At California psychiatric hospitals, epidemic of patients’ assaults on staff goes untreated
This article was produced with the support of the California Data Fellowship, a program of the Center for Health Journalism at the USC Annenberg School for Communication and Journalism.

Nearly 200 Napa State Hospital workers demonstrate for safer conditions in 2010, in the wake of the killing of staff member Donna Gross at the hands of a patient. (Robert Gauthier/Los Angeles Times via Getty Images)
California’s network of state psychiatric hospitals is charged with treating people with mental illness who pose a danger to themselves or others, but workers faced with ongoing assaults by patients have struggled to provide a therapeutic environment. In this in-depth account, veteran California journalist Liza Gross reports that injured workers at the five psychiatric hospitals, including Napa State Hospital, have lost tens of thousands of workdays while taxpayers pay millions of dollars in workers’ compensation and overtime costs.
Stephen Seager felt lucky when Napa State Hospital offered him a job as staff psychiatrist in the spring of 2011. His wife, also a physician, had already relocated to Northern California from their home in Utah, after cutbacks at their hospitals forced the couple to find new positions.
Seager had originally trained as an emergency room physician, but the continual stream of traumas burned him out. He switched to psychiatry for a change of pace. He’d been drawn to medicine to help those in need, and people with severe mental disorders certainly fit the bill.
Seager had treated patients in acute psychiatric distress at hospitals in Phoenix, Los Angeles and St. George, Utah, but, like most psychiatrists, he’d never set foot in a state mental hospital. He just knew they treated some of society’s sickest psychiatric patients and that most had been judged incompetent to stand trial or not guilty by reason of insanity. He thought he could help them.
When Seager took the job at Napa, he says he didn’t know that even people found to have committed violent acts were free to wander the hospital halls. He also didn’t know that the clinical staff doubled as security guards.
And he didn’t know that seven months before he showed up for work, a veteran psychiatric technician named Donna Gross had been murdered right outside his new office.
The exact details of Gross’ death are not known, but police investigators and state occupational safety inspectors were able to piece together the general outlines of what happened, the coroner’s and inspector’s reports show.
On Sept. 23, 2010, Gross (no relation to the author) was returning from a break for her second shift of the day, around 5:30 p.m., when she entered the hospital’s secure treatment area, which houses patients deemed criminally insane. She walked across the grounds, where many patients congregated unsupervised. Before she reached her unit, a patient grabbed her and dragged her behind a patio wall. Gross pressed the alarm on her belt, but nobody came to her aid. Staff alarms, according to court records, didn’t work outdoors.
An hour after the 54-year-old grandmother had passed through security, her colleagues found her sprawled on the courtyard patio, dead. Police quickly determined that Gross had been strangled by Jess Massey, a 37-year-old patient known for his violent history and penchant for stalking.
Most patients who assault staff, according to Seager and other staff members, remain on the wards. After all, many came to California’s state psychiatric facilities because they committed violent crimes. Massey had been sent to Napa after pleading not guilty by reason of insanity after repeatedly stabbing a woman in a Sacramento parking garage. Police investigators said Massey confessed to killing Gross. He pleaded no contest in court and is now serving 25 years to life at Corcoran State Prison.
Gross’ murder forced California hospital administrators to respond to increasing pressure from employees who’d long protested perilous conditions at the state’s five psychiatric hospitals. Officials offeredshuttles so Napa employees didn’t have to walk through the grounds, and tightened restrictions on grounds passes.
A month before Seager started working at Napa State, the Occupational Safety and Health Administration fined the hospital $100,140 for “serious” and “willful” violations that led to Gross’ death. This time, hospital administrators agreed to deploy security teams to patrol the grounds and lifted a hiring ban.
It wasn’t enough — not for workers at Napa or the state’s other facilities. Since Gross’ death, employees at California’s five psychiatric hospitals have suffered thousands of assaults a year, resulting in tens of thousands of lost days on the job and costing taxpayers at least $135 million in workers’ compensation and overtime.
Dr. Stephen Seager
As a new employee, Seager had barely stepped onto his unit when a burly patient batted the slightly built doctor aside like a fly, sending him crashing into a wall. Seager’s head hit with a thwack that split open his scalp. The man then grabbed a heavy wooden chair and smashed it over an older patient’s head. Seager, who’d just turned 61, tried to stanch the blood gushing from the man’s head until paramedics arrived. “I’ve kept up my ER skills as a psychiatrist because I have so many emergency beatings and traumas,” he says.
Seager’s colleagues convinced him to go to the county hospital. It took 10 stitches to close his wound. The patient never returned. Seager heard he’d been flown out to a nearby hospital. He found out the patient died only because a colleague’s relative worked at the hospital where he’d been treated.
At Napa State, violence was — and still is — just part of the routine, as the signs that are posted twice a week reporting assaults on staff indicate. There are steps officials could take to control the violence at California’s state hospitals, Seager says — steps that would ultimately save taxpayers money. “But the administration and Sacramento don’t seem to care.”
Safety Measures Fall Short
Neither the measures taken before Seager’s arrival, nor those taken since, have stopped the bleeding at California’s five psychiatric hospitals. In the years following Gross’ death, workers at Napa, Patton, Metropolitan, Coalinga and Atascadero state hospitals have suffered on average 2,795 assaults a year, costing California taxpayers over $82.7 million in workers’ compensation claims over the past two fiscal years alone, according to data obtained through state public records requests.
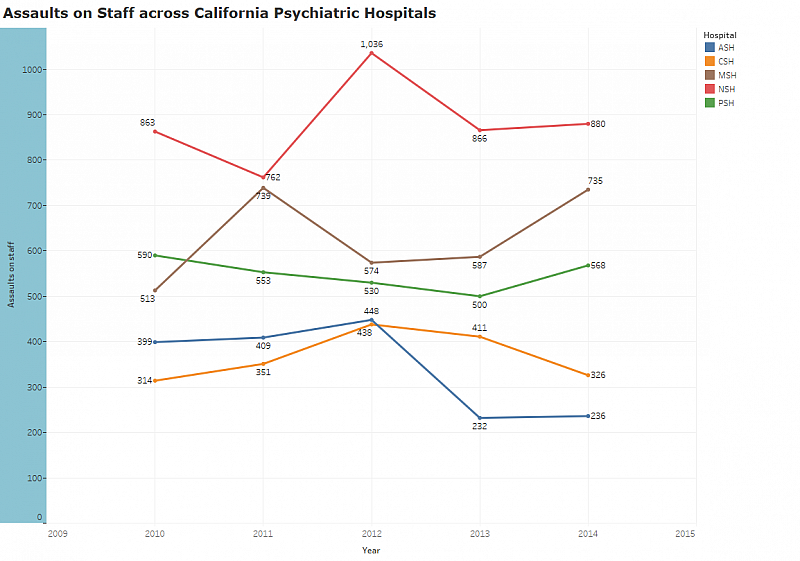
Patients at the five hospitals committed nearly 26,000 assaults between 2011 and 2014, the latest year for which data are available, according to aggressive incident report records obtained from the Department of State Hospitals, which oversees the facilities.
Staff were the victims of 11,000 — more than 42 percent — of those assaults, the records show. Psychiatric technicians, nurses and their colleagues sustained 2,745 assaults at the five facilities in 2014, nearly 150 more than the year before. In the past two fiscal years, 2013-14 and 2014-15, they lost 105,108 days of work, the equivalent of 473 full-time employees.
Workers at Napa State alone endured 880 assaults in 2014, up from 866 the previous year. Employees were routinely kicked in the chest, punched in the face, shoved against walls and knocked to the ground, police logs obtained through public records requests show.
If you look at the rate of assaults based on the number of staff working at the facilities, it looks like safety has improved. The chances of an employee getting assaulted peaked at 30 percent in 2012, compared with 24 percent in 2014. But those figures are misleading, union reps say. For one thing, paperwork requirements for assaults increased while hospitals were required to report to a federal monitor (which ended in 2013), and it was not uncommon for assaulted staff to suffer in silence rather than fill out more forms.
But perhaps more importantly, not everyone faces the same risks. Although any staff member runs the risk of a beating, says California Association of Psychiatric Technicians representative Coby Pizzotti, psych techs are especially vulnerable because they have the most contact with patients. The state doesn’t release the number of assaults on staff based on job category.
With 3,500 psych techs and over 2,700 assaults in a year, Pizzotti says, “It’s not a matter of if you get assaulted, it’s when you’re going to be assaulted and how severe.”
The year Gross was killed, staff at Napa State filed 289 workers’ comp claims, according to the Los Angeles Times. Over the past two fiscal years, that number jumped to 517 and 519, state records show. As the abuse continued, Seager says, staff and administrators acted like daily assaults were all in a day’s work. “It’s horrifying to me that no one does anything about it or even talks about it,” he says. “It’s not mentioned. Ever.”
Frustrated by this culture of silence and the state’s unwillingness to address the rampant violence in its hospitals, Seager documented the ongoing beatings in a 2014 book, “Behind the Gates of Gomorrah: A Year with the Criminally Insane.” He wrote the book, he says, because he wanted the public to know that the people they send to state hospitals to get treatment can’t get better in the midst of so much violence. And staff can’t deliver the care they were trained to provide when they’re constantly worried about their safety.
Hospital administrators weren’t happy about it, Seager says. But they didn’t fire him.
“The safety of our patients and staff has always been among our top priorities,” says Ralph Montano, spokesman for the Department of State Hospitals. Among recent safety improvements, Montano points to a new personal alarm system, which alerts police and reveals an employee’s location, indoors or out, and what he describes as key pieces of legislation signed by Gov. Jerry Brown in 2014.
The laws were designed to improve safety by giving clinical staff the right to access a patient’s criminal history for violence risk assessment and allowing medication orders to follow patients judged incompetent to stand trial. Patients can spend months in prison or jail without treatment before reaching the hospital, Seager says, increasing their risk for violent behavior.
Another law authorizes hospital officials to build enhanced treatment facilities, where the most dangerous patients receive treatment in secured areas as part of a pilot program. The department reported last year that a quarter of patients had been involved in aggressive incidents but only a fraction of them were considered “repeatedly violent patients.” The hope is that segregating those prone to violence will make the hospitals safer.
Hospitals Take on More Mentally Ill Patients Charged with Crimes
Napa State wasn’t always such a violent place. When psych tech Michael Jarschke started working at the hospital in 1972, most patients came to Napa because they couldn’t take care of themselves, not because they’d committed a crime. In those days, he’d sometimes get clobbered by patients beset by fits, but brutal beatings were rare.
More patients started coming to California’s state hospitals through the criminal justice system in the mid-1990s, Jarschke says, just before Donna Gross hired on at Napa State.
To ease overcrowding in prisons and jails, Napa and other state hospitals took on more mentally ill patients charged with crimes. In 1995, forensic patients, who have been convicted or accused of a felony linked to mental illness, made up 60 percent of patients in state facilities, state records show.
Today, 96 percent of the state’s psychiatric patients came through criminal courts — accounting for 37 percent of the nation’s criminally insane.
But staff weren’t trained to deal with “prison-minded” patients, says Jarschke, who served as president of the California Association of Psychiatric Technicians’ Napa chapter until May. Over time, he’d see more and more patients with gang affiliations, anti-social personality disorders and, like Jess Massey, predatory tendencies.
In the old days, Jarschke invited patients to his house for dinner, to help them feel normal. “That’s not happening here,” he says. “It’s not the same. It’ll never be the same.”
Jarschke soon realized the tools he used in a bike repair class could turn deadly in the wrong hands. But he felt strongly that he should keep teaching his patients skills that would boost their self-worth, so he set up a wheelchair repair program, thinking it would help them get a job when they got out. Some of his patients had committed monstrous crimes, but to him, they were people with mental problems, not criminals.
Jarschke had just set up a wheelchair repair program when Gross was killed. Even the wheelchair program was too risky, he realized. He shut it down.
The day after Gross’ murder, Jarschke and his colleagues formed the Safety Now Coalition to protect both staff and patients.
One of the first things they did was push for fully functional personal alarms and more security and clinical staff at the hospital. In 2012, administrators added a police substation within the secured treatment area outside, where Massey had cornered Gross. The following year, department spokesman Montano says, they finished implementing the alarm system.
But police aren’t on the wards when fights break out, so it’s up to staff, usually psych techs, to intervene. Most psych techs at California’s state hospitals are women who routinely find themselves trying to restrain men twice their size.
The alarms don’t prevent assaults, Seager says. “They simply allow people to get you medical help faster. We’ve had social workers have their teeth kicked in and bones broken. We’ve had head injuries where they’ve never come back.”
Workers often showed up for a shift having no idea there had just been a brutal assault. Last year, Seager says, “Someone was strangled and left for dead, and [the administration] never said anything about it.”
Safety Now asked administrators if staff at Napa could post a sign when a peer suffers an injury that requires more than local first aid, Jarschke says. The request was granted.
Subsidizing Violence on the Job
Lupe Alonzo-Diaz, the Department of State Hospitals deputy director of administrative services, acknowledged the risks staff face before a state oversight agency last year. “The potential to be assaulted is a daily threat for nursing staff,” she told the Little Hoover Commission, an independent agency that monitors and proposes improvements to state government operations.
The Department of State Hospitals defines aggressive acts as “hitting, pushing, kicking or similar acts directed against another individual to cause potential or actual injury.”
Verbal assault is not included in statistics released by the state, even though studies show that workers can suffer greater psychological effects from threats of violence than from physical aggression.
With so many battered workers unable to do their jobs (they’re out on worker’s comp due to the assaults), the Department of State Hospitals has asked psych techs and nurses to work more than 4.7 million hours of overtime — at time and a half — since 2012 to meet legal staffing requirements. Overtime hours for psych techs have increased more than a third since 2012, reaching 1.2 million hours last year at a cost of $53 million, Pizzotti testified before the Little Hoover Commission.
Nearly 150,000 overtime hours were mandatory during the 2014-15 fiscal year, up from 92,000 the previous year, state records show.
The union is fighting mandatory overtime, CAPT’s Pizzotti says, because it leaves workers unable to prepare for an extra shift, by going to bed early the night before or arranging day care for their kids. Sometimes employees don’t know until two hours before they’re scheduled to leave that they have to stay on, he says. “That throws your world into complete upheaval.”
California banned mandatory overtime for nurses in the private sector in 2001 because it compromises worker and patient safety. Since then,overwhelming evidence has linked long extended shifts to increased risks of clinical mistakes and higher rates of occupational injury.
Fatigued staff faced with the constant threat of assault are ill-prepared to safeguard their patients. Weak and vulnerable psychiatric patients sustained over 3,400 assaults at the hands of their peers in 2014, state records show. Although the numbers dropped nearly a quarter between 2010 and 2013, they jumped by 100 assaults in the following year.
Hospital administrators are forced to rely on mandatory overtime or face serious consequences, such as loss of certification, court sanctions and fines, Alonzo-Diaz told the Little Hoover Commission. It’s difficult to hire new staff, she said, because the risks associated with the work, combined with lower wages compared with private hospitals — as much as $63,000 less for nurses and $15,000 less for psych techs — make it hard to attract and retain employees.
Pizzotti says the state could solve these problems in part by expediting a hiring process that is so drawn out that job seekers find work elsewhere before they hear if they’re in the running.
Relief appeared to be on the horizon in August, when the Legislature passed SB 780, a bill prohibiting the state from using mandatory overtime as a staffing tool. But the bill was withdrawn after Gov. Jerry Brown signaled his opposition to the measure, Pizzotti says.
“We decided not to move the bill onto his desk, knowing that it would be vetoed,” he says. That means union representatives are back to bargaining with administrators to reduce mandatory overtime.
‘Everybody’s in the wrong place’
For psychiatrist Seager, improving safety over the long term requires coming to grips with the systemic failures that left state hospitals ill-equipped to deal with violent criminals. Homeless people with acute psychiatric conditions should be treated in state hospitals, he says, while the nonviolent mentally ill now in prisons and jails should be treated in community treatment centers and people convicted of violent crimes should be treated in prisons.
Instead, he says, “Every single person in the mental health care system is in the wrong place.”
Even so, the state could implement several reforms now. Every hospital should have enhanced treatment units as soon as possible, staff say, to protect workers and vulnerable patients from the subset of patients who commit the majority of assaults.
The state authorized funding for the program this year, and administrators expect to open units at Atascadero and Patton in 2018, says department spokesman Montano.
It could be several years before an enhanced unit comes to Napa. “That’s an ominous feeling for us,” says psych tech Jarschke.
For now, increasing staffing levels would go a long way toward reducing violence on the wards, union rep Pizzotti says. Last year, the Department of Public Health hit Napa with several citations for failing to protect patients, including one who sustained a head injury and another who suffered a broken jaw. According to police reports and sources, that’s almost inevitable when an alarm draws all hands from one unit, only to leave another unattended.
Taxpayers have been spending tens of millions of dollars a year in overtime that leaves workers exhausted, prone to making mistakes and even more vulnerable to injury, Pizzotti says. Last year, 18.4 million taxpayers filed with the California Franchise Tax Board. The money spent on overtime could have hired hundreds of full-time psych techs, he says, greatly reducing the risk of violence while allowing staff to focus on the therapeutic care they were trained to provide. It would have cost the average taxpayer less than the price of a latte at Starbucks.
But those positions remain unstaffed. Meanwhile, Seager says, the assaults at Napa grew bloodier and more frequent.
Next month marks the sixth anniversary of Donna Gross’ murder. This will be the first year Seager won’t be there to pay his respects. “I finally had enough of Napa,” he says. Seager left in June to freelance as an emergency services psychiatrist for several Bay Area hospitals.
“The medical care at Napa is first rate and the staff is terrific,” Seager says. “It’s just not safe.”
[This story was originally published by KQED.]

