Are penalties an effective way to improve hospital care?
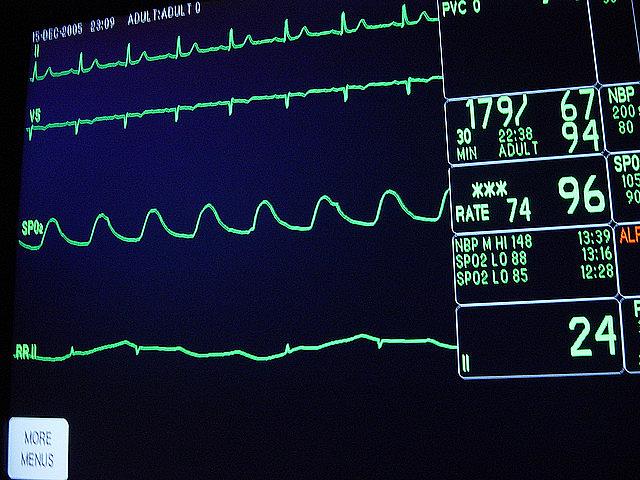
Photo courtesy of Flickr / brykmantra
High-quality hospitals are vital to healthy communities — they literally provide essential services. One of the many goals of the Affordable Care Act (ACA) is to improve hospital quality. The legislation set up penalty programs which reduce a hospital’s Medicare reimbursements if the hospital falls below certain quality measures. In theory, these penalties are meant to act as incentives, pushing hospital administrators and physicians to improve care. Whether the penalties will accomplish this goal is unclear.
This year, 2610 hospitals will see their Medicare reimbursements reduced, according to a Kaiser Health News analysis. In 28 states, the majority of hospitals will be penalized. However, evidence is already emerging that suggests the penalties, in some cases, may not be working as planned. For example, a report in the August edition of Health Affairs revealed that California’s safety-net hospitals were more likely to face fines even when they provided better care compared to other hospitals.
Safety-net hospitals, which care for a disproportionate number of low-income and uninsured people, are central to the communities they serve. Many of their patients have no other options for receiving medical treatment. Yet there is growing concern that these hospitals will face the largest penalties.
My stories will examine the impact of three different ACA penalty programs on hospitals: value-based purchasing, readmission reductions, and hospital-acquired conditions. The fines for each program were designed to be modest, but there is a risk that the overlapping effect could be significant when hospitals receive penalties in all three areas. This is even more of a concern for safety-net hospitals, which may already have tight budgets.
Incentive programs have tremendous potential to bring about positive change. But any incentive scheme that involves cuts to essential services deserves special attention. My project aims to explore the real-world effects of the ACA’s penalty programs through interviews with hospital administrators, physicians, and patients, as well as an analysis of the latest data from the Centers for Medicare and Medicaid Services. Why are safety-net hospitals more likely to receive penalties than other hospitals? Are the penalties exacerbating funding shortages at hospitals that are already stretched thin? And what is the real impact of the penalties on quality of care? These are the questions I hope to address.

