Can California nursing homes avoid the next ‘humanitarian crisis?’
This story was produced as part of a larger project by Brenda Gazzar, a participant in the 2020 California Fellowship.
Her other stories include:
'This isn't a drill': How LA's Motion Picture home battled coronavirus
‘Pandemic within a pandemic:’ What’s fueling LA County’s coronavirus death toll in nursing homes?
Known and loved: These six residents of LA’s Motion Picture home died of coronavirus
‘Behind the 8-ball:’ Many Southern California nursing homes hit hard by coronavirus had prior issues
A tale of two Southern California nursing homes in the era of coronavirus
Family of nursing home resident who died: ‘She had 3 really good years there and 1 really bad week’
Social isolation takes toll on Southern California nursing home residents during pandemic holidays
This nursing home ‘angel’ struggled to support her family. Then she got coronavirus…

Marisela Munoz holds a photo of her aunt, Evangelina C. Martinez, who raised her since birth, at her home in Canyon Country, Friday Aug. 28, 2020. Martinez, who was a resident at Astoria Nursing and Rehabilitation Center in Sylmar, died after becoming ill with COVID-19 at the age of 93.
(Photo by Hans Gutknecht, Los Angeles Daily News/SCNG)
Marisela Muñoz never wanted to see the woman who raised her since birth land in a nursing home.
But Evangelina C. Martinez, who was Munoz’s aunt but whom she considered her mother, had Alzheimer’s and needed around-the-clock care that Muñoz and her siblings could no longer provide. So eight years ago, they placed the elderly woman at Astoria Nursing and Rehabilitation Center in Los Angeles’ Sylmar community.
“Mama Eva” ultimately did well at the 218-bed home, joking with her favorite caregivers and persuading one of them to regularly buy her a can of Coca-Cola to share, said Muñoz, a resident of Canyon Country in Santa Clarita.
Then, in mid-April, the facility informed Muñoz that a few residents at Astoria had tested positive for the novel coronavirus.
“They said … ‘Everything’s under control. We took the (COVID-19 positive) patients to the hospital there. (Martinez) was nowhere near the two positive patients,’ ” Muñoz recalled of her worried phone call to the facility the next day.
But in subsequent weeks, Muñoz realized that the virus had triggered a broad outbreak at the nursing home, followed by Martinez’s death.
Marisela Munoz looks at a photo of her aunt, Evangelina C. Martinez, who raised her since birth, at her home in Canyon Country, Friday Aug. 28, 2020. Martinez, a resident of Astoria Nursing and Rehabilitation Center in Sylmar, died after becoming ill with COVID-19 at the age of 93. (Photo by Hans Gutknecht, Los Angeles Daily News/SCNG)
Meanwhile, California Department of Public Health records reveal a disorderly and fear-ridden environment at the Sylmar home.
On April 23, three months after the state’s first coronavirus case, an unidentified Astoria resident who had tested positive for the virus told state surveyors she had been placed in a room by herself and did not receive care until she was about to be transferred to the hospital at noon.
The resident told surveyors that “nursing staff did not check on her nor serve her breakfast that morning,” according to state deficiency records. She “stated she felt helpless and alone.”
Workers “were scared of the resident” because of her COVID-19 status and “the facility should have been prepared,” Astoria’s infection preventionist nurse told surveyors.
Astoria’s administrator also acknowledged that the facility “was not ready to care for COVID-19 residents,” according to the records.
Some 85 residents and nearly 70 healthcare workers at Astoria Nursing and Rehabilitation Center had contracted the virus as of Dec. 11, according to Los Angeles County records. Twenty of the infected residents died, including 93-year-old Martinez.
Astoria Nursing and Rehabilitation Center in Sylmar. (Photo by Hans Gutknecht, Los Angeles Daily News/SCNG)
A spokeswoman for the two-star (or below average) quality rated facility could not be reached after scheduling a time to speak with a reporter from the Southern California News Group. Several subsequent attempts to reach her and the home’s administrator by phone, text and email went unanswered.
“It makes me upset because who knows how long my mother could have lived … if they were better prepared or they might have taken other steps to prevent it?” Muñoz said.
A holistic approach
New state laws require nursing homes to store personal protective equipment in the future and employ a full-time infection preventionist, moves applauded by advocates as vital steps. But it’s also clear that preparing the troubled nursing home industry for the next pandemic will require a holistic approach.
The federal government required nursing homes to create plans for all kinds of hazards, including infectious disease threats, by mid-November of 2017. The rules included having regular emergency preparedness training and drills.
Before then, nursing homes were required to have “very minimal emergency plans in place and they were more about evacuation rather than … looking at every type of risk there is,” said Jason Belden, director of emergency preparedness at the California Association of Health Facilities, which represents more than 900 skilled nursing facilities.
Jason Belden, director of emergency preparedness and physical plant services at the California Association of Health Facilities. (Photo courtesy Jason Belden)
So why were nursing homes in California unprepared for the coronavirus pandemic?
The primary focus of state and local officials in recent years had been protecting nursing home residents from wildfires and, to a lesser degree, floods, Belden said. Meanwhile, each health care facility prioritizes with local jurisdictions the risks they believe are most likely to occur.
Pandemic planning probably wasn’t No. 1 on the list for nursing homes or even hospitals, he said.
“After 2020, I imagine it probably will be No. 1 for everybody,” Belden said.
Moreover, the state’s pandemic plan prior to the pandemic called for nursing homes to accept patients from hospitals in case of patient surges, he said. That doesn’t work with this virus, however, because nursing home residents “are vastly more susceptible to negative outcomes if they get COVID.”
Further complicating matters were conflicting messages and guidance from a host of federal, state and local agencies — as well as from various associations — on issues such as wearing masks, hampering nursing homes’ response to the crisis, Belden said.
“That absolutely, without a doubt, unequivocally has to change,” he said.
Staffing ‘the major factor’
Since March, California nursing homes have faced “a humanitarian crisis,” said Charlene Harrington, a nursing and sociology professor emerita at UC San Francisco. While nursing home residents make up less than 1 percent of the state’s population, they comprise more than a quarter of all COVID-19-related deaths in the state.
Harrington and her colleagues have found through their research that nurse staffing levels are “the major factor that prevent COVID infections and deaths.”
Charlene Harrington, a nursing and sociology professor emerita at UC San Francisco. (Photo courtesy Charlene Harrington)
California’s minimum staffing standard of 3.5 hours of direct patient care per nursing home resident per day “is simply too low” to protect residents, Harrington said at a state Assembly budget subcommittee hearing on Oct. 28.
Meanwhile, homes are circumventing that standard with waivers granted by the state.
“We urge increasing the state’s minimum staffing law to 4.1 hours per resident per day for total nursing, including 45 minutes of RN time (per patient) and 24-hour RN coverage,” she said.
Currently, only California nursing homes with at least 100 beds are required to have a registered nurse on site at all times.
Assemblyman Jim Wood, who chairs the Assembly Health Committee, said he was both “kind of appalled” and “shocked” to learn that was the case.
“I just can’t help but think that a change in that direction would be a dramatic potential improvement in the quality of care and the quality of health of the residents so that something early can be caught,” Wood, D-Santa Rosa, said at the hearing.
The California Department of Public Health is working to develop new staffing strategies, including targeting infection control strike teams to facilities with short staffing, testified Heidi Steinecker, a deputy director at the state agency.
Another strategy is to have surveyors reassess emergency staffing waivers for facilities that haven’t provided adequate safe staffing level plans or maintained safe environments, she said.
Meanwhile, yearly turnover of nursing home administrators and directors of nursing can be as high as 40 percent or more, according to some surveys, which experts say affects the quality of care and staff morale.
A push for more pay
UCSF’s Harrington also urged state lawmakers to require a 15 percent increase in nursing assistant wages in the coming year to reduce turnover — which can cause higher COVID-19 infection rates — and staffing shortages.
Nicole Howell, executive director of Ombudsman Services of Contra Costa, Solano and Alameda counties, agreed that facilities should be required to “immediately raise compensation” for certified nursing assistants and caregivers. She suggested 30 percent, or about $3 an hour.
On average, direct care workers earn only $1 to $2 more per hour than minimum wage — often working 60 to 80 hours per week — “to do the most critical work that we have to care for older and disabled adults,” Howell said at the hearing.
Deborah Pacyna of the California Association of Health Facilities said nursing home workers deserve more pay. But about 70 percent of nursing home residents are Medi-Cal patients and the reimbursement rate “doesn’t cover the cost of care.”
“To the extent we could get more money from the state in a Medi-Cal reimbursement, we can pass that money on to our deserving staff,” Pacyna said in an interview.
She noted that the average operating profit margin per long-term care facility in California was 1.1% in 2018, according to California’s Office of Statewide Health Planning and Development Training.
Even with annual reimbursement rate increases, Medi-Cal “does not reimburse facilities for their actual costs so there is a continual shortfall,” Pacyna said, adding that labor costs are reimbursed at 95 percent and other costs are reimbursed less.Assemblyman Wood, however, argued that some players in the industry are making “huge profits.” Perhaps nursing homes could be required to use funding from future Medi-Cal rate increases for increasing wages to their hard-working staff, he said.
“That’s never happened, as far as I’m aware,” he said in an interview. “The whole issue (of staffing and wages) has really reared its ugly head during the crisis.”
A military approach?
Pandemic plans are worthless if there’s no structure or function to execute them, said Dr. Michael Wasserman, immediate past president of the California Association of Long Term Care Medicine.
“I often look to the military for the most effective examples of crisis management,” said Wasserman, who used to run the state’s largest for-profit nursing home chain and is currently medical director of a senior care home in Reseda. “Having a clear chain of command and clearly defined roles and responsibilities are absolutely essential during a crisis.”
Dr. Michael Wasserman is a geriatrician and immediate past president of the California Association of Long Term Care Medicine. (Photo by Michael Owen Baker, contributing photographer)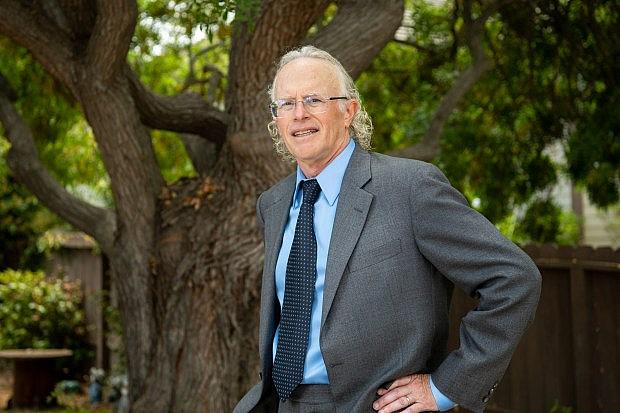
Having a competent and engaged medical director to work with staff — while guiding administrators who have little clinical expertise — is also critical in battling infectious diseases, he said at the Assembly subcommittee hearing.
The state should require medical directors to get certified to ensure they have the skills, tools and professional obligation to provide qualified oversight of nursing home care, he said.
“If every nursing home in the state had a certified medical director over the past eight months … and in conjunction with the appropriate nurse staffing levels, far fewer nursing home residents would have died,” he testified.
When asked by this newsgroup, state public health officials did not acknowledge any geriatricians or long term care medicine professionals on the task force. But they said in an October email that the task force “works closely with dozens of subject matter experts from within (the) state government and private sector.”
Infection control
Advocates are calling for better enforcement of infection control standards at these homes.
Instead of being treated as “an afterthought,” such violations require both higher and more consistent fines, said Tony Chicotel of California Advocates for Nursing Home Reform.
“We need to … have basically a zero-tolerance policy on violations,” he said in an interview.
The Legislature could determine a minimum penalty for such violations instead of leaving it to the discretion of the enforcement agency, he said. It’s also important to have different surveyors visit a nursing home over time so that they don’t get too chummy with staff, Chicotel said.
CANHR recently criticized a recently implemented California Department of Public Health plan whereby surveyors visit these homes at least every six to eight weeks. The advocacy group has argued that it will “divert the surveyor workforce” from investigating an “enormous backlog of complaints” on nursing home abuse and neglect.
Before the pandemic, California Department of Public Health surveyors entered facilities they monitor on an annual basis, said Steinecker, the agency’s deputy director.
“If we learned anything, it’s not enough,” she told the Assembly budget subcommittee hearing. “We learned being physically present in these facilities more often garners better compliance.”
The Center for Medicare and Medicaid Services, which oversees the quality of nursing homes at the federal level, recently provided technical training and assistance to CDPH staff on maximizing “federal regulations which are stricter in regards to infection control processes,” Steinecker testified.
The state public health agency also is partnering with other agencies, including Cal-OSHA, to expand its predictive analytics data concerning outbreaks, she said.
“Some of the most recent outbreaks that have happened are due to violations not necessarily under CDPH jurisdiction but out of violations from our partners’ compliance and regulations,” Steinecker said.
Testing
Dr. Matthew Zahn, medical director of communicable disease control at the Orange County Health Care Agency, noted earlier in the pandemic that he was pleased to have its public lab focused on nursing homes. But the lab lacked capacity.
Dr. Matthew Zahn, medical director of communicable disease control at the Orange County Health Care Agency. (Photo by Leonard Ortiz, Orange County Register/SCNG)
“I think we need to have more of a process where testing of patients and screening of patients happen through commercial labs because the capacity through commercial labs is so much greater,” Zahn said in May.
For several months now, the county’s public health lab has been providing testing with nursing homes as needed for COVID-19 outbreaks, while nursing homes are using commercial labs for their routine testing of employees and residents, officials said.
Public health labs across the state were not equipped to handle the influx of testing needed and long turnaround times made these results less useful.
Early in the pandemic, local health labs had only enough capacity to run 10 to 12 test kits a day, Sen. Richard Pan, D-Sacramento, said in an interview.
Giving more dollars to public health, which has seen significant cuts in recent years, could help bolster the capacity of public health labs, allow for needed contact tracing and curb testing agent shortages, said Pan, a pediatrician who chairs the Senate Health Committee.
Meanwhile, Gov. Gavin Newson announced in late October the opening of a $25 million lab in Valencia, built with diagnostics company PerkinElmer, that’s expected to process 150,000 diagnostic tests upon reaching full capacity by March.
‘They’re still people’
Despite waiting for hours outside the Astoria nursing home on an early May morning, Muñoz didn’t get to see the woman who was essentially her mother before she was taken to the hospital.
“I kind of got really upset because at least that was my chance … to at least let her know that we were there,” she said, noting the elderly woman had been wheeled out from the back after Muñoz notified an employee of her presence.
Muñoz then went to Glendale Memorial Hospital, where she could see through a window that Martinez had difficulty breathing.About a week later, when doctors were hoping to transfer Martinez to hospice, Muñoz was able to visit her in the hospital for 15 minutes. During that visit, Martinez tried to squeeze her hand — something she always did with her when she was afraid, Muñoz said.
“All I could do was tell her that I loved her and it was OK for her to go,” she recalled, her voice cracking with emotion.
Martinez, who also had pneumonia, died two days later.
Now, Muñoz and her family are left with only photos, videos and mementos of “Mama Eva,” who with her late husband raised eight children — four of whom were her nieces. As Astoria Nursing and Rehabilitation Center faces more state and federal deficiencies, she fears that the elderly will continue to be forgotten and “thought of as disposable.”
“I know that (preparedness) takes time and it takes a lot of money, but whether our family members might be 20 years old or 90 years old … they’re still people,” Muñoz said. “They still have feelings.”
This article was produced as part of a project for the USC Center for Health Journalism’s California Fellowship.
[This story was originally published by The Press-Enterprise.]

