More San Diegans could enter mental health conservatorships. But the system is already struggling
This story was originally published in inewsource with support from the 2022 California Fellowship

California Highway Patrol Officer Jesse Matias looks for an individual he has previously interacted with that suffers from mental illness in an encampment near a freeway in San Diego, April 28, 2022. Like other law enforcement agencies, the Highway Patrol responds to mental health crisis calls and may transport individuals to hospitals for possible involuntary holds if an officer determines they meet criteria.
(Zoë Meyers/inewsource)
Mimi Murray believed she could fix it.
All her son needed, she thought, was to come back to San Diego and get some help from Mom. She expected he would have a short stay at their Rancho Peñasquitos home in North County before finding a new job and landing back on his feet.
Why this matters
Some lawmakers are turning to conservatorships as a possible solution for the state’s homeless crisis, yet California’s system for involuntary mental health treatment is inadequate and lacks resources.
That was six years ago.
After 18 stays at shelters and recovery homes, Michael — who is diagnosed with bipolar II, schizoaffective and substance use disorders — remains homeless. His mother said though his eight years as a U.S. naval officer give him access to services through Veterans Affairs, he does not believe he is sick and does not regularly receive treatment.
Mimi, in turn, chooses to focus on the short-term.
“It’s not when he gets into permanent housing and he manages his mental illness, and hopefully he would find companionship. I can’t think about that,” she said. “I think about, well, I hope he is able to stay where he is next week and I hope he doesn’t lose his phone tomorrow, or I hope he doesn’t get his EBT card stolen again.
“I’m short-term because long-term didn’t work. I thought I could fix it.”

Mimi and Mike Murray are shown at their home in San Diego, Aug. 22, 2022. They are caregivers for their son who suffers from mental illness. (Zoë Meyers/inewsource)
As the state grapples with its homeless crisis, elected officials across the state have pointed to one longstanding law as a possible solution: expanding conservatorships for Californians diagnosed with severe mental illness. The move could put more people under the care of counties for treatment, even if those placed under conservatorship object.
But inewsource spoke with nearly 40 people involved in the mental health system and found major problems: Some are frustrated by the lack of resources and what they say is a reluctance by decision-makers throughout the county to pursue conservatorships, leaving out the most vulnerable people who may not voluntarily seek treatment because they’re unaware of their illness.
Others also believe a lack of data and oversight raises major questions about whether growing the program will actually work.
This isn’t the type of probate conservatorship more commonly associated as of late with pop singer Britney Spears. Instead, they’re called LPS conservatorships, a nod to the state’s Lanterman-Petris-Short Act: County officials can oversee involuntary medical treatment, including mandated medication and placement in a locked facility, for a person diagnosed with at least one of the eligible serious mental illnesses, among them schizophrenia, bipolar disorder and others.
A clinician must also deem the person gravely disabled, meaning they’re unable to care for basic needs such as food, clothing or shelter as a result of the disorder.
Some of San Diego’s most prominent leaders support CARE Court, a Gov. Gavin Newsom-led program that will allow people with psychotic disorders to be referred to court for behavioral health plans. If they fail to follow court orders, they could be referred for conservatorship.
Mayor Todd Gloria made conservatorship reform a chief message in his State of the City speech earlier this year, calling for state action “so that people who cannot help themselves aren’t left vulnerable to the dangers of life on the streets.”
But others argue conservatorships deprive people of their basic rights. They worry about forcing more people into a system that can’t meet demand as is and hasn’t been fully studied — and they fear any expansion of them would instead be used to push unhoused residents out of sight.
Alex Barnard, an assistant professor of sociology at New York University, said his research on conservatorships shows both sides can be true.
“The conservatorship system can both be impossible to get into for some people who seem to really need it,” he said, “and also have people stuck in it who don’t need it.”
Barnard blames a shared root cause: Lack of accountability and oversight.
Conservatorships are less common in San Diego
Mimi and her husband never formally sought conservatorship for their son, nor have health care providers who have worked with Michael. She said one case worker previously believed he qualified for a conservatorship but wasn’t hopeful it would be approved.
“As we heard over and over again, you’re gravely disabled if you can’t care for yourself, if you’re a danger to yourself or to someone else,” Mimi said. “And he never quite fit that definition.”
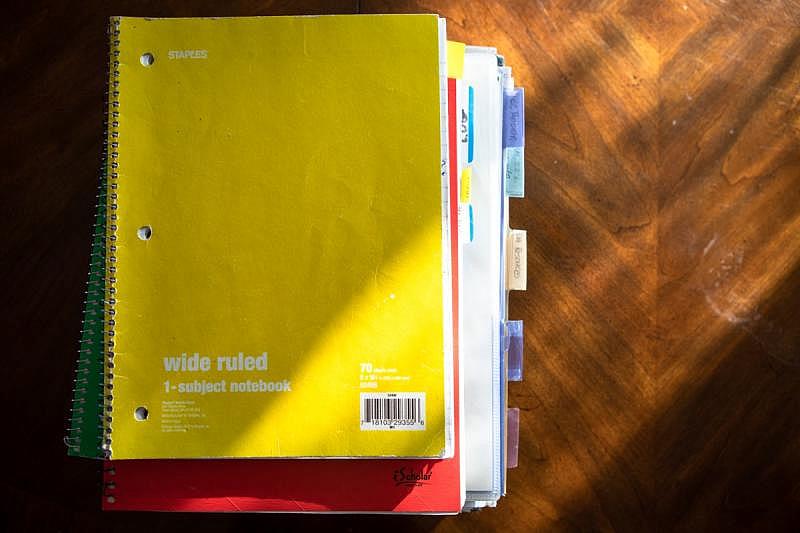
A stack of notebooks kept by Mimi Murray contains notes and information pertaining to her son’s care, San Diego, Aug. 22, 2022. (Zoë Meyers/inewsource)
Data shows San Diego has been pursuing temporary conservatorships less frequently in recent years, and one report found it held one of the lowest rates for permanent conservatorships among the state’s largest counties.
Temporary conservatorships last up to 30 days, and officials use that time to determine whether a longer-term arrangement is needed. During fiscal 2016-17, the county investigated nearly 500 requests for temporary conservatorships, according to data inewsource obtained. Officials petitioned the San Diego Superior Court, which has ultimate approval over conservatorships, for about 72% of those requests.
That percentage has dwindled nearly every year since, as has the number of referrals the county receives from medical providers. By 2020-21, the county only pursued temporary conservatorships for 53% of 565 referrals.
Counties’ powers are limited and those considered for a conservatorship go through a series of other officials, from law enforcement to clinicians to program providers, before their case lands in the public conservator’s office. Many people are placed on multiple 72-hour holds known as 5150s — a reference to a section of the state’s Welfare and Institutions Code — before their petition, if ever, makes it to the county.
San Diego-based psychotherapist Joseph De Vico blames officials for focusing on other priorities. “The only thing they care about is if the Chargers leave San Diego,” he said. “This is what makes people cry in local government.”
His arguably cynical views are at least informed by experience: De Vico has been involved in the system for nearly two decades and previously worked as an investigator in the county conservator’s office. Part of his job entailed fielding calls from people seeking help for their loved ones — pushing shifts to nearly midnight, he said.
De Vico now is a consultant, providing therapy and assisting families who are trying to navigate the conservatorship process. He said it’s a difficult pursuit that isn’t always determined by the severity of a person’s illness.
“I always tell people, all we can do is we have to keep throwing the truth out there,” he said. “And you just have to hope that you catch a conscientious person on a good day.”
Linda Mimms, a Poway resident who serves as vice chair of the Schizophrenia & Psychosis Action Alliance, described a discouraging process for families: If a loved one can present well for the short period of time they’re speaking with investigators, she said, securing a conservatorship is unlikely.
“The family, the siblings, they’re in a constant state of crisis,” Mimms said. “It is horrendous. And it’s not the type of health crisis that you’re going to have neighbors come over and bring a casserole — because nine times out of 10, you’re not gonna tell anybody. This is what parents say to me.”
County officials say though a smaller percentage of cases are being pursued, their efforts are becoming more efficient: The court granted more than 85% of permanent conservatorship cases in 2020-21, a percentage that has for the most part grown over the past five years.
Nathan Fletcher, chair of the Board of Supervisors, said the county’s goal is early intervention.
“There’s no reluctance on the part of the county to use (conservatorships),” he said. “But I will tell you, there is a long-term goal that a decline in these numbers would be seen as a good thing — if the originating reason for the decline is that we’re doing a better job meeting those goals.”
In San Diego, the court every year typically signs off on granting about 200 new permanent conservatorships, a one-year arrangement that can be resubmitted annually. Some 700 to nearly 1,000 permanent conservatorships are re-established each year, according to county data.
Still, those numbers are far lower than that of other counties when adjusting for population, according to a report from San Francisco County officials earlier this year. San Francisco reported 7.1 permanent LPS conservatorships for every 10,000 residents during fiscal 2020-21, the highest rate among the state’s 13 largest counties examined by the report. Los Angeles and Santa Clara were not included.
San Diego had the smallest caseload, with just 0.8 permanent conservatorships for every 10,000 residents.
The disparity between two urban areas with similar problems is hard to account for, said Barnard, “other than that it’s just a really under-regulated system with no clear vision of who should be conserved, how many people should be conserved.”
What the LPS Act was supposed to fix, and what problems persist
The LPS Act was signed in 1967 by then-Gov. Ronald Reagan in response to California’s practice of locking people with mental illness away in hospitals and facilities long-term, sometimes indefinitely.
The new law placed stricter limitations on involuntary hospitalization and instead favored voluntary treatment through community-based care.
But nearly 60 years later, problems remain statewide. A 2020 state audit found an inadequate system: Crowded hospitals and lack of treatment beds were causing up to one-year waits to receive care, data was incomplete and inconsistently available, and treatment after exiting a conservatorship was limited.
Auditors also found state officials did not know “the extent to which billions in funding has assisted” individuals with mental illness.
In San Diego, the number of beds is limited, and treatment is costly. The county has said that hospitalizing people for mental illness has cost local health providers more than $10 billion a year, and federal law creates severe limitations: Medicaid does not reimburse for care provided in psychiatric hospitals or other residential treatment facilities that have more than 16 beds.
Officials throughout the conservatorship process also are weighing other factors that have little to do with the legal criteria for conservatorship, Barnard said: Police are thinking about what will happen once they take people to the emergency room, for example, or hospitals are concerned about bed availability and the financial cost of treatment.

California Highway Patrol Officer Jesse Matias looks for individuals living under freeway ramps in Mission Valley, April 28, 2022. Like other law enforcement agencies, the Highway Patrol responds to mental health crisis calls and may transport individuals to hospitals for possible involuntary holds if an officer determines they meet criteria. (Zoë Meyers/inewsource)
And if a person is considered a particularly complex case, with medical needs beyond their mental illness or a history of violence, they could sit in an inpatient facility for months or years waiting for placement.
“It’s almost this random alignment that leads to somebody being conserved,” Barnard said. “A lot of those decision makers are thinking one or two steps down the line and realizing that this person isn’t going to wind up going where (they) think they should go, so is it really worth allocating scarce time and resources to this?”
The county has made significant mental health investments in recent years, including the rollout of Mobile Crisis Response Teams and new crisis stabilization units. Behavioral Health Director Luke Bergmann said the county uses “a pragmatic approach, a clinically grounded approach and openness to using tools that we have evidence work.”
In 2015-16, its behavioral health services budget was more than $440 million; this year, it’s nearly $890 million. Officials will also roll out plans later this month to move the county’s conservatorship program under the behavioral health department.
Barnard said while “we’re kind of living in a boom moment” for investment, San Diego’s mental health system has suffered from funding cuts dating back several decades.
“There’s a lot of things that are being proposed that would’ve worked for a lot of these individuals 30 years ago, had they been offered to them,” Barnard said. “But now it’s 30 years of them being burned and neglected.”
Fletcher said investing in behavioral health is his top priority — and the goal is “to get the right care to the right person at the right time.”
“The need for an LPS conservatorship should societally be seen as a damning indictment of our failure to not help people before it gets to that level of crisis,” he said.
A fix to San Diego’s homeless crisis?
Last month, as Mimi Murray was waiting in the VA hospital lobby for her son, she observed a man’s encounter with police. He was “disheveled” and talking to himself, she said, and appeared homeless.
Mimi watched it unfold for an hour before the man left, she said. She couldn’t shake the fact that a psychiatric care unit sat just a couple floors above.
“Nobody in that hour was called that was dressed like someone from the medical side of the hospital,” she said. “There were just four police officers that handled the whole thing. I thought, ‘If you can’t get care in the hospital and you’re exhibiting all these symptoms of mental illness, where are you gonna go?’”
The county’s number of homeless residents has jumped by 10% since January 2020, and the most recent data from the San Diego Regional Task Force on Homelessness found 13% of those surveyed reported having a serious mental illness that included a level of hospitalization or clinical care.
In the city of San Diego, where Mayor Gloria has defended his administration’s handling of the city’s homeless crisis, the number of unsheltered residents — meaning they weren’t in emergency or temporary housing — increased by 9%.
Gloria said he knows the public has heard him repeatedly speak about offering homeless services that were being declined.
“A lot of those folks are declining those services without the functional ability to actually make an informed decision,” he said. “A severe schizophrenic person with perhaps a co-occurring substance abuse problem is not likely able to make an informed decision. And yet our current system acts as if they can.”

California Highway Patrol Officer Jesse Matias approaches an encampment along the side of the freeway in San Ysidro, April 28, 2022. Like other law enforcement agencies, the Highway Patrol responds to mental health crisis calls and may transport individuals to hospitals for possible involuntary holds if an officer determines they meet criteria. (Zoë Meyers/inewsource)
Gloria said his own family has experienced mental health crises. His aunt has schizophrenia and occasionally goes missing; when his grandmother died a year and a half ago, “it was heartbreaking to see her in her last days just wondering about her daughter,” he said.
But Gloria also points to the burden on government operations: Nearly 60,000 calls were made to the city’s 911 system for mental health emergencies just last year — and officials estimate they consume roughly 400 hours of first responders’ time daily.
Yet the city is hampered by its lack of authority, the mayor said: It has neither a mental health hospital nor behavioral health clinicians, and only the county can submit an LPS conservatorship petition to the court.
Anne Jensen, program manager at San Diego Fire-Rescue’s EMS Community Health Team, said she encounters only a couple people per year who were in such severe condition that they may be eligible for conservatorship.
The program serves what the city calls “high 911 utilizers” — just 1% of San Diego’s population makes up about one-fifth of emergency calls.
“I think that they paint people that are vulnerable with a very wide brush stroke,” Jensen said. “And when you start to see the nuances you realize that one-size-fits-all is not gonna cut it.
“And ultimately we need very culturally humble people who can put patients in the center of everything.”

MJ Jacquot works in the triage department of the Telecare Mobile Crisis Response Team office in San Diego, Sept. 1, 2022. Mobile crisis response teams partner with local law enforcement and dispatch behavioral health experts to assess, de-escalate and connect people with services. (Zoë Meyers/inewsource)
Supporters stress that CARE Court, which Newsom signed into law last week, will be open to a limited number of the most severely ill residents who are living on the streets.
But proposing more conservatorships as a solution to homelessness has raised concerns, with critics casting doubts on whether forcing people into treatment is more effective.
Disability Rights California opposes CARE Court, saying it’s “based on stigma and stereotypes of people living with mental health disabilities and experiencing homelessness.” The advocacy group said Black Californians, who make up 40% of the state’s unhoused population, would be disproportionately impacted, and that officials should instead focus on community-based treatment centers and housing.
Josh Whitehead, a Chula Vista resident, was diagnosed as a teen with anxiety disorder that went untreated for several years. In 2018, at age 30, he was placed on a 5150 hold following a suicide attempt.
During what was ultimately a 10-day stay at Scripps Mercy Hospital in Hillcrest, Whitehead said he met other patients, including one who was on conservatorship and had been waiting six months to be placed at a long-term facility.
Whitehead said he fears the state “is just looking for an easy solution to a problem they’ve had no problem ignoring for decades.” Any proposal needs to address multiple issues, including homelessness and substance abuse — and come with substantial funding — to work, he said.
“I don’t see that happening,” Whitehead said. “I really don’t. I hate sounding fatalist in that regard, but they don’t really wanna solve the problem. They just want to kick it down the road again.”
What we don’t know
Officials told inewsource that talks of conservatorship reform happen without a full understanding of whether the system is working: The state has not fully studied the issue — the 2020 audit only examined three counties — and data is woefully lacking statewide.
Insufficient numbers submitted to the Department of Health Care Services mean the number of LPS conservatorships in California isn’t fully known. San Diego County was unable to provide any historical data on housing status and the race and ethnicity of conservatees.
“There have been a few years of a series of bills that are intending to or wanting to expand LPS,” said Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association of California.
“We thought, ‘Well, we don’t even really know what’s happening. So why are we trying to expand something that we don’t really, truly understand?’ ”
Barnard said the safety net the LPS Act was supposed to provide has withered because of a lack of attention and leadership from the state level. No state department oversees LPS conservatorships.
Questions about strategy — how many people are under conservatorship and whether that number should go up or down, for example, or whether those people should be in locked facilities or living in the community — have gone unanswered, he said.
“Here you have what seems like this incredibly important, coercive part of the mental health system,” Barnard said, “and yet there’s absolutely no visible strategy statewide of how we are using this tool.”
CARE Court stood out among the slew of mental health-related bills that came before the state legislature last session. The program would be rolled out in phases, with San Diego included in the first wave to set up their system by October 2023.
Legislators authorized $63 million to assist with implementing the plan. That’s in addition to the nearly $15 billion included in the state budget over the last two years for solutions to homelessness, including bridge housing.
Gloria concedes there are a lot of unknowns: how many more beds are needed, how many clinicians will be needed, what’s required from the budget, and what counties and cities will have to do — and as he admitted to inewsource, little personal optimism earlier this year that change would come. He’s more optimistic now after hearing from other elected officials and the momentum behind CARE Court.
But without a mandate from the state, none of those questions will be answered, he said.
“I’m here raising my hand saying I will find ways to build the housing, to create the units, to establish the shelter beds, to actually more functionally address this,” Gloria said. “But waiting to collect a bunch of data to address this literally consigns people to die on our sidewalks. And I’m just not willing to wait that long.”
The governor’s office estimates as many as 12,000 residents will be eligible for CARE Court.
‘I can’t cure it’
In 2020, Mimi penned a letter to friends. “Michael is not doing well… an understatement,” she said.
Michael had been recently released from jail — he’s been there multiple times for short durations — and was being transferred to a residential treatment center, but “slipped away before even getting admitted.” At the time, Michael was homeless, not taking medication “and instead existing in an environment which is pushing him down a rabbit hole of deep dysfunction,” Mimi wrote.
“The person with cancer or diabetes may want to do anything and everything to get cured… or at least get their disease under control,” she said in her letter. “But the same can’t necessarily be said for a person with mental illness.
“If we all can begin to recognize that, then maybe the stigma of mental illness will be replaced by understanding and caring and support.”

Objects like their son’s high school medal, photographed here at their San Diego home, are reminders to Mike and Mimi Murray of the achievements in their son’s past, Aug. 22, 2022. (Zoë Meyers/inewsource)
Mimi told inewsource that every time she and her husband thought it couldn’t get worse, it did. Their marriage, now entering its 53rd year, was strained, and she said they were determined to not let it fall victim.
Both continue to attend support group meetings, where they’ve learned to cope among others who are experiencing the same. Mimi occasionally accompanies their son on appointments and errands. And like other mothers who spoke with inewsource, she has a meticulously organized binder that holds his important documents and other information should he ever need them.
It took a long time to no longer feel guilty about her son’s illness, Mimi said. She’s learned there’s a difference between quitting and surrendering.
“I as a loved one cannot control it. I didn’t cause it. I can’t cure it,” Mimi said, recalling a conversation she had with a VA staffer who worked with homeless veterans. “And he said, ‘There’s one more thing. Your son didn’t choose it.’”
inewsource investigative data reporter Jake Harper contributed to this report.