On a warm August afternoon in 2002, Bonnie Steele stood in the dining room of her family’s five-bedroom house, printing an essay for her evening theology class. She examined the homework beside an open window, where her north Minneapolis neighborhood’s summer air and sounds lingered.
Two of her daughters peeked into the room.
“We’re going to walk over and go see Grams,” the 12- and 19-year-olds told Steele.
Her four kids often walked to her parents’ nearby home. Usually, it was quiet and only took a few minutes — but this day was different.
Seconds after the front door closed behind the girls, the sound of a car’s engine filled the dining room, followed by screeching tires. Steele peered out of the window and saw a man leaning out of the car with a rifle pointed toward her girls.
“He started shooting, and it was like BOOM, BOOM, BOOM!” Steele said. “It just reverberated off of all the walls in that room.”
She was paralyzed by fear, unable to chase after her children or call out to them as she desperately wanted. Both girls survived the shooting unscathed, but Steele said the trauma remains.
She knew that she and her family had to move. Years of living in poverty and in fear for her life had taken a toll on her health.
Weeks earlier, during a dental visit, she discovered her blood pressure was 270/150, well above the healthy adult average of 120/80. With stage 3 hypertension, Steele, who was 45 at the time, was at risk of a stroke.
Steele was likely experiencing the effects of “weathering.”
The term describes how repeated exposure to stressors leads to poor health outcomes. A related concept, racial weathering, points to racism as a major stressor among Black Americans, contributing to their historically high rates of chronic disease, viral infection and premature death.
The science of weathering
A weathered body is weaker, ages faster, and is more prone to chronic disease, said Arline T. Geronimus, a public health researcher and professor at the University of Michigan who first proposed the hypothesis in 1992.

Arline Geronimus
When a person experiences consecutive life-threatening situations like an eviction notice or physical violence, they become weathered. These situations trigger a fight, flight or freeze response and causes the body to work harder to help a person escape the threat or to fight back. Stress hormones are released and excess oxygen flows to major muscles like the heart. Blood thickens to prevent death from injury.
The fight, flight or freeze response is only helpful against an occasional threat. When flipped on and off again, it becomes a problem. The fluctuation of chemicals wears the body down into a “weathered” state.
Geronimus said Black Americans are at greater risk for weathering than their white counterparts due to societal pressures.
“Populations that have been racialized or stigmatized or are subject to structural and systemic, as well as interpersonal racism, are the ones that are likely to weather the fastest and the worst,” she said.
Add to that, Black Americans are more likely to experience poverty, violence, discrimination, and other life-threatening situations in their lifetime. Those health disparities can lead to conditions that Geronimus said can be caused by weathering:
- Diabetes: In 2019, Black Americans were 2.5 times more likely to be hospitalized with diabetes than white Americans. (Stress can cause blood sugar levels to rise. While this is a healthy short-term response, in the long run, it causes insulin resistance.)
- Heart disease: Black adults are more than twice as likely to die of cardiovascular disease than white adults. (Long-term stress can cause abnormally high levels of inflammation in the body. This can increase plaque buildup in the arteries and lead to coronary artery disease.)
- Hypertension (high blood pressure): Two in five Black men (42%) and Black women (43%) suffer from hypertension, compared to 31% of white men and 27% of white women. (Stress triggers a release of cortisol into the blood, known as “the stress hormone,” which in turn raises blood pressure.)
A History of Racism and Stress in America
Racism has been a stressor for Black people since America’s inception. From approximately 1619 to 1865, enslaved Africans endured various forms of abuse. The Emancipation Proclamation of 1863 freed nearly four million enslaved African Americans, but systemic and interpersonal racism persists.
Bonnie Steele, who is now 67, noticed the first signs of weathering in herself after the terrifying shooting outside her Minneapolis home. But even before that, she saw it in her father, as he endured the stress of racial violence.
Her father worked as a janitor in Minneapolis’ public schools and a hospital between the 1950s and 1980s. Despite being an intelligent man who could solve algebraic equations in his head and recite the Declaration of Independence, Steele said he was denied access to the privileges of his white counterparts. He couldn't access education, was denied homeowners insurance, and was passed over for jobs because he was a Black man who'd have to work near white women, she said.

The home where Bonnie Steele grew up in Minneapolis.
Submitted
He worked handyman jobs overnight in a “sundown” part of town, where Black people were attacked by white residents if found there after dark. On those nights, Steele’s mother would load young Bonnie into the car and drive to her father’s worksite, where the mother and daughter would sleep until morning.
“They, probably she more than him, hoped being together might afford some protection from being in Northeast alone at night,” Steele said.
I’m sick and tired of being sick and tired.
Fannie Lou Hamer, 1964, co-founder of the Mississippi Freedom Democratic Party and a victim of forced sterilization
That threat of racial violence was reminiscent of Steele’s father’s early life in Greenville, Miss. As a teenager, he fled the southern town when a neighbor, a Black husband and father, was lynched and castrated by a group of white men after refusing to give up his family’s land. The father’s badly beaten son was returned home with a warning: “Be gone by sundown or we’re going to kill the whole family.”
Steele’s father was one of approximately six million Black southerners who fled north between 1910 and 1970. Still, even as a “racial refugee” during the Great Migration, he couldn’t outrun racism. Of his life in Mississippi, he wouldn’t tell his daughter much. She says he would say: “I didn’t leave nothing there.”
Her father’s mysterious past was accompanied by constant, unexplained infirmities. Kicking, screaming nightmares and daily vomiting led his daughter to believe he may have been a victim of weathering.
“I absolutely believe his nightmares and vomiting were stress-related,” Steele said.
How weathering causes multiple chronic conditions
Research has linked weathering to individual illnesses prevalent in the Black community, including high blood pressure and heart disease. Less discussed is how racial weathering leads to multiple chronic conditions, which Black people develop five to-10 years earlier than other groups.
“It's very rare for weathered people to have just one condition,” said the Michigan researcher Arline Geronimus.
“Parts of your body are overused, some are under-oxygenated. So, for both reasons, a lot of your systems and organs have been damaged and dysregulated or weakened.”
During the COVID-19 pandemic, people with multiple chronic conditions, also referred to as “underlying conditions” or “comorbidities,” were most at risk for severe or fatal infections. Studies report that 75% of hospitalized COVID-19 patients had at least one preexisting condition.
At minimum, 73,460 Black people died with COVID-19 between 2020 and March 2021, according to The COVID Racial Data Tracker. Overall, Black Americans were hospitalized two times more and died 1.6 times more than their white counterparts.
“The disproportionate death toll of the COVID-19 pandemic on the poor and people of color lays bare the fact that weathered bodies are more vulnerable to the worst ravages of infectious disease outbreaks,” Geronimus said.
In a 2021 paper titled, “Weathering the Pandemic: Dying Old at a Young Age from Pre-Existing Racist Conditions,” Geronimus argued that several factors contributed to the poor outcomes among Black and other people of color. These factors include: overexposure to COVID-19 for “essential workers;” close quarters and limited medical care for inmates in jails and prison; and an inequitable access to medical care.
Some infected by COVID-19 died at younger ages than white Americans because their immune systems were previously weakened by stress, Geronimus writes in the paper, published in the Washington and Lee Journal of Civil Rights and Social Justice.
Contrary to a commonly held belief, healthy eating and regular exercise aren’t strong enough interventions to curb these outcomes in the Black community, Geronimus said.
“Those things don’t completely mitigate weathering because…[racial] stressors are triggered anywhere you are,” she said.
Gun violence and high blood pressure
After 10 years in a house where gun violence constantly interrupted family time, Bonnie Steele now believes the stress of it all severely damaged her health. An automatic weapon once fired off near her daughter’s backyard birthday party. On another occasion, bullets pedaled through the living room walls while her father visited.
“Stressful doesn’t even begin to describe it,” she says.

The Minneapolis home where Bonnie Steele lived with her family before gun violence forced them to flee to a safer neighborhood.
Bonnie Steele
When her daughters were nearly shot during that summer walk in 2002, it was the final straw.
Steele called her husband, Jerry, immediately.
“I said, ‘This is it. I am done.’ I literally told him, ‘I don’t care what happens to this house. If they kill one of the kids, then what do I have?’” she said. “And he just said, ‘OK, we’re gonna go.’”
Steele and her husband sold their dream home in Minneapolis and moved 25 miles West to Minnetrista, a small town with a 7% poverty rate and 0.2% Black population.
Minnetrista was eerily quiet.
They heard crickets at night instead of gunshots. And during the day, saw horses and trees instead of cars and concrete. Their new three-bedroom house sat on its own land, a mile from the next home. The children could roam freely outdoors for the first time in years, catching frogs and playing in the pastures.
Steele’s health improved immediately.
“We’d been there a week, and I went into the doctor, and my blood pressure dropped down to normal,” she said about the 110/70 reading.
For so long, Steele and her doctor assumed her numbers were high because she had some risk factors that are commonly associated with hypertension, such as being overweight. Her race has long been used as a risk factor, but that can overlook other underlying causes that are associated with racial weathering. Only when they considered the impact of her previous environment did they understand the connection. “We were stunned,” she said.
But Minnetrista was only a temporary refuge. With too little income and two children in college, the family of six couldn’t afford to live there on their own. After a year, they left the home they were renting from a friend and headed back toward Minneapolis. They settled in a neighboring city, Minnetonka, for its affordability and proximity to the children's schools.
Declaring racism a public health crisis
Today, 21 years after leaving Minneapolis, Steele lives with seven chronic conditions: anxiety, arthritis, depression, fibromyalgia, high blood pressure, metabolic syndrome, and Type 2 diabetes. The first time she contracted COVID-19 in 2022, it landed her in an intensive care unit.
“Pain is just part of my life,” she said. “I try my best to ignore it, but it is just an everyday thing.”
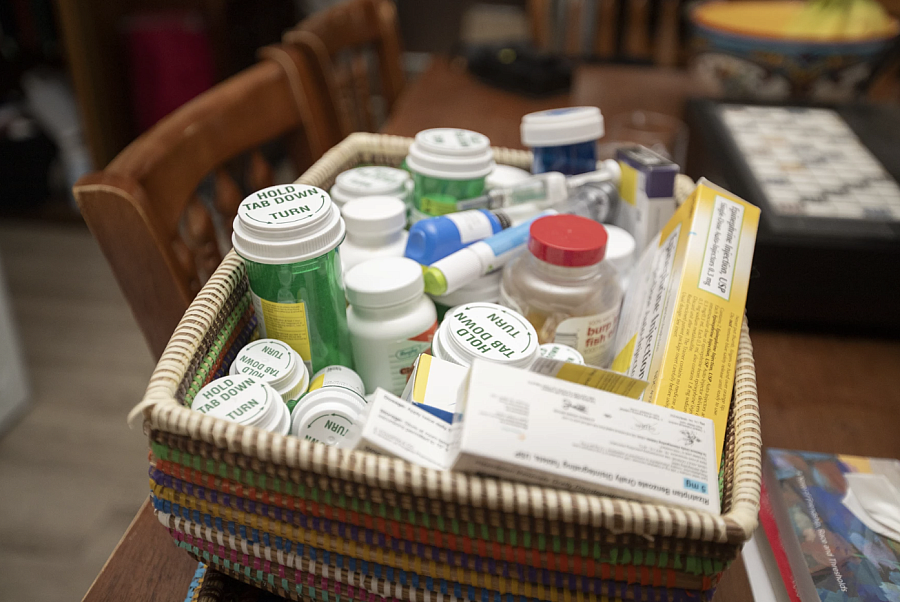
Years of living in poverty and in fear for her life has taken a toll on Bonnie Steele's health. She now uses several medications.
Christopher Mark Juhn
Her illnesses compounded over the years, as she and her husband attempted to protect and provide a future for their four children. They prioritized education, hoping it would give the kids access to a safer, more stable life. Despite what Steele describes as discriminatory treatment from local schools and teachers, all the children graduated college and landed six-figure jobs — but it came with a cost.
“To work as hard as we did, it required everything we had. Everything physically, emotionally, spiritually, intellectually that we could put into it,” Steele said.
But she was determined to provide a better life for her children, starting with a commitment to her firstborn moments after the little girl was born.
After a three-day labor, Bonnie says she whispered into her daughter’s ear: “I don’t know what the price will be, but I will pay it for you to not have the life that I’ve had.”
Moving the next generation of her family forward — against America’s backdrop of racism and wealth inequality — may have contributed to her poor health.
“I do wonder if some time if we have these health issues because we pushed so hard to get out of poverty,” she said.
Steele believes the government should address barriers affecting the quality of life of Black Americans, and ultimately, their health. She is an advocate for reparations, a public health solution neither her city, state, or country has adopted.
However, her hometown of Minneapolis has explored other options.
On July 17, 2020, the city council there adopted a resolution declaring racism a public health emergency. It came two months after George Floyd was murdered by Minneapolis police officer Derek Chauvin outside of a convenience store.
“The City of Minneapolis recognizes that Africans were forcibly brought to this country, enslaved, and after the emancipation of slavery, citizens of this country perpetuated anti-Black racism through violence, mass incarceration and anti-Black policies, including redlining,” the council wrote.

Tia Taylor Williams
Submitted
While there was no mention of racial weathering, Minneapolis council members at that time acknowledged racism as a contributor to high rates of hypertension, cancer, heart disease, and diabetes in the Black community. The resolution includes plans to activate public departments to respond to community stress and trauma.
To date, 149 cities, 94 counties and 22 states have declared racism a public
health crisis, according to a map by the American Public Health Association. Tia Taylor Williams, director of the association’s Center for Public Health Policy, says the commitments are the proper response.
“Once you acknowledge that racism affects health, you acknowledge that there’s been intentional and historical disinvestment from communities,” she said. “The logical way to address that or to redress that is to invest in those communities.”
Acknowledging racial weathering in medical care
Medical professionals are beginning to speak more openly about racism. The American Medical Association pledged to confront it and mitigate its health effects in 2020. Doctors have also found ways to address it in their practices.
Dr. Pamela Adelstein, the director of family medicine at Fenway Health in Boston, says acknowledging racism in health care is vital. As a provider for people of color for over two decades, she’s witnessed racial weathering impact her Black patients.
Some live in food deserts and violent neighborhoods, Adelstein, 53, said.

Dr. Pamela_Adelstein
“If you can’t sleep then your blood pressure goes up. You can’t sleep because there’s gun violence all night. How do you do that? No one can,” Adelstein said. “People are having a normal reaction to an abnormal situation.”
Despite abundant research on weathering, Adelstein said she has colleagues who don’t consider the condition valid. Last year, after publishing an op-ed about it, she said a white male commented that he “asked all of the people of color in my hospital if they experience racism and they said ‘no’.”
“Part of the weathering is a sense of isolation,” Adelstein said. “It’s almost like society gaslights everyone to think that it’s your personal responsibility that has caused this, rather than more systemic factors.”
Adelstein asks her patients about their encounters with racism and believes other doctors should too. She suggests incorporating a questionnaire into visits that poses questions such as “how do you think racism has played a part in your general health,” “your mood,” “your anxiety,” and “your ability to parent or work or be a partner.”
She believes racism should be considered a risk factor and until the healthcare system pivots to acknowledge this, it’ll always be a “blind spot."
“The constant microtraumas and macrotraumas are detrimental to people’s health and well-being and have short- and long-term effects. And if we are going to improve the health of people, it’s imperative that we look at that. Otherwise, we’re missing a huge opportunity.”
A dream deferred
Policy change may have a positive impact on future health outcomes for Black Americans, but it does not help many others who were not adequately protected. In the past 20 years, Black Americans have seen 1.63 million deaths attributed to what is called excess mortality, according to a study in the Journal of the American Medical Association. The study says those who died were robbed of more than 80 million years of potential life. The main cause of death was heart disease, and middle-aged adults were among the most affected.
One of the last times Steele spoke with her dad was before he passed away in 1997. He brought up his granddaughter, and how he wanted to see her graduate from medical school. She recalls him saying: “Oh, I wish I could live long enough to see Nicky get her white coat.’”
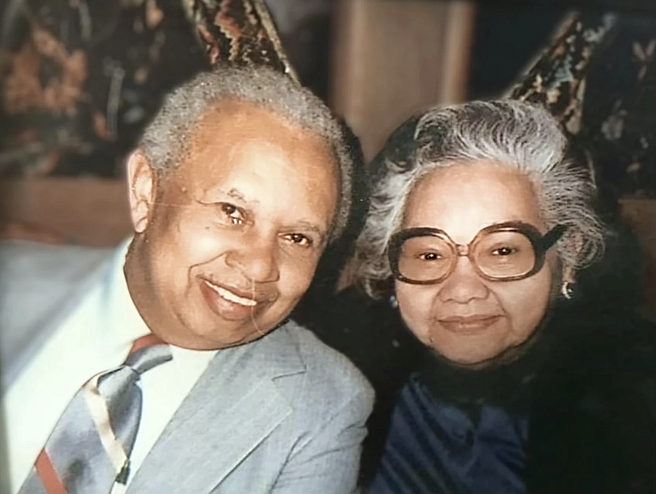
Bonnie Steele's father and mother.
Bonnie Steele
The grandfather’s wish remained unfulfilled. He passed at 75, due to a rare lung disease.
On a cold January day in 2024, Steele visited her father’s grave, and fondly recalled the moments her children spent with their grandfather: counting coins; seeing him at their recitals, and playing piano as he listened.
“Dad, I’m sorry you were born too soon, because it should have been you,” Steele said, referring to the opportunities her children were given. “But I’m so grateful you were here to make sure they lived the dream that you would have liked to have had.”


