‘I Don’t Have Faith in Doctors Anymore.’ Women Say They Were Pressured Into Long-Term Birth Control
The story was originally published in TIME, with support from our 2023 Impact Fund for Reporting on Health Equity and Health Systems.

(From top) Rauslyn Adams, Miannica Frison and Crystina Hughes in Birmingham, Ala., on April 27, 2024.
Nydia Blas for TIME
Miannica Frison was in the throes of labor in 2020 when a nurse entered her room at UAB Hospital in Birmingham, Ala. Frison was screaming in pain. But rather than see how she could help, Frison recalls, the nurse said she heard Frison was having her third baby, and asked if she wanted to be sterilized immediately after she gave birth. Outraged, Frison kicked the nurse out of the room.
Doctors eventually told Frison she needed an emergency C-section. As she lay on the operating table, just moments after her son was pulled from her belly, a doctor entered the delivery room. “We can go ahead and put an IUD in right now, since you’re already open,” the doctor said, according to both Frison and her husband.
Frison was woozy from her epidural, but had experienced a traumatic birth, and at that moment, she didn’t think she wanted more children. So she allowed the doctor to insert the Mirena, an intrauterine device (IUD) that would prevent pregnancies for up to eight years. In the months that followed, she didn’t like the way the IUD was making her feel. But Frison says she couldn’t persuade her gynecologist to take it out. The doctor told her she needed to lose weight first, Frison recalls, and that there were medicines to offset the side effects she was experiencing, such as nausea.
It would be three years before Frison could get the device removed. Even then, she had to undergo three procedures, one lasting seven hours, she says, because the device had migrated to the lining of her uterus. It left her with four thumb-sized scars on her belly from where a doctor inserted an instrument to try to find the IUD. The experience caused Frison, a 32-year-old hairdresser, to have a profound mistrust of the medical system. “I don’t have faith in doctors anymore,” she says. “I can’t trust any of them.”
Frison’s experience was more common than one might expect. In the last two decades, doctors have encouraged women to choose long-acting reversible contraceptives, or LARCs, because they are the most effective method of preventing unplanned pregnancies. Doctors and many patients like that LARCs–either IUDs, which are inserted in a woman’s uterus, or implants, which are inserted in a woman’s arm–allow women to “set it and forget it” for years. But an increasing body of evidence indicates that an important public health tool intended to give women agency over their bodies is at times deployed in ways that take it away.

"I don't have faith in doctors anymore," Frison says.
Nydia Blas for TIME
A TIME investigation based on patient testimonials, medical studies, and interviews with 19 experts in the field of reproductive justice, including physicians, researchers, and advocates, found that doctors are disproportionately likely to push these contraceptives when treating Black, Latina, young, and low-income women, or to refuse to remove them when requested. This pattern, reproductive-justice experts say, reflects the race and class biases plaguing the U.S. medical system and extends a sordid and long-standing history of America’s attempts to engineer who reproduces. It also reflects what appears to be a broad push by policymakers to use birth control as a tool to curb poverty.
“The idea is that we can stop people that we don’t want to be reproducing from reproducing, but can say, ‘This is temporary because it’s removable,’” says Della Winters, a professor at California State University, Stanislaus who has studied the history of LARCs and calls the rise of so-called provider-controlled contraception targeting certain populations a type of “soft sterilization.”
Doctors pressuring patients into getting LARCs is a national phenomenon, experts say, but it may be especially prevalent in the South, where there is a troubling history of reproductive control. To explore what women are experiencing, TIME spoke with 10 women in Alabama, including four patients at UAB Hospital, who said they were pressured to get an IUD postpartum or had their doctors refuse to remove the devices when they initially asked. Four doulas who work in the state told TIME they’d witnessed doctors pressure Black women, especially those on Medicaid, into getting IUDs by asking them repeatedly during birth—but not, according to their clients, prior to it—about their preferred birth-control method and then strongly suggesting an IUD.
UAB disputed that it engages in reproductive coercion and said in an email that it follows guidance from the American College of Obstetricians and Gynecologists (ACOG), which suggests that LARCs should be offered immediately postpartum as standard care. The hospital also says that its providers receive implicit-bias training to avoid disparities in maternal and infant health outcomes. Patients are counseled on contraception options throughout the course of their pregnancy, the hospital says, and “every patient makes her own decision on contraception, and our team supports them in the decisions they make about their health.” Federal privacy laws prohibit UAB from commenting on an individual patient’s care, UAB says.
The ACOG says its recommendation for doctors to offer immediate postpartum LARCs refers to women who have already selected an implant or IUD as their contraceptive method. Though the group previously recommended that doctors emphasize LARCs as the most effective contraceptive, it said in 2022 that it now recommends a “patient-centered” approach to contraceptive counseling. (The Alabama patients who spoke to TIME shared experiences that took place between 2016 and 2023.)
Doctors who pressure patients to get or keep LARCs may do so because they think they’re acting in the patients’ best interest, says Nikki B. Zite, an ob-gyn and professor at the University of Tennessee Graduate School of Medicine. They might advocate for women with substance-abuse problems or major health issues to get a LARC, Zite adds, because they want them to be healthy before they give birth, or might hesitate to take out a LARC because they know the devices are expensive for insurers, and that symptoms a woman experiences after insertion, like cramps or bleeding, will pass. Zite remembers being extremely enthusiastic when she first started recommending LARCs to patients in the early 2000s. Now she recognizes that could have come across as coercive. “If a patient came to me for diabetes, I would want them on insulin—that’s the most effective treatment,” she says. “I have a chart showing that LARCs are the most effective form of contraception, so doctors think, ‘Why wouldn’t I want them using a LARC?’ The answer is that reproductive health is different.”
Even if they have good intentions, doctors, in their enthusiasm for effective birth control, may strong-arm certain women into getting and keeping contraceptive methods they don’t want. TIME examined 14 separate peer-reviewed studies in which Black and Latina women and lower-income patients reported experiencing higher levels of coercion from doctors to use LARCs. In one 2022 paper that reviewed a survey of nearly 2,000 women in Delaware and Maryland, about 26% said they were pressured to get their LARC, and low-income women on Medicaid were more likely than higher-income women to feel pressured to keep it. A separate 2022 study of more than 2,000 adolescents found that Black girls were twice as likely as white ones to receive LARCs.
In five additional studies reviewed by TIME, doctors admitted either to resisting some patients’ requests to remove LARCs or to pushing certain populations toward LARCs because they didn’t trust them to avoid a pregnancy that the doctor viewed as undesirable. “The other thing that really frustrates the crap out of me,” one doctor told researchers, according to a study published in 2021, “is the patient who comes in and says, ‘No, I don’t want to be pregnant, but I don’t use any birth control.’ You want to take that person and shake them. Some of it is ignorance, some of it is cultural.”
In the wake of the Supreme Court’s 2022 Dobbs decision, which overturned the constitutional right to an abortion, the question of just how widespread this pressure may be takes on greater urgency. Research shows that doctors in states with restrictive abortion laws are redoubling their emphasis on the use of LARCs. These may be well-meaning attempts to help women and teens avoid a pregnancy they don’t want and would not have the option to terminate. But reproductive-justice advocates say pushing LARCs on poor women or women of color is also a form of reproductive control. It can not only strip patients of autonomy over their bodies, but also erode their trust in medical providers, causing them to withdraw from care and eschew birth control altogether.
"This is when the culture of medicine that centers providers’ perspectives over those of patients has its absolute worst impact," says Christine Dehlendorf, a physician and professor at the University of California, San Francisco, who was one of the first to study how provider bias affects LARC counseling. "We are explicitly able to take away people's autonomy by refusing to remove contraceptive methods, but all the time, providers can believe that they're doing the best thing for the patient, and that they know better."

UAB Hospital in Birmingham, Ala.
Nydia Blas for TIME
LeAnn, a stay-at-home mom from Tuscaloosa, Ala., was on Medicaid when she gave birth to her second child in 2018, at age 20. Her doctor kept asking her about her plans for contraception after she gave birth, says LeAnn, who did not want her real name used to protect her privacy. She eventually agreed to get the Mirena inserted at her six-week postpartum visit.
Almost immediately, LeAnn says, she started waking up in the middle of the night with uterine pain so severe that she couldn’t stand up straight. After three months of pain, she says she asked her doctor to remove the IUD, but he refused, saying she needed to choose another form of birth control. The pain was so bad, LeAnn recalls, that she would sometimes end up in the emergency room. “I just suffered for a year,” she says. Finally she decided the best strategy was to lie and tell her doctor that she wanted another baby; with that, he removed the IUD.
LeAnn is white, but says her doctor knew she was on Medicaid. Research suggests that doctors are often hesitant to remove IUDs in women who they know are poor or who have children at home. A 2016 study found that 1 in 4 women who went to a Bronx, N.Y., clinic asking doctors to remove their IUDs were not successful. “These ideas of who should and shouldn’t have children are still very much influencing our policies and practices, even if it’s more subtle than in the past,” says Mieke Eeckhaut, a sociologist at the University of Delaware, who found that young, economically disadvantaged, unmarried, and Hispanic women disproportionately reported being pressured to keep their LARCs.
Systemic racism and classism have long pervaded the American medical system, including reproduction. Before birth-control methods like the pill and IUDs were legally available, policymakers used sterilization to prevent certain “low-status” women from having children. Laws permitting states to sterilize women whom lawmakers thought would be unfit parents were so common throughout the South that the civil-rights activist Fannie Lou Hamer coined the term “Mississippi Appendectomy” after she went to have a uterine tumor removed and unknowingly got a hysterectomy instead.
Advances in birth control in the 1950s gave women more options, but it also gave doctors a measure of control over who got pregnant. Margaret Sanger, the founder of Planned Parenthood, promoted the pill in part as a way to limit reproduction in “defective” populations. After the FDA approved the Norplant, a small contraceptive rod implanted in a woman’s upper arm, in 1990, states began pushing the device on low-income Black women, incentivizing welfare recipients with cash bonuses.
In the 2000s, pharmaceutical companies started rolling out a new wave of extremely effective hormonal IUDs, including the Mirena. To doctors, these devices, alongside safer implants introduced in the late 1990s, were something of a miracle. With one short insertion procedure, they could help women avoid pregnancies for long periods of time. (The duration of each device varies, but they generally last from about three to 10 years.) LARCs are not only 20 times more effective than the pill. They also offer the promise of convenience: no more worrying about picking up a prescription from a pharmacy on a regular basis, or remembering to take the medication at the same time every day.
But as these devices entered the market, American women stayed away from them—just 5% used them in the late 2000s, compared to 19% of women in places like Sweden. This reticence prompted doctors to launch a campaign to market LARCs to women perceived to be at risk of unplanned pregnancy, a policy fixation in the wake of the welfare-reform push during the Clinton Administration. In 2007, an anonymous funder—Bloomberg later reported that it was the Susan Thompson Buffett Foundation—approached researchers at Washington University in St. Louis with a goal: promoting and providing the most effective contraception in an effort to prevent unintended pregnancies. They launched the Contraceptive CHOICE project, which recruited women “at the highest risk for unintended pregnancy”—a group they defined as minorities, poor women, and women under 25.
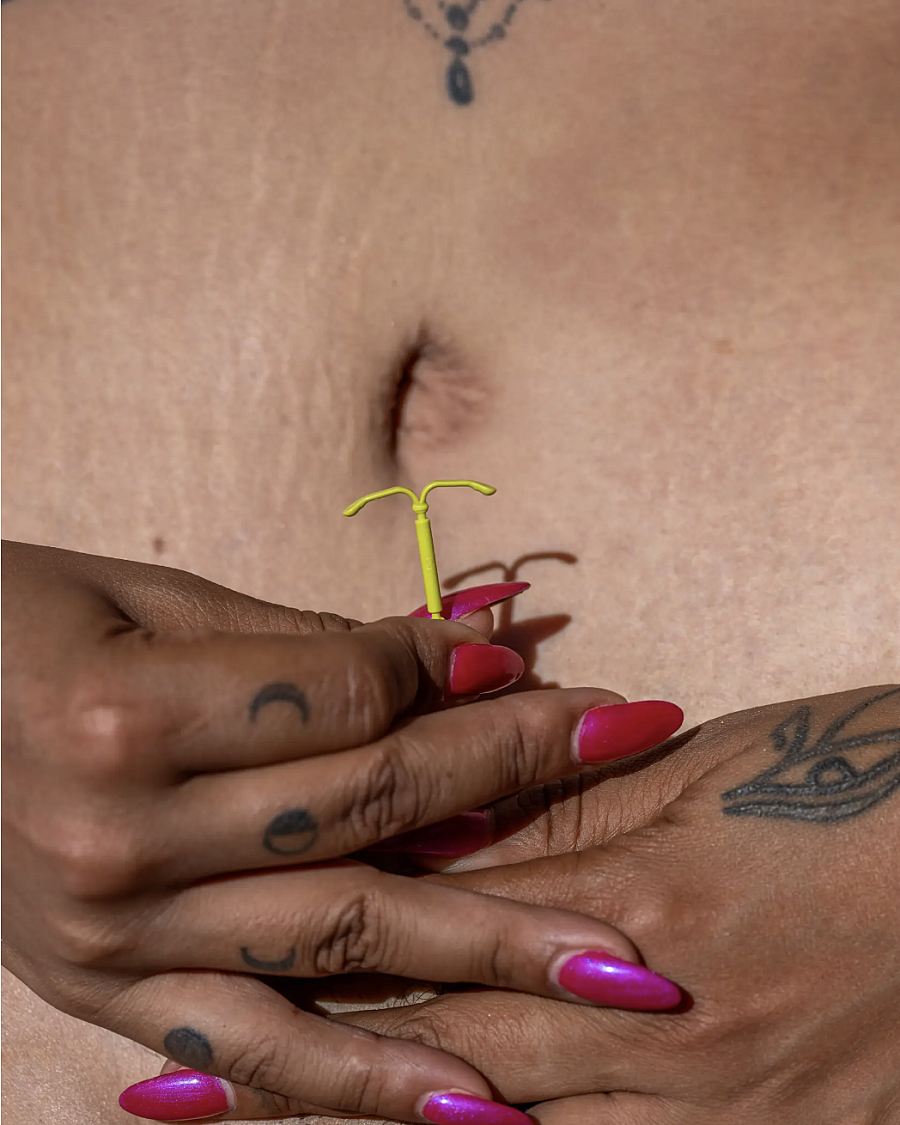
A Mirena IUD.
Nydia Blas for TIME
The CHOICE project did not ask those women which type of birth control best fit their lifestyles, or if they were seeking a method that they could stop on their own without a doctor’s assistance. Instead, doctors used a standardized script to counsel women that LARCs were the most effective contraceptive and that they could receive the devices for free. As a result, 75% of the women in the program chose a LARC, compared to just 5% of women attending the same clinics before the CHOICE counseling was launched, according to a study of the project, which included 9,256 women.
The initial results, published in 2010, were a watershed in reproductive health. Counseling women to choose LARCs appeared to be a relatively simple way to prevent unintended pregnancies, and CHOICE researchers trumpeted the potential to save U.S. taxpayers $11 billion annually in costs associated with unintended births. Policymakers and philanthropists hailed LARCs as a “silver bullet” that would reduce unintended pregnancies and save states huge sums in public benefit costs. The Susan Thompson Buffett Foundation reportedly put $200 million into research and promotion of IUDs. (The foundation did not respond to a request for comment.) Public health groups like the American Academy of Pediatrics and ACOG launched “LARC-first” campaigns to increase uptake. The World Health Organization and Centers for Disease Control and Prevention launched a “tiered effectiveness” model urging doctors to talk about LARCs and sterilization as the best way to prevent pregnancy. Many providers were also counseled to ask women “one key question”: whether they were planning on getting pregnant within a year. If the answer was no, doctors were supposed to suggest LARCs.
Informing women about their contraceptive choices is a laudable goal. So is ensuring access for women who may not be able to afford them otherwise. (Since the passage of the Affordable Care Act, insurers have been required to cover contraception; Medicaid also covers the cost of contraception for lower-income women.) But experts say the LARC-first campaigns become problematic when doctors focus on effectiveness to the exclusion of other factors, including the ability to start and stop birth control when women desire. “There’s been a lot of targeted information about LARCs, which is great if that’s what the patient wants,” says Kavita Shah Arora, the division director of the ob-gyn department at the University of North Carolina at Chapel Hill. “If we’re pushing people into a form of birth control that they don’t want, that is not great.”
States like Delaware and Colorado launched programs to increase access to birth control, offering a range of contraceptive options but emphasizing the effectiveness of LARCs. Colorado said in 2017 that it saved nearly $70 million in public-assistance costs because of LARCs. “Better birth outcomes, a reduced teenage birthrate and millions of dollars saved are cause for celebration,” Delaware Governor Jack Markell, a Democrat, wrote in a 2016 New York Times op-ed about his state’s efforts to promote LARCs and save taxpayers money.
But the notion of fighting poverty and saving money by reducing unplanned pregnancies misses a big point: poverty is not caused by pregnancy. Many women are poor when they get pregnant because of entrenched social issues. Advising them to wait for a better time to have a baby implies that women who are poor shouldn’t procreate. Saying that unplanned pregnancies cause poverty “stigmatizes poor women, especially poor women of color, and blames them for profound inequality that’s actually caused by things like lack of access to meaningful employment or safe schools,” says Patrick Grzanka, a psychology professor at the University of Tennessee who has studied LARC coercion.
Alarmed by efforts to target LARCs at low-income populations, a group of women’s health organizations led by Sister Song, a nonprofit dedicated to reproductive justice for women of color, put out a statement of principles about LARCs in 2016. They warned that as funders set targets for the number of LARCs inserted, women reported being talked down to and undermined by doctors, who “treat them as though they do not have the basic human right to determine what happens with their bodies.” The group rejected efforts to direct women to any particular method and cautioned providers against making assumptions based on race, ethnicity, age, or economic status.
The statement was endorsed by more than 150 organizations, but it’s taken a while for actual practices to change. That’s partly because many doctors were trained in a LARC-first approach and might not know that there are new recommendations about how to talk about contraception. Indeed, ACOG recently issued new guidance that eschewed a LARC-first approach and recommended patient-centered contraceptive counseling. But one recent study found that even some medical providers who said they were embracing this approach nonetheless rejected patients’ requests to have their LARCs removed.
“I’ll never just walk in a room, “Oh, we’re just taking the IUD out?’” one medical provider told researchers about the limitations of patient-centered care. “Sometimes I’ll get them to, ‘Let me just examine you, do some cultures, let me do an ultrasound and make sure it’s in the right position.’ And then secretly I know I’m not going to fix their bleeding, but secretly I’m hoping that they’ll just leave and not come back in … or they just can’t get back in to get it removed and things will calm down.”

"It really took me becoming a doula to realize that I was coerced into getting the IUD,” Crystina Hughes says.
Nydia Blas for TIME
Charity Howard, a doula in Alabama, says there’s a striking difference in what happens to different types of women when they go to the hospital to give birth. Black women on Medicaid are asked to consent to having an IUD inserted immediately postpartum, according to Howard. But "when they have private insurance," she adds, "they don’t run into this issue.” Doctors can be persistent, according to Howard, who says she witnessed a doctor at UAB persuade one of Howard’s clients, a lesbian who was pregnant from a sperm donor, to get an IUD, even though the woman was not at risk of an unintended pregnancy. When Howard protested, she says she was escorted out of the hospital. (In its statement to TIME, UAB said it could not comment on individual patients.)
When Crystina Hughes went to UAB in 2019 to give birth, she planned to wait until her six-week follow-up appointment before deciding on a form of birth control. But as soon as her daughter was born, Hughes says, a doctor asked if she wanted to get an IUD inserted, noting her cervix was already dilated. Hughes says she declined, but when her husband went with her newborn daughter to the ICU, the doctor returned to ask again.
Hughes, who is Black, reasoned that if the doctor asked twice, it had to be important. So she agreed. Her milk dried up around six weeks, and she had to have the IUD removed within a year because of a prolapsed uterus, says Hughes, 35, who has since become a doula. Hughes says she often sees her clients pressured into getting LARCs, once even while doctors were weighing a woman’s newborn. “It really took me becoming a doula to realize that I was coerced into getting the IUD,” says Hughes. “It’s like, ‘Can you let her have 24 hours before you ask her if she’s thinking about birth control?’” (UAB says that it provides equal care to all patients, regardless of their gender, sexual orientation, race, or religion, and that to not offer a patient contraception based on their sexual orientation would be discriminatory.)
There are reasons a doctor might want to insert an IUD right after a woman gives birth. The patient may already be on pain medication, so it won’t hurt as much, and she’s less likely to come back pregnant with another baby in a few months. Some women on Medicaid also lose their coverage soon after they give birth, which could be another reason doctors push IUDs on them and not others. Studies have found that IUDs are more likely to fall out or migrate if they’re inserted immediately postpartum, but ACOG says that it has reviewed “cost-benefit analysis data” that suggests placing IUDs right after a woman has given birth is the best approach, “especially for women at greatest risk of not attending the postpartum follow-up visit.” Still, reproductive-justice advocates say that pressuring a woman after the enormous challenge of childbirth, when she may be less likely to resist, is problematic. And they warn that ACOG’s criteria means doctors may pitch LARCs differently based on their biases about who they think will—or won’t— show up for a follow-up visit.
Some of the discrepancy in who is directed to LARCs is also built into the health care system. Medicaid covers the postpartum IUD insertions in many states, while private insurance doesn’t, in part because of the higher expulsion rate for devices placed at this time. Hospitals are also often compensated by one lump sum, called the global fee, for a woman’s pregnancy and delivery care, which means they can lose money if they pay for and insert a LARC postpartum as part of that care. Since 2012, however, 43 states have altered their Medicaid policy so that hospitals could receive extra compensation for inserting an IUD or implant immediately after a woman gave birth, a change that may have incentivized hospitals to push this particular method of contraception on women with Medicaid but not others.
A study of the program in South Carolina, which adopted this policy in 2012, found that some women were dissatisfied with how providers talked to them about LARCs. Three out of 10 women who received a postpartum LARC later tried to get it removed, but encountered problems, the study found. “They just keep promoting these long-term methods,” one Black woman told researchers, recalling her encounters with doctors during her hospital stay. “It’s like they’re getting a commission or something.”
The pressure doesn’t necessarily stop after delivery. When Rauslyn Adams gave birth at UAB in 2016, she says she was told that she would lose access to Medicaid if she didn’t get an IUD—which, she says, she later found out was untrue. Not wanting to lose her health care, Adams agreed to get the Mirena at her six-week postpartum visit. Adams says her milk production slowed soon after she got it. When she asked a doctor to take it out, the doctor refused, Adams says. When she successfully pleaded with another doctor to remove the device, she says, her milk supply improved. “They really treated me like a dumb poor Black woman,” says Adams, who went back to UAB twice to complain in the months after she gave birth. (UAB says that all patients are counseled on contraception and options available to them throughout their pregnancy, and that these conversations are documented and confirmed when they are admitted to the hospital. Consent forms are signed for the chosen plan, the hospital says.)
Power dynamics in the South sometimes make Black women feel like they can’t refuse doctors’ recommendations, says Aisha Prewitt, a doula who works with women in Birmingham and who has observed postpartum coercion. “They will say, ‘It’s not coercion, it’s birth control,’” Prewitt says. “But they’re not presenting other options. Even if the women ask about other options, it’s, ‘Oh, you don’t want to be bothered with the pill. Let’s give you something that requires no thought.’” That pressure is heightened around the experience of birth because Alabama has the highest rates of maternal mortality in the U.S., and the numbers are particularly bad for Black women. . “A lot of Black women think, ‘I’ll go along with anything the doctors say,” Prewitt says, “ just to make sure I can get out of this hospital alive.”

Rauslyn Adams in Birmingham, Ala., on April 27.
Nydia Blas for TIME
Since the Dobbs ruling, according to early findings by researchers in North Carolina, many doctors have narrowed their focus to promoting the most effective contraception, like LARCs, while actively dissuading young people from choosing shorter-acting methods, especially in states with more restrictive reproduction laws. A soon-to-be-published study from researchers in South Carolina, which interviewed more than 1,200 women in five Southeastern states, found that nearly half of Black women overall experienced pressure from providers about birth control, compared to 37% of white women.
Some of this pressure is enshrined in law. In May 2023, for example, North Carolina passed a bill limiting access to abortion after the 12th week of pregnancy. It included a provision awarding $3.5 million in birth-control funding to health departments and community centers, with the stipulation that the funding could be used for only LARCs, not the pill, and only for poor or uninsured patients. “When this version came through in the wee hours of the night, I highlighted that section, and wrote in the margins, ‘REPRODUCTIVE COERCION’ because it was explicitly about LARCs instead of about funding any contraceptive options," says Erica Pettigrew, a primary-care physician in North Carolina. “I was really disappointed in this earmark, but I saw so many of my colleagues thinking this was a good thing.”
Adolescent-health experts worry this coercion will only get worse as policymakers and physicians try to prevent those in states with abortion restrictions from getting pregnant in the first place. “The slippery slope that we will go down is another type of reproductive restriction by coercing people to use these long-term methods who may not have chosen them,” says Aisha Mays, a doctor and founder of the Dream Youth Clinic, which provides free health services in the San Francisco Bay Area.
That pressure has compounding effects. Women who feel pressured into getting an IUD or implant are less likely to trust their doctors or stay on any birth control as a result, according to studies. Some women turn to DIY medical care if they don’t trust their providers. A viral TikTok trend shows women removing their own IUDs because, in some cases, they can’t get an appointment or, in others, because doctors won’t remove them.
It’s one more example of the disparate treatment poor women and women of color receive when it comes to medical care. Black women are twice as likely to be coerced into procedures like inductions and epidurals during perinatal and birth care, according to researchers. Some doulas in Alabama say that after bad experiences with labor and delivery, women are electing to have home births rather than risk being ignored or undermined by doctors. Once they feel that doctors aren’t taking their concerns seriously, women are less likely to seek out and receive important screenings and preventative health measures, which leads to worse health outcomes overall.
Miannica Frison is a prime example of this erosion of trust. She doesn’t currently have an ob-gyn, and after her years-long battle to get her IUD removed, Frison vowed to never get birth control again. One of the biggest ironies for Frison is that doctors seem so obsessed with getting her on birth control, but seem to care so little about her actual pregnancy outcome. Frison did not want a C-section, but doctors gave her little choice, she says. Because UAB is a teaching hospital, there were constantly people coming into the room to poke and prod her, she says, sometimes not even introducing themselves when they stuck fingers into her body.
UAB says that decisions about a vaginal or C-section birth are made in the best interest of patients’ health and safety, and that every woman provides written informed consent for “a full range of services” when admitted, including a C-section. “UAB is one of the largest and most advanced academic medical centers in the nation, so patients benefit from the expertise of highly trained care teams who provide a patient with evidence-based care,” a spokeswoman said in an email, adding that medical students are not involved in hands-on care in delivering a baby.
Frison was discharged from the hospital on Mother’s Day. Soon after she got home, she began vomiting. She’d been discharged, she says, even though she’d told doctors she felt extremely sick; when she was readmitted to the hospital, she says, she found out that she had sepsis. Frison couldn’t nurse her son because she had to spend five days in the hospital without him; when she got out, he wouldn’t latch.
“They were happy to tell you about how you could get sterilized,” Frison says. “But when it came to aftercare, or pregnancy care, none of that mattered.”

(From left) Miannica Frison, Rauslyn Adams and Crystina Hughes in Birmingham, Ala., on April 27.
Nydia Blas for TIME
—With reporting by Leslie Dickstein


