place on a mammogram (one that lasts), your test finds it, you take it out, it's gone - whether you find it age 44 or 45. Whether you're mammogramming every year or every other year, that smudge would appear and you would go through the stressful process of sorting out that it's not cancer. By reducing mammograms to every other year, you may halve someone's anxiety about getting their boob mashed into inhuman thinness, but you won't halve the absolute number of procedures for true false positive masses, or for overdiagnoses of tumors that won't kill someone. And the naysayers admit, reducing mammograms to every other year means some lives lost. Not many, but if it's you, I can promise you, it will feel like one too many...
13) Nowhere does this (or any) cost-effectiveness model ADD IN the benefits of peace of mind. In current cost-effectiveness modeling, you can only detract from health, you can't adjust upward for mental benefits. That's a monstrously huge flaw in these discussions. I personally had a false positive, all-the-way-to-biopsy (really big ouch) mammogram result. I can tell you, looking at my two elementary-school-aged kids and knowing that the smudge on my mammogram was NOT CANCER and was now gone forever was a HUGE benefit.
14) What no one is discussing (much) in the media is the fact that these new recommendations are similar to European guidelines. The massive problem with that approach is that Europe has universal healthcare. We don't. Unless you have universal healthcare coverage to guarantee easy no-cost access to doctor evaluations, timely treatment, and in-depth counseling and education about risks, you can't adopt their screening practices. They have a safety net (and possibly bigger issues around over-screening and over-diagnosis). We don't.
15) They stuck a price on your life. Literally. Here's a great summary from a surgeon/scientist's take on this issue (check out the full post for a wonkier, and slightly different, opinion on this same issue): "Indeed, the current recommendations of the USPSTF are no less arbitrary or necessarily more scientific than previous recommendations for screening. What they reflect is a different attitude towards the risk-benefit ratio, in which the modest benefits of mammography in women between ages 40-49 are judged not to be worth the harm caused. Others may look at the same data and decide that the benefits of screening in this age range are worth the potential harms. What we should all agree on is that women should be aware of and understand as much as possible those tradeoffs. In the meantime, I'm not entirely buying these new recommendations, at least not the argument that they are more "science-based" than the older recommendations when, in actuality, they also arbitrarily decide that screening 1,300 women to save one life is an acceptable cost but screening 1,900 to save a life is not."
16) What about for older women? Should you stop having mammograms at 75? Or 80? Or never? No matter what you hear in the news, the bottom line is...they don't know. Here's the USPSTF's own statement: "The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of screening mammography in women 75 years or older." So what does all this mean? If you're a woman in your 40's, it means you should argue with your insurance company if they try to deny coverage for mammograms until you're 50. It means you should think long and hard about where you fit in the spectrum of "harm" - how much of a life-hit would you take if you had a false-positive? But, conversely, how much benefit do you get from doing what you can to stay healthy? And, at it's most basic and brutal, given the small difference in numbers-needed-to-screen, is your life in your forties worth less than someone else's life in her fifties?
Because the bottom line is still...mammograms save lives.

