The Health Divide: Black people feel left out of weight-loss drug craze
(Getty Images)
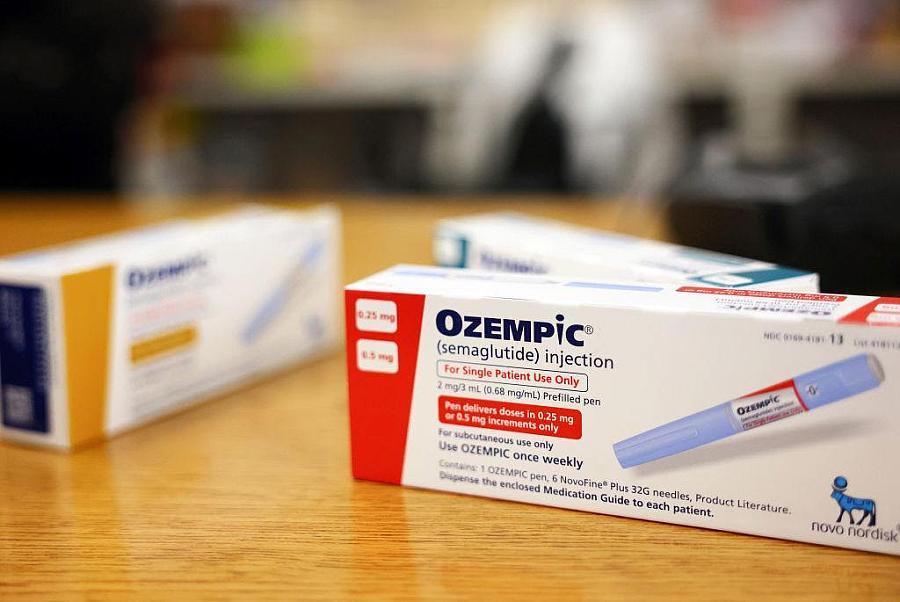
Weight-loss drugs like Wegovy and Ozempic have rapidly surged in popularity, but the benefits aren’t being distributed equally, reports Anissa Durham in a Word In Black-STAT collaboration.
“Many Black Americans … worry that their community is being left behind,” Durham writes.
These medications not only cause weight loss, they can also improve health in other ways, such as by lowering risk for stroke and heart attack.
But several factors impede Black access. People in minority groups are less likely to be prescribed these drugs than whites.
“I think the conversation is definitely missing in the Black community,” said Dr. Fatima Cody Stanford, an obesity specialist at Massachusetts General Hospital. Patients may be unaware that the medicines cause side effects and must be taken long-term for any weight loss to last.
Even for those in the know, access can be challenging. High demand has created shortages, with some patients waiting months to fill prescriptions.
And the sticker price, without insurance, is nearly $1,000 for a one-month supply.
“If you don’t have insurance or good insurance, it’s going to be more challenging to access it,” said Jonathan Gustave, an Orlando man who has Type 2 diabetes but has had difficulty filling his Ozempic prescription.
The need in the Black community is great: Non-Hispanic Black Americans have the nation’s highest rates of obesity. Black Americans, along with American Indians and Native Alaskans, have the highest rates of diabetes as well.
And social factors, such as lack of access to stores that sell fresh food and calorie-heavy church luncheons, can also contribute to weight gain in Black communities, Durham reports.
Black people with obesity face a double bias due to both race and weight, Durham notes, and Black women deal with even more body image distortion than Black men.
That bias persists even in the doctor’s office, where clinicians spend less time with patients who have obesity and are more likely to attribute health problems to their weight.
For example, Durham interviewed more than a dozen Black people about weight, and two women mentioned delays in diagnosing polycystic ovary syndrome, which can cause weight gain.
Yet the access to the new medications is not on par with the need in the Black community.
“If I could just get Ozempic, you have no idea, I’d take it in a heartbeat,” said Michel Hobson, a 67-year-old Texan with Type 2 diabetes. But the costs, she said, are well beyond her reach.
Black Americans less likely to join residential care communities
There’s a stark divide between white and Black Americans who need help with daily living, according to a joint AP News-CNHI News investigation.
White people who need assistance, such as in-home dialysis, are most likely to enter residential care communities, such as assisted living. These create community and prevent isolation while allowing some continued independence.
Black adults, in contrast, are more likely to enter nursing homes, which provide more comprehensive care, but lack those benefits of independence and community, report CNHI’s Carson Gerber and AP’s Nicky Forster and Devi Shastri.
The trio analyzed data from the Center for Disease Control and Prevention’s 2020 National Post-acute and Long-term Care Study.
“The bottom line is white, richer people have a solution now — which is these incredible assisted-living communities — and minorities and low-income people don’t,” said Jonathan Gruber, an economist at the Massachusetts Institute of Technology.
The reasons behind the disparity include the costs: most people pay privately for residential living, while Medicaid can cover nursing homes.
Other reasons are murkier, the reporters write. Geography may play a role, but it’s unclear if assisted living options are sited near or far from Black communities; the government doesn’t maintain a list that could be mapped.
Cultural factors could also contribute: Black families may prefer to care for family members themselves for as long as they can manage.
For example, Steven Nash, who runs a Black-owned nursing home in the Washington, D.C., area, cared for his own father at home.
“We try as hard as we can to honor the wishes of our elders,” Nash said.
Advocates urge changes to tissue donation rules for gay men
Gay men can donate blood. If they die, their family can donate their organs. But that’s not the case when it comes to tissues such as skin or corneas.
Frustrated advocates say it’s past time that disparity was eliminated, reports Rae Ellen Bichell at KFF Health News.
Specifically, advocates want the U.S. Food and Drug Administration to change what’s called the deferral period for tissue donation. Currently, a deceased man cannot be a tissue donor if he had sex with another man during the five years preceding his death. This results in rejection of hundreds of cornea donors each year. Advocates want that changed to just 90 days.
The restrictions were enacted three decades ago to prevent HIV transmission, but Dr. Michael Puente Jr., co-leader of the “Legalize Gay Eyes” campaign, said they’re “nonsensical” in an era with advances in HIV testing.
“A gay man can donate their entire heart for transplant, but they cannot donate just the heart valve,” said Puente, who is gay.
There is no known case of HIV transmission by cornea, Bichell notes; the tissue contains no blood or other body fluid.
The five-year restriction is not only discriminatory but impractical, since it expects grieving relatives to be aware of a deceased individual’s lengthy sexual history, said Kevin Corcoran, head of the Eye Bank Association of America.
The issue has been in question for some time: In 2021, members of Congress sent a letter to the FDA stating “policy should be derived from the best available science, not historic bias and prejudice.”
The FDA does have the issue on its agenda, but the it has been there since 2022 without action, Bichell notes.
Advocate Sheryl J. Moore reported that when her teenage son, Alexander “AJ” Betts Jr., died, she was able to donate his organs but not corneas simply because he identified as gay, even though she told officials he wasn’t sexually active.
“I felt like they wasted my son’s body parts,” Moore told Bichell. “I very much felt like AJ was continuing to be bullied beyond the grave.”
Families of color struggle to get cystic fibrosis diagnoses for newborns
Screening of all newborns for cystic fibrosis (CF), a potentially fatal lung disease, is meant to ensure babies with the condition are diagnosed early and treated as soon as possible. But for some families of color, the universal testing has backfired, making diagnosis harder, reports Liz Szabo at The New York Times.
Some states implemented screening in the 1980s, with the final states starting in 2010, making the practice nationwide. The first screen is for high levels of a blood protein that often accompanies CF. If that’s positive, physicians proceed to genetic testing.
But the gene tests were developed mainly based on data from white children, Szabo reports. They don’t include all mutations that can underlie the disease, particularly those that occur in people of African, Asian, or Latin American descent.
The result is that the genetic tests miss only about 5% of white babies with cystic fibrosis, compared to 44% of Asian babies, 22% of Black babies, and 14% of babies who are Hispanic, Native American or Alaska Native.
Moreover, physicians have been taught that CF almost only affects white people.
This is a misconception. In fact, universal screening contributed to a rise in new CF diagnoses among Black and Hispanic people. Their share of new cases rose from 9% in 2000 to 14% in 2020.
Misunderstandings about CF and overconfidence in medical tests means that physicians who see a negative test result from a baby of color may dismiss parents’ concerns, or even blame parents for their infant’s problems, Szabo reports.
“Parents are told, ‘Your child had a normal newborn screen. You are crazy,’” said Dr. Meghan McGarry, a pediatric lung doctor at Seattle Children’s Hospital. “It’s becoming a barrier to care. That’s the opposite of what it was meant to be.”
Delayed diagnosis by just a couple of months can increase a person’s risk for lung problems and death.
Awareness is a key part of the solution. For example, Ann & Robert H. Lurie Children’s Hospital of Chicago has instituted an awareness campaign, funded by the CDC, to ensure testing happens within two months of birth and educate physicians about risk of false negative results in non-white babies.
The Cystic Fibrosis Foundation also has plans to publish screening guidelines promoting racial equity this fall in the hopes of educating both physicians and patients. The foundation already has a page about misconceptions, noting that more than 15% of the patients in its registry identify as people of color.
Dr. Susanna McColley, a pediatric lung doctor at Northwestern University Feinberg School of Medicine, told the Times that any child with symptoms of CF, or a sibling with the condition, should receive the definitive diagnostic test for excess salt in their sweat.
Communities of color overlooked on long COVID
People of color are particularly likely to have long COVID symptoms dismissed by the medical community, reports Akilah Johnson at The Washington Post.
Data so far indicate that long COVID is spread equally among ethnicities. But researchers told Johnson that people of color often don’t have a formal long COVID diagnosis, preventing them from being counted and from receiving appropriate treatment as well as social or financial assistance.
“If we are only engaging white, middle-class, English-speaking America in treatment, we don’t yet understand the full impact,” said Linda Sprague Martinez, who heads the Health Disparities Institute at UConn Health.
Johnson points to racism and physician bias as reasons Black patients are more likely to be dismissed in routine care, and probably when reporting long COVID symptoms as well.
People of color and non-English speakers may not even hear the term “long COVID” or other key information from medical providers, Johnson reports.
In contrast, affluent or white individuals may be able to visit multiple physicians until they obtain the care they need.
The National Institutes of Health’s large RECOVER study of long COVID is also working with a racially skewed population, with inadequate representation of Black, Latino, and Native American people as well as rural, immigrant, LGBTQ+ and disabled individuals. (The $1.6 billion NIH study has been criticized for its ponderous pace, lack of practical results and treatments, and for testing exercise therapies that could worsen the condition in subjects, according to a STAT-MuckRock-Sick Times investigation by Betsy Ladyzhets.)
Pediatrician Dr. Kanecia Zimmerman, who runs the RECOVER coordinating center at Duke University, said her group is trying to reach diverse communities but acknowledged, “We’re not where we want to be.”
Diagnosis can make a huge difference. It did for Chimére Sweeney, a Black former middle school teacher, though only after a two-year odyssey.
“I cried that day because I was like, ‘Thank you, God!’” Sweeney said. “Having that diagnosis got the ball rolling on everything else for me — Social Security, this retirement.”
From the Center for Health Journalism
- Webinar Jun 12, 10 a.m. PT: “The Next Pandemic: Can We Avoid Repeating History?” Bird flu is spreading through cows and has infected several people. Experts will discuss the latest developments and how reporters can keep a spotlight on emerging threats and our collective readiness. Sign-up here!
- Apply for our Data Fellowship! The Fellowship trains journalists to “interview the data” and “bulletproof” their reporting for accuracy. Graduates produce a major investigative or explanatory health reporting project or a series of data-driven health stories. The Fellowship includes a $2,000 stipend, one week of extensive training, and five months of professional mentorship. Applications due July 10; fellowship week Oct. 7–10.
What we’re reading
- “In low-wage jobs, working while Black means showing up sick,” by Jennifer Porter Gore, Word In Black
- “Racial disparities in cognitive outcomes tied to early life experiences,” by Sophie Putka, MedPage Today
- “NIH-funded clinical trials often miss racial, gender diversity enrollment goals, report finds,” by John Wilkerson, STAT
- “Medicaid unwinding deals blow to tenuous system of care for Native Americans,” by Jazmin Orozco Rodriguez, KFF Health News
- “How can we combat he rise in suicides among Black youth? An interview with Dr. Yolanda Lawson,” by Courtney Wise, MindSite News
- “Cancer patients get poorer care at hospitals serving minority communities,” by Dennis Thompson, HealthDay

