Decades of scary headlines aren’t curbing bad nursing homes. It’s time we help families instead
Once again newspapers across the country are trumpeting headlines announcing the latest horror shows brought to you by America’s nursing homes. Take, for example, The Quad City Times in Iowa reporting the “Rosewood Nursing Home Fined for Patient Neglect Abuse,” or The Oregonian telling readers that “Neglect at Ashland nursing home caused ‘extended suffering’ for weeks, suit claims.”
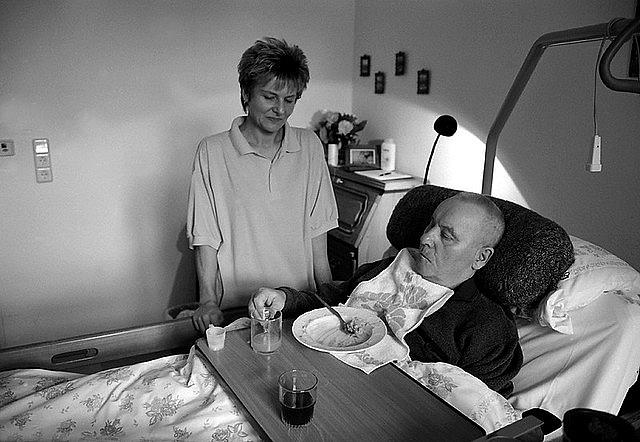
And so it has been since the early days of Medicaid in the late 1960s, which made it possible for families to receive government help paying for care while giving nursing home owners a government-sanctioned path to profitability. But with the potential for riches came abuse, neglect and the deaths of residents who have endured some awful care over the last five decades.
Despite a good federal law (though not always vigorously enforced), oodles of ratings shining light on bad facilities and helping families pick the good ones, the availability of graphic and disturbing inspection reports and a ton of press coverage, nothing much has really changed.
The structure and financial incentives of the industry conspire to give reporters the same story year after year. A newspaper or magazine headline written in 1975 or in 1995 would largely be accurate today. Undercover investigations I did for Consumer Reports in the 1990s and early 2000s spawned a lot of reporting by other news outlets. The takeaway was almost always the same: Families beware!
Since it has become obvious that journalism is not going to change the structural and financial incentives that allow bad nursing home care to thrive, it’s time to move the long-term care story into new territory.
We can still write about bad nursing homes and poor enforcement, like the GAO’s recent announcement that Medicaid regulators need to address enforcement gaps in Oregon’s nursing home enforcement dating back 15 years. But we need to do a better job reporting on the entire process that leads many people to bad nursing homes in the first place.
That means we need a new genre of reporting that actually helps families facing the difficult task of choosing care after a hospital stay, as my family did when I was moved from hospital to hospital in late 2017 and early 2018 for a serious and unexpected illness. I’d wager most families are no more prepared to confront those critical choices than mine was. However, decisions they make or, more often, decisions made for them, can mean the difference between the recovery or decline of their loved ones.
With so much at stake, informed decisions that place the right patients in the right care setting at the right time are essential. That requires helping patients and their families understand the full range of options available to them.
The structure and financial incentives of the industry conspire to give reporters the same story year after year. We need a new genre of reporting that actually helps families facing the difficult task of choosing care after a hospital stay.
That’s the conclusion reached in four excellent reports from the United Hospital Fund (UHF) in New York City that found one in five hospital patients across the country need further care after discharge. They are being sent to nursing homes, long-term acute care hospitals (LTACHs), sub-acute care facilities, home care agencies, and rehabilitation centers, often with little input from their families or knowledge of what these facilities do.
If they seek help from the media to inform them about how the process works, options and pitfalls, families come up the losers. In short, discharge planning is a mess, and with few exceptions, the press has yet to tell these stories.
When I was transferred as a patient from a New York teaching hospital to a long-term acute care facility in New Jersey, my family had no idea what this was. Neither did I when I regained consciousness and was returned to the LTACH after another hospital stay. I had done the major stories on long-term care facilities and thought I knew the industry, but I, too, struggled to understand what kind of facility I was being sent to. It wasn’t until I got home did I learn an LTACH is a relatively new designation for facilities that treat sicker patients for an average of at least 25 days at a time and are reimbursed by Medicare.
The UHF found that too often families discover that hospitals limit the options for them, which, of course renders even the best rating scheme useless and prevents any kind of meaningful patient shopping for post-acute care. When my daughter called Manhattan facilities looking for care, most wouldn’t even take her calls. “I called around and realized you cannot find a place on your own,” she said. “That’s not how this works.”
The transferring hospital and potential new ones seemed to be working together to control where I would get my care. David Lipschutz, associate director of the Center for Medicare Advocacy, told me hospitals have electronic systems and share profiles of patients they are about to discharge. “They shop the patient around and say, ‘This is the facility to go to.’” When hospitals are running up against the limits of what Medicare pays, they have an incentive for moving the patient out.
The United Hospital Fund reported that even though hospital staff often stressed patient choice, patients and their families felt, in fact, they had little choice. The “choices” they were given were often faux choices. New York state regulations require hospitals to give families lists of post-acute care facilities that fall within a patient’s insurance network. If families visit one of the facilities and like it, and there’s no bed available, hospitals send them to an alternative place that does have one. Looking up ratings in a news story or on the CMS website is a useless exercise. Essentially there is no choice. Nor is there much choice when a provider list is out-of-date — a common problem.
When the time came for me to go home, discharge personnel at the hospital handed me a list of 38 home health agencies, many for-profit. I was supposed to pick one. That was an impossible task since I had no Internet access, no way to examine the Medicare’s home care ratings, which I had always thought were less-than-robust any way, make phone calls to track down satisfied or unsatisfied clients, or do anything to make an informed decision.
In the end I chose the Visiting Nurse Service of New York, a nonprofit group, because I had interviewed their staff members over the years.
It would have been much more useful for someone to have explained the process of going home, receiving home care through Medicare, and how these services fit together and were paid for. Long after I had recovered, a doctor explained to me how all this worked.
Journalists can do what that doctor did for me and help their audiences understand the process. One day while waiting for my turn with a physical therapist, a patient in the waiting room approached me. She was 57 and had suffered a stroke. She knew I was a writer because we had talked at another session. “Please tell us how this works,” she said. “We don’t understand any of it.”
Veteran health care journalist Trudy Lieberman is a contributing editor at the Center for Health Journalism Digital and a regular contributor to the Remaking Health Care blog.