Pregnant Oregonians need more addiction and mental health support — but the state’s network is fragile
The story was originally published by InvestigateWest with support from our 2025 Impact Fund for Reporting on Health Equity and Health Systems, as well as the Center's engagement initiative.

Sarah Bovee does crafts with her 4-year-old son, Ryan, at their home in Oregon City, Oregon. Bovee, drawing on her own experiences with opioid addiction and recovery, is a peer support specialist and doula for mothers with substance use disorders. Bovee says support from a doula and addiction specialist “changed the tape in my head” and helped her overcome some of the shame and stigma of battling substance use disorder through her pregnancy.
(Leah Nash/InvestigateWest)
Every year, a group of Oregon health care professionals gathers for a grim exercise — reviewing every case in which a mother died during or soon after pregnancy. This past February, they reported a troubling finding: Mental health conditions and substance use were causing more of those deaths than any other factor.
Most of the deaths were suicides or overdoses. Some of the women were homeless. Many faced discrimination or fell through cracks in the health care system due to the complexity of their needs.
“These are tragic cases,” said Dr. Mark Tomlinson, a maternal-fetal specialist who chairs the Maternal Mortality and Morbidity Review Committee, created by the state Legislature in 2018. “Sometimes seeing opportunities that could have been done differently, that could have prevented this … it’s hard to look at these things.”
The committee’s work is part of a nationwide effort to better understand the country’s troubling growth in pregnancy-related deaths marked by deep racial disparities. The maternal mortality rate for Black and Indigenous people is three times higher than that of white women, and they are more than twice as likely to die during or after pregnancy from substance use or mental health-related causes, which have become leading drivers of maternal deaths across the nation.
According to Oregon’s review committee, almost all of the 13 mental health and substance use-related maternal deaths from 2018 through 2021, which amounted to 41% of all the mothers who died, were potentially preventable. The deaths highlight the challenge of reducing maternal mortality and racial disparities even in a state like Oregon, which is home to pioneering programs that combine behavioral and perinatal health care.
Oregon’s network of care for parents most at risk remains fragile and piecemeal. Programs like Project Nurture, which serves pregnant people with substance use disorders, has seen success in Portland and a few other communities but leave large swaths of the coast and Eastern Oregon unreached. There aren’t enough health care workers, and those who remain report high levels of burnout. Despite the strains on these systems, state lawmakers recently passed up an opportunity to increase funding for programs focused on pregnant people battling addiction, and advocates worry that impending federal cuts to health care programs like Medicaid may make it even harder to sustain progress.
But public health officials say that providers and politicians are still not broadly aware of the toll that substance use disorders take on pregnant people, especially how deadly those conditions have become.
“The problem has grown exponentially in the last 10 years. And the people that are making decisions don’t see that,” said Dr. Heather Mackay-Gimino, an OB/GYN on the review committee. “That’s to me, a huge barrier.”
State Sen. Lisa Reynolds, D-Portland, said she was “frustrated and disappointed” that a bill she introduced in the 2025 Legislative session to help peer recovery programs bill Medicaid for their services failed to advance, despite research showing their effectiveness.
“Every pregnant person should have easy, quick access to substance use disorder treatment if they have an issue,” Reynolds said. “And we are not there. We’re better than some states, but not as good as we should be.”

Early childhood advocates rally for a “Choose Children Day of Action” hosted by the Children’s Institute, a Portland-based nonprofit. State Sen. Lisa Reynolds (right) sponsored a package of six family-focused bills during the 2025 legislative session.
(Celeste Yager-Kandle/Children’s Institute)
Unless lawmakers and health officials prioritize care for pregnant people with substance use and mental health needs, practitioners and advocates predict Oregon will struggle to save more lives and reduce the disproportionate harm to people of color and lower-income women.
“We are making a statement by what we do not fund, and I think we are placing values on certain moms versus others,” said Kali Thorne Ladd, chief executive officer of the Children’s Institute, a Portland-based nonprofit advocating for early childhood programs. “And in doing so, we perpetuate inequities.”
‘I didn’t feel human’
Hours after giving birth to her son in July 2021, Sarah Bovee realized something was wrong.
She was recovering in a Seattle hospital, drowsy from labor and a dose of buprenorphine, a medication to treat opioid use disorders. But there was mounting pressure in her pelvic area, so she alerted a nurse.
The nurse told Bovee that she was experiencing withdrawal and probably just needed to go to the bathroom.
“I know this isn’t withdrawal,” she recalled telling the nurse. “I know what I’m feeling.”
But the nurse didn’t examine Bovee, so she tried to do as she was told. Instead, she fell asleep on the toilet, where she sat alone for 45 minutes.
It wasn’t until she woke up and stepped into the shower that Bovee discovered the real problem: She had a severe prolapse, a shifting of organs caused by weakened pelvic muscles and ligaments that is common after birth, but gets worse with straining and requires immediate treatment. She was rushed into surgery, needed multiple blood transfusions, developed an infection and was put on antibiotics for three weeks. Bovee believes things wouldn’t have gotten so bad if she had been examined when she first raised a concern.
Instead, Bovee felt shamed and dismissed throughout the birth, and suspected her admission of ongoing substance use was the primary reason. When she first told a nurse about it, Bovee said, she was immediately asked whether she had any open wounds on her body. While she was in the shower, where she discovered the prolapse, the nurse warned her not to defecate there.
“I didn’t feel human,” Bovee said. “It was hard to heal from that whole process.”


On the left are family photos that Sarah Bovee, an Oregon City, Oregon, mother in recovery, set out to decorate her home. Bovee, pictured on the right with her 4-year-old son Ryan at their home in Oregon City, Oregon, says support from knowledgeable, understanding health care providers helped her rebuild relationships with her other three children and successfully recover from a relapse during her pregnancy with Ryan.
(Leah Nash/InvestigateWest)
Four years later, Bovee remains in recovery and is raising her 4-year-old son Ryan. Her journey underlines the complexity involved with making pregnancy healthier for people at highest risk of serious or deadly complications — and how targeted programs can make a difference.
As a child, Bovee was removed from her mother’s care due to drug use, and years later, her mother died of a heroin overdose. Bovee lost custody of two of her older children through the child welfare system, too.
“Everybody in my family… has an alcohol or drug addiction,” Bovee said. Relapsing “just felt like a predestined failure.”
Although Bovee faced major challenges during her pregnancy with Ryan — she was navigating homelessness and grief after the deaths of several loved ones — she also had some support from people where it mattered most. After birth, she spent 21 days recovering in the hospital and a week in a drug treatment program, which Child Protective Services required in order for her to maintain custody of her baby. A doula trained in harm reduction brought her milk to the child’s father every three hours when Bovee couldn’t be with him. An addiction specialist guided her through treatment and advocated for her in court hearings.
“She changed the tape in my head, by just affirming that I was resilient, that I was a good mother, that I’m here and I’m continuing to stay here, and that’s evidence of my intentions to be a good mother for my child,” Bovee said of the specialist.
Now, Bovee provides that same kind of support as a doula and peer support worker with Project Nurture, the program operating in several Portland hospitals that brings together family medicine doctors, midwives, peer support workers, doulas, and drug and alcohol counselors to improve pregnant participants’ health and reduce child welfare placements.
For many parents struggling with substance use, the support can mean the difference between healthy outcomes and tragic ones, or between being able to parent their baby and experiencing the trauma of separation.
Drug use, alcohol and smoking put women at higher risk for pregnancy complications such as hemorrhage and preeclampsia, and increases the likelihood that babies will be born premature, underweight or with other complications. Perinatal depression, anxiety and psychosis can interfere with breastfeeding and spur increased social isolation and dependence on substances.
But in many instances the discrimination and stigma that parents face — which the review committee said was a “leading factor” in substance use and mental health-related deaths — can drive them away from seeking help. It’s also not uncommon for mothers dealing with addiction to avoid prenatal appointments out of fear that child welfare authorities will get involved.
“There’s people who I’ve known in the past that have had their baby on a bike path because they were afraid to go to the hospital,” Bovee said.
Parents of color may also face racism or a lack of cultural competency while seeking health care, said Victoria Warren-Mears, director of the Northwest Tribal Epidemiology Center, which collects data on tribal health. For some, painful histories with the health care system and the government have created deep distrust, including the involuntary sterilization of both Native and Black women and more than 100 years of forced removal of Native children from their families to institutionalized boarding schools.
“If you don’t feel comfortable in a health care system, you’re not going to go,” Warren-Mears said. “And people have all sorts of experiences with health care that may lead them not to want to seek services because of fear of how they’ll be treated.”
Strained solutions
The Maternal Mortality and Morbidity Review Committee has emphasized the need for programs that not only address the medical needs of pregnant people, but also issues like housing, food insecurity and stigma that can exacerbate physical and mental health problems. In its 2023 report to the Legislature, it recommended that the state “greatly expand” programs like Project Nurture, citing a 2021 expansion of the model into five additional counties.
Yet many areas of Oregon still don’t have such programs or struggle to meet demand.
“The needs are greater and the expenses are higher than either a standard pregnancy or maybe even than a standard person with substance use disorder,” said Reynolds, the state senator from Portland. “That combination makes it particularly tricky and expensive.”

State. Sen. Lisa Reynolds, D-Portland, introduced a “Momnibus” package of legislation focused on young children and families in the 2025 legislative session, including a bill focused on expanding access to doula and lactation care.
(Courtesy photo)
Drug treatment programs are often underequipped to meet the needs of pregnant people and may even turn them away. A 2019 study found that, nationwide, only 1 in 10 women of reproductive age who needed addiction treatment accessed it. A 2022 state assessment found the majority of county-level substance use disorder providers in Oregon don’t offer special programs for pregnant people or parents of young children. Meanwhile, perinatal health care practitioners are not always trained to care for people with addiction and associated mental health issues.
Research on the effectiveness of peer support, a key component of these programs, is still emerging, but participants say it can make all the difference to connect with someone who has experienced the same struggles and come through them.
As a peer and doula, Bovee attends prenatal appointments and walks women through referrals for housing, therapy and food stamps — not just handing them a phone number, but making introductions and following up. She has brought someone their medication to spare them a trip to a pharmacy near where street drugs are being sold. She waited in her car for four hours while talking a very pregnant client through her fears about giving birth in a hospital. She advocates for the needs and preferences of the mother during the birth, and remains a resource for at least a year postpartum.
Throughout the process, she works alongside midwives and drug and alcohol counselors at Legacy Emmanuel Medical Center in Portland. All team members are trained to provide non-stigmatizing care.
Project Nurture has shown promising results: A 2018 analysis linked participation in the program to lower incidences of preterm birth and C-section, and increased engagement with both substance use treatment and perinatal appointments. A 2020 study of the program echoed some of those findings, and also found a reduction in child welfare placements and substantiated maltreatment findings among participants within a year of birth.
“It’s really hard to think of any other program that could potentially have this much of a long-term impact, because it’s such a critical time period for the mom, for the baby, for the pregnancy,” said Cat Livingston, medical director for Health Share Oregon, a nonprofit that funded the launch of Project Nurture a decade ago. “And it could change the trajectory of kids’ lives, where they can stay within a home with parents who are getting adequate substance use disorder care and parenting support.”
One of the main obstacles to growing such programs is their struggle to get paid through Medicaid, the federal-state health insurance program for low-income adults and children. While the model brings behavioral and physical health together into one setting, in the billing world, those services remain siloed. Regulations have kept some hospitals from being able to bill Medicaid for peer services. Organizations eat the cost of the care that they can’t recoup, which provides little incentive for the model to grow.
“In order for this to have long-term sustainability, I believe that we need to have a payment mechanism that recognizes that this is more complicated care,” Livingston said.
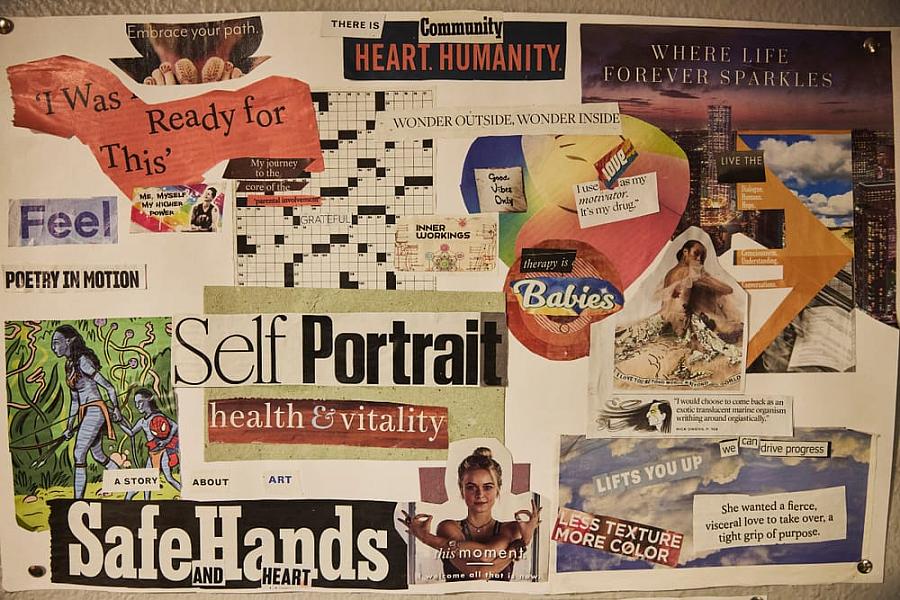

A vision board (left) and other recent artwork by Sarah Bovee, an Oregon City, Oregon mom in recovery.
(Leah Nash/InvestigateWest)
As of September, around 200 participants were enrolled in Project Nurture. Nurture Oregon, the rural expansion, served 341 people within its first two years. It’s not clear how many pregnant or postpartum people may need that support, but according to the most recent data from the National Survey on Drug Use and Health, nearly 22% of Oregonians ages 18 or older reported experiencing a substance use disorder within the last year — more than 900,000 people.
Black and Indigenous residents are hit hardest. Both groups are less likely to access substance use treatment and experience the highest rates of deadly overdose, according to data from the Oregon Health Authority. They are also less likely to access adequate prenatal care.
Due to a lack of comprehensive data, it’s difficult to assess how the state’s existing wraparound programs are meeting the needs of Black and Indigenous parents. Snapshots of data from Project Nurture and Nurture Oregon sites show that the rate of Black and Indigenous participation generally tracks with the demographics of their communities, but leaders expressed a desire to increase the cultural responsiveness and diversity of peers and providers.
In many instances, organizations focused on Black and Indigenous families are stepping up to fill the needs within their own communities, but rely almost entirely on grants and donations, limiting their reach.
Sacred Roots, a Portland-based program run by the Black Parent Initiative, provides free doula and lactation support to Black women. Like Project Nurture, its doulas and lactation specialists are trained to spot those struggling with their mental health or substance use and to provide support or connect them to other resources, said Michelle Smith, program manager.
Sacred Roots is supported primarily by grants. While it has explored the possibility of becoming a Medicaid billing hub for the doulas it contracts with, the complexity of the process stalled those efforts, Smith said. The organization is “familiar” with Project Nurture, she said, but there isn’t a robust referral relationship.
Meanwhile, peer support workers like Bovee are concerned about the sustainability of their work. Some programs have recommended that peers focused on pregnant patients take on smaller caseloads due to the complexity and emotional toll. But in reality, many workers overload themselves in order to avoid turning people away. In September, Bovee had 28 clients, about double the recommended amount.
The lopsided ratio of demand for help versus the number of people who can provide that help “kind of preys on people with lived experiences … because I’m gonna show up for somebody in need, period,” Bovee said.
Her work demands are often unpredictable, and while her employer affords her some flexibility, Bovee said she’s not allowed to work overtime. Even working full time, she still relies on a housing voucher to help pay her rent.
“We’re persons in recovery, too, right? I need it to be sustainable,” Bovee said.
Faltering progress
While research continues to show the deadly risks that mental health and substance use pose for pregnant people, several Oregon public health leaders said a lack of awareness among lawmakers and the public is hampering efforts to improve support.
As required by law, the review committee’s reports are submitted to Legislative health care committees. But Tomlinson, the committee chair, said he’s unsure how many state leaders have read them. Besides Reynolds, he hasn’t heard from many lawmakers, he said.
“We have no idea who looks at it and what they think about it, not even within the Legislature,” he said. “We didn’t hear anything from the governor.”
Gov. Tina Kotek “has long been a proponent of doulas as key supports for pregnant women,” said spokesperson Lucas Bezerra. “The work of the committee informs her approach, and she will continue reviewing their reports and supporting their work.”
Reynolds, a pediatrician, worked with groups such as Black Futures Initiative and the Children’s Institute to craft and introduce a slate of bills focused on young families this session. Of the six bills that Reynolds introduced, two passed: One strengthened eviction protections for families with young children, and another bolstered pay and access to doula care, which provides mental support for families.
But Oregon Senate Bill 691, her bill requiring Medicaid to cover peer services in all clinical settings, died without being heard in the legislative budget committee. It had no public opposition, but Reynolds said the bill fell down the list of priorities as the session went on.
It was a blow to advocates who worked to craft the bill and whip up support.
“This is a supermajority Democratic state,” said Thorne Ladd, executive director of the Children’s Institute. The peer services bill’s failure “shows we haven’t done our work here.”
The Oregon Health Authority is convening a new workgroup to strategize ways to clear some billing barriers and encourage access to health services without legislative action, a spokesperson said. Reynolds also said, given the state’s budget challenges, that she’s looking for other ways the state can prioritize pregnant parents without asking for new dollars.
But that work is unfolding against a backdrop of cuts to public safety-net programs. Oregon is poised to lose billions of Medicaid dollars in the coming years as a result of the spending package Congress passed this summer, called the “One Big Beautiful Bill,” and state officials estimate that new Medicaid enrollment requirements will lead to around 200,000 Oregonians losing health care coverage.
For hospitals already struggling financially, costly maternal health care units are also one of the first services to be cut back.

Sarah Bovee poses for a portrait with her 4-year-old son, Ryan, at their home in Oregon City, Oregon.
(Leah Nash/InvestigateWest)
But the payoff of such programs can last for generations. Supportive, stigma-free care has helped Bovee rebuild relationships with all of her children. She sets Fridays aside to be with her youngest son, Ryan, and they often spend those days doing art projects or walking along the Willamette River. The joys help fuel her work, she said, while her work helps remind her of how far she has come.
“Every single client I come across, I see myself in at some point in my journey,” she said. “And it reminds me I’m not only offering support to people like me, I’m healing parts of myself with every step that I take. Every time I show up, every person I connect with, every time I allow myself to be vulnerable and create a safe space for persons like me. It’s the flap of butterfly wings that changes things a generation away.”

