Coronavirus is driving a big shift in health care toward telemedicine
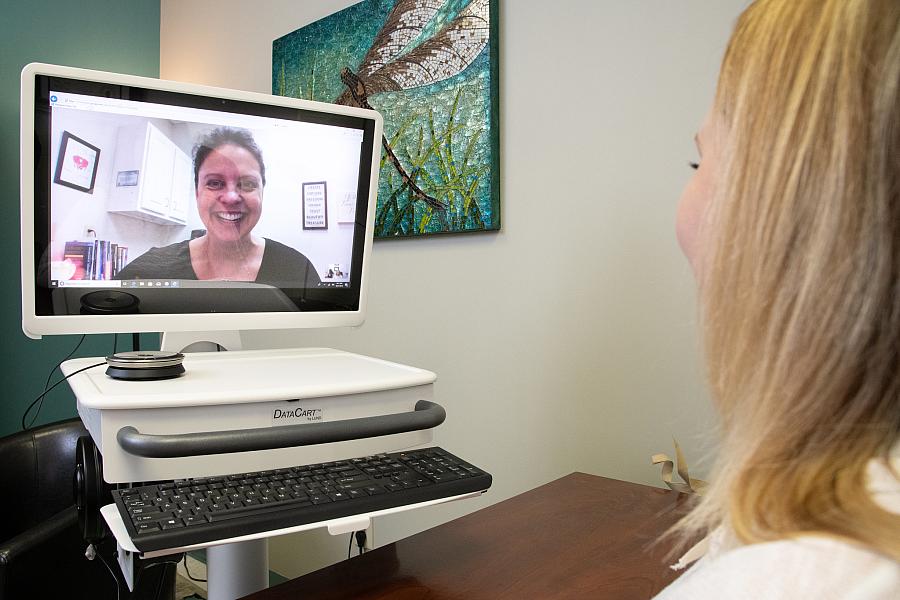
The coronavirus outbreak represents a potential sea change in how health systems use telemedicine.
In response to the COVID-19 pandemic — and in an effort to avoid unnecessary viral spread from patients visiting healthcare facilities — Congress approved new measures as part of the coronavirus bill signed on March 17, which increases access and provides reimbursements to providers for telehealth services. Prior to this amendment, hospitals were not funded by Medicare to provide routine telemedicine visits, and patients could not receive telecare in their own homes.
This act has the potential to transform health care permanently. COVID-19 has triggered dramatic changes in how many hospital systems approach telemedicine. At Keck Medicine of Medicine of USC, we have been shifting towards virtual care for the past two years and have made significant inroads in very different settings, from virtual primary care, to allowing families to see and chat with their loved ones and the recovery nurse immediately after surgery. As the COVID-19 outbreak has unfolded, this pace has accelerated at warp speed, and the new federal regulations will further boost our shift to telemedicine.
Clearly, what was needed to accelerate the telemedicine journey was an urgent imperative to do things differently. The pressure to reduce the risk of exposure to COVID-19 and still care for patients ordered by the government to stay home has shifted most of our non-urgent care to telemedicine visits. In the space of a few days, we have gone from around 100 televisits a day, to 650 in a recent two-day period — and climbing. In the face of the COVID-19 threat, suddenly the world has changed. Health systems including ours have found themselves needing to transform fast.
Five hundred million dollars have been allocated by Congress for telehealth spending to allow Medicare providers to be paid to provide telemedicine services to seniors. These updates allow not only payments for telemedicine visits but also include more radical steps — for instance, allowing doctors to prescribe controlled substances via a televisit without a prior in-person evaluation.
These are direly needed changes. We need to avoid unnecessary contact and protect both patients and staff from potential infection with the COVID-19 virus. The very patients whom we have worried would not adopt the new technology are the ones most at risk in this pandemic. The case fatality rates are highest for those 80 and over. In addition, friends or family who would often accompany an older patient on an in-person visit would breach social isolation.
Some forward-thinking groups, such as South Central Foundation in Alaska, have been ahead of the curve, and have already transformed the way they deliver care via patient portal communications and televisits. In addition, start-ups such as Babylon Health have demonstrated demand for health care delivered by phone or video, but many of their customers are young millennials who are skilled users of phone and video technology. Concerns that older patients could not cope, nor would want to see their physician virtually, have long been ingrained in our health care psyche, and there are real needs to consider around computer literacy, access and trust. But many of these concerns have been based more on myth than reality, and even the very elderly can often get help from grandchildren or friends and use FaceTime routinely.
So far, the early patient feedback is favorable, with patients valuing the time spared from making a visit when they are concerned about the risks of visiting a health care facility. But the potential use of this technology goes much further. In our community, USC Verdugo Hills hospital is using telehealth to screen patients in the ED waiting area, allowing patients who need higher levels of care to be directed immediately where they need to go while sparing other patients and staff from unnecessary exposure.
Other potential applications include allowing quarantined colleagues or those at high risk to virtually support their co-workers on the frontline in hospitals and in the ICU. Greater use of telemedicine has already been suggested as one way that U.S. hospitals can help avoid the high rate of fatalities and health care worker infections seen in Italy.
We need to fully embrace the potential for telemedicine as a major tool in the fight against the COVID-19 pandemic, but once the current crisis subsides, we should ensure that we continue the transformation our health care delivery systems. Telemedicine should become a routine way of delivering health care. Widespread adoption of telemedicine may prove to be one of the silver linings of this crisis.
Dr. Carol Peden is a professor of anesthesiology and director of the Center for Health Systems Innovation at Keck Medicine of Medicine of USC. Michael Hochman is the director of the Gehr Family Center for Implementation Science at USC Keck. Dr. Barbara J. Turner is a professor of medicine at USC Keck.