Cities are trying to address the staggering impact of asthma. The problem: Our healthcare system isn't set up to address underlying triggers
Talis Shelbourne reported this project on the intersection of asthma, housing and health systems with the support of a grant from USC Annenberg Center for Health Journalism's 2022 Impact Fund for Reporting on Health Equity and Health Systems.
Other stories include:

Laketa Watts, left, director of Essentially Empowered, a community organization, and Sherri Sherri Ohly, director of the Envision Community Health Worker Training Center, holds Watts’ son Isaiah at Watts’ home in Milwaukee. The women are health care advocates working to bring awareness about the concerns of asthma on a local and national level. Ohly trained Watts in 2018 as a community health worker, who would later created Essentially Empowered, a program that she oversees for asthma prevention.
ANGELA PETERSON / MILWAUKEE JOURNAL SENTINEL
Asthma cost the U.S. economy $81 billion in 2013, CDC researchers estimate.
But its costs aren’t solely measured in dollars and cents.
Shante Brown, a Bay View High School student, lost her mother to an asthma attack when she was just a preschooler.
Shante’s own asthma was controlled as a child but worsened as she matured into a teenager.
Working at a local fast food restaurant increased Shante’s exposure to grease and particulate matter. Spending more time in friends’ homes, away from her aunt’s clean and tidy house, increased her exposure to dust and other irritants.
By age 17, Shante was using her rescue inhaler regularly and her aunt, Antoinette Chapman, described the teenager’s asthma as “severe.” In December 2019, Shante was hospitalized in Children’s Wisconsin for her asthma and fell into a coma.
She recovered, but the asthma remained uncontrolled.
One early August morning in 2021, she collapsed in the bathroom of a friend’s house, gasping for air. Her friend’s mother tried to administer a breathing machine. Another friend performed CPR. But just an hour and a half later, Shante stopped breathing.
Shante Brown, a Bay View High School student, lost her mother to an asthma attack. Shante suffered an asthma attack in 2021 and died. COURTESY OF ANTOINETTE CHAPMAN
Although such asthma deaths are rare, they still happen, said Jasmine Zapata, the Wisconsin Department of Health Services’ chief medical officer of community health.
“I will never forget, I was doing a rotation in the pediatric ICU, and there was a young girl who got air-flighted in because she was in a life-threatening situation due to an asthma attack,” Zapata recalled. “She almost died. She was very, very critically ill.”
Zapata is working to help expand Wisconsin’s Asthma Care Program with Christine Rameker, the state’s asthma program manager.
For many public health experts, the expansion is a long time coming.
Asthma, a respiratory condition characterized by chronically inflamed and hyperactive airways, is a deceptively complex disease. Poorly controlled asthma is common in low-income areas, where specialists are often out of reach and housing is frequently substandard.
Asthma sends residents from predominately Black ZIP codes to the emergency department at rates 10 or even 20 times higher than it sends the residents of affluent suburbs, Wisconsin Hospital Association data shows.
Despite this disparate impact on communities of color, the city of Milwaukee has failed to implement a citywide initiative to address uncontrolled asthma.
At a time when many cities nationwide are exploring strategies to reduce uncontrolled asthma, Wisconsin has a breadth of solutions to include in its expanded program, such as increasing the ranks of community health workers, conducting home-based interventions, implementing stronger housing and health policies, and using updated technology for asthma education.
Community health workers pivotal for sustainable care
Sherri Ohly is the director of the Envision Community Health Worker Training Center, a University of Wisconsin Population Health Institute project which operates under a three-year U.S. Centers for Disease Control and Prevention grant.
Community health workers, Ohly said, are integral for addressing health literacy in their communities, and they tend to provide more sustainable support to families than an emergency room doctor can.
“Our healthcare system is so: ‘Here’s the information, here you go, here it is,’” Ohly said. “(When) community health workers come to a family, they look at what’s the crisis that needs immediate attention? And then as they go further, they can dive deeper and figure out what’s triggering these asthma attacks. All of that takes time and trust. And that’s not what health systems are designed to do in a clinical setting.”
Prospective community health workers often choose a specialty, such as health education, coaching skills or care coordination. And because many of them come from the communities they serve, they are able to act as translators for patients, both literally and figuratively.
“The lingo that’s used within healthcare and public health, that is sometimes really difficult to digest even when we’re speaking the same language,” said Morgan Krhin, a community health worker coordinator for Wisconsin’s Chronic Disease Prevention Program. “Community health workers reinterpret that to make it digestible, easy to understand and less intimidating for the community.”
Community health workers are often funded with short-term grants, which Krhin said deters people from the profession and leads to shortages.
“Because they’re coming from the same communities in which they’re serving, they are not paid in an equitable way, compared to other health professionals who are working in similar spaces,” Krhin said.
Because community health workers do not have a clinical role, they are frequently treated as novelties, which complicates efforts to ask health systems or insurers to fund the position more permanently.
Without community health workers who look like and have the trust of the communities where they work, the task of health education fall to others, like Francis Starms Discovery School nurse Ashley Capodarco.
“I’ve noticed and heard from families that they’re more willing to open up and listen to someone who is from their neighborhood and has the same background,” Capodarco said. “I think there needs to be a lot more people of color presenting medical information.”
Home-based interventions must be part of the solution
The CDC suggests that home-based interventions are key to reducing symptom days, improving quality of life and lowering missed school days.
Communities often fund these programs through grants, such as the BUILD (Bold, Upstream, Integrated, Local, Data-driven) Health Challenge, a national coalition of health insurers, foundations and community organizations that award local agencies money for health equity initiatives. The organization has had several iterations of its awards in Portland, Seattle, Des Moines, Oakland, Denver, Albuquerque, Chicago, Detroit, Cleveland, Pasadena, the Bronx and Baltimore, among other cities.
West Philly was one of those communities.
Philadelphia is home to many of the same conditions found in Milwaukee — an aging housing stock, a history of housing racism and fragmented attempts to address health disparities. After receiving a BUILD Health Challenge Grant, Children’s Hospital of Philadelphia added home remediation to its Community Asthma Prevention Program (CAPP).
Partnering with Rebuilding Together Philadelphia and Habitat for Humanity, the new iteration, called CAPP Plus, helped West Philadelphia families with uncontrolled asthma repair subfloors, plumbing and duct systems and address pest infestations, mold and/or dirty air ventilation systems.
The CAPP was run by Dr. Tyra Bryant-Stephens, a primary care physician. More than two decades earlier, she was teaching asthma education classes to reduce emergency room visits for asthma.
Tyra Bryant-Stephens runs Children’s Hospital of Philadelphia Community Asthma Prevention Program. CHILDREN'S HOSPITAL OF PHILADELPHIA
At the classes, she noticed: “(When) we talked about environmental triggers, parents would start to zone out. And we realized it was … because they didn’t have money. They were a tenant and they just felt so totally helpless.”
At the time, the hospital’s community health workers were conducting home assessments where they would provide smoking cessation resources, vinegar cleaning solutions, HEPA vacuum cleaners and instructions on how to reduce mold and pests.
But it often wasn’t enough.
“Over the years, we were struck by how our community health worker would say, ‘I gave them the stuff, but there’s still a hole in the ceiling’ or, ‘There’s still a big leak,’” she recalled.
That’s when Bryant-Stephens convinced Children’s Hospital to participate in a BUILD Challenge grant, which required a hospital match.
The expanded program, CAPP Plus, only applied to West Philly residents who had two asthma-related emergency room visits or one hospitalization in the past year and who would commit to staying in their homes for a minimum of three years. Participants were able to receive roof repairs, duct cleanings, mold remediation and other large repairs.
Children’s Hospital saw such positive returns, it began fully funding the program.
“We finished our 100th home in December. I went out to talk to the parent to hear her views and she said, ‘This would have never happened,’” Bryant-Stephens recalled. “She’s a single mom with three kids. She said … ‘I would try to save a little bit, but then something would come up.’ Parents making as little as they do and then having low wages, it’s just hard – unless they get a windfall, or someone comes along and helps them out.”
Bryant-Stephens is hoping CAPP Plus will reach 40 homes this year and expand to include renters. Renters’ landlords must have four or fewer units, live in the neighborhood and be on good terms with the tenant, who must agree to stay at least three years.
The investment, Bryant-Stephens said, is worth it.
“There should be a lot more investment,” she said. “Eighty percent of the dollars we’re spending should be on social determinants of health rather than hospitalization.”
Successful programs show significant return on investment
Amy Kind, associate dean at the University of Wisconsin-Madison’s School of Medicine and Public Health, said programs such as CAPP Plus are rare because the medical field is just now starting to realize the value of collaborating to address social determinants of health.
“(There’s) this issue of turfism — 'I work on hearts, not housing’ or, ‘That’s not my thing, it’s a housing thing,’” she said. “It should be everyone’s problem. And making more people aware that poor quality housing could affect pulmonary disease should be just as important as the inhaler or the pill.”
Amy Kind, professor at the University of Wisconsin School of Medicine and Public Health. ANGELA PETERSON / MILWAUKEE JOURNAL SENTINEL
Many physicians in Milwaukee are unsure how or where to send their patients for help outside of the medical realm, further illustrating the need for a more holistic approach to address chronic diseases.
Some communities have taken that approach.
The Greensboro Housing Coalition mounted a public pressure campaign against one apartment complex owner whose tenants were disproportionately visiting the hospital for asthma-related issues. In partnership with community groups, Cone Health and the University of North Carolina-Greensboro, the complex was eventually sold to a landlord who has brought the building up to code. Asthma-related hospital visits from that complex have declined.
Several other cities — including two in the Midwest — have taken advantage of the BUILD Health challenge to address asthma.
In Cleveland — a city with high rates of lead poisoning, asthma and chronic obstructive pulmonary disease (COPD) — three local organizations received a BUILD Health challenge grant of $250,000. Grant recipients remediated 57 homes by:
- Performing a free home environmental assessments
- Conducting proactive housing inspections
- Creating complete rental registry
- Using home violations to identify hotspots of unhealthy housing
- Enforcing code compliance
The program’s success also led the public to support a tax increase for city services. And the city raised an additional $2.3 million from landlords’ rental registrations.
Des Moines is another city with a large renter — and rent-burdened —population and old housing stock prone to developing asthma irritants such as mold. Des Moines received a BUILD Health Challenge grant in 2015, and three health systems worked with the local health department and Polk County Housing Trust Fund to create the Healthy Homes Des Moines program. The program is unusual in that it uses public funds to remediate rental properties at no cost to families.
Since the program’s implementation, asthma-related emergency department visits decreased from once every 60 days to zero, children had an average of six additional symptom-free days and the children’s legal guardians missed 70% fewer days of work per month due to asthma.
Carolyn Schaefer, a registered nurse and healthy homes specialist, and Mike Miller, a city of Des Moines code enforcement officer inspect a home for environmental causes of asthma March 1, 2016, in Des Moines. In 2016, Des Moines, Iowa, launched a program to find and fix household problems that contribute to childhood asthma. It was supported by Polk County and the city’s three main hospital companies, Mercy, UnityPoint and Broadlawns. KELSEY KREMER / REGISTER
Along with these outcomes, the program also has changed the local inspection department. Partners lobbied for the addition of a local options sales tax to help fund the department, inspectors were educated on asthma triggers and the department is currently exploring a “healthy and safe” seal of approval for landlords who volunteer for a thorough inspection and pass.
Other healthy home programs throughout the country show home-based interventions have good health and economic outcomes.
One home-based intervention asthma program in Minnesota produced a return on investment ranging from $5.25 to $1.61 for every dollar spent, and reduced missed school and work days over a three-month period.
University of Massachusetts’ Lowell Healthy Homes Program focused on addressing environmental triggers in housing — mold, mildew, pests and dust mites — by providing asthma education, specialized vacuum cleaners, pest control items and property manager training. The program cost $36,000 and saved $71,000 in health care costs and the number of emergency room visits dropped 80%, according to a 2014 study.
Policy makers have the power to make the city healthier
Systemic inspections, which involve city inspectors visiting rentals throughout the city on a rotating basis, has been proven to reduce the prevalence of substandard housing.
The use of rent abatement and withholding programs in Baltimore, Columbus, Los Angeles and Detroit helped strengthen this housing strategy, a 2022 study on housing code violation and asthma found.
Greensboro’s Rural Unit Certificate of Occupancy ordinance, enacted by the city council in 2003, required mandatory inspections for virtually all rental housing. The number of housing units with code violations dropped 77% in the first eight years, and the city was able to bring more than 8,700 properties up to minimum standards in four years. The ordinance was eliminated in 2011, and complaints from renters went right back up.
The Asthma Free Housing Act, passed by the New York City Council in 2018, requires landlords with three or more apartments to address all conditions — including pests and mold — that could act as triggers.
Not all such systemic housing inspection programs have successful outcomes. For example, after such a program was instituted in Boston, the number of violations barely changed. Researchers said the reason was because it required an inspection too infrequently — once every five years — and allowed landlords to use private inspectors.
Katharine Robb, a post-doctorate fellow at Harvard University with a background in public health, said today’s inspectors focus too much on code compliance, which often hurts residents.
“There’s often this perception that housing inspectors are really there just to take a very punitive approach,” she said. “The enforcement of housing codes often leads to (the) displacement of residents or evictions. Landlords are induced to make improvements to homes and that costs money. They raise rents, or landlords retaliate against tenants.”
Rethinking Medicaid reimbursement is another policy tool that could avoid significant health care costs down the road.
Medicaid reimbursement means providers receive a pre-determined fee when Medicaid-eligible residents use particular services. The state is then reimbursed by the federal government.
Obtaining Medicaid reimbursement for services, large and small, could significantly help low-income residents access services vital to improving asthma outcomes. Hospitals, for example, that employ community health workers could receive Medicaid reimbursements for them.
Gary Steven, founder of the Allergy, Asthma & Sinus Center in Greenfield, is particularly excited about the potential of Medicaid covering the costs of a tool that could help patients more consistently — and less expensively — keep track of how asthma is affecting their body. The tool is a spirometer, a home-based machine used to test lung function that is typically only found in specialists’ offices.
Medicaid reimbursement can also help cover the cost of home intervention programs, as the 2015 Green & Healthy Homes Initiative on asthma suggests, by making it part of “targeted case management” and eligible to be waived. Wisconsin is considering such a program as part of expanded asthma-control efforts.
Thirteen states already use Medicaid reimbursement for home-based asthma services, a National Center for Healthy Housing survey found, with 69% covering home assessments, 54% covering education about triggers, 38% covered low-cost supplies and 15% covered structural remediation. The cost range of visit reimbursements was $81-$200.
Technology key for tracking, education patients
Effective strategies to reduce uncontrolled asthma aren’t just in homes, hospitals and the halls of policymakers — they can also be found in technology.
Steven built his own database to track the number of emergency room visits his patients have made.
In Louisville an initiative to add sensors in inhalers helped asthmatics track their inhalers and helped health care providers track how frequently they used them. The initiative, “AIR Louisville,” led to a 78% reduction in rescue inhaler use and a 48% improvement in symptom-free days, a 2018 study found.
Dr. Sunit Jariwala, the medical director of digital transformation at New York’s Montefiore Medical Center. PHOTO COURTESY OF SUNIT JARIWALA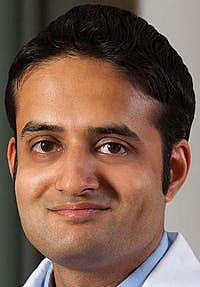
Dr. Sunit Jariwala, the medical director of digital transformation at New York’s Montefiore Medical Center, tackled the extreme asthma disparities in his Bronx patient population by creating an asthma-focused phone app. The app instructs patients on medications use, proper inhaler technique, different asthma triggers and how to develop an action plan. According to a study of 39 pediatric patients in that area, emergency department visits and prednisone use decreased significantly following use of the app.
The app, ASTHMAXcel, started with a PowerPoint.
Jariwala was working in the Bronx, where asthma-related hospital visits were three times the state average. Galvanized, he and a pulmonologist formed the Montefiore Asthma Center and started delivering a PowerPoint with information about asthma to doctors and patients.
But his patients wanted to download it.
Steered by the National Asthma Education and Prevention Program, Jariwala and his team integrated feedback from patients, clinicians, psychology professor Jonathan Feldman and pediatrics professor Marina Reznik to build the app.
The team received 14 grants for $2.5 million from the federal government, American Lung Association, American Academy of Allergy, Asthma & Immunology, and other partners.
“It’s been all user-centered design,” Jariwala explained. “It’s fully based on the national guidelines, but it’s also contextual in the sense that we highlight features like pollen counts.”
The app also helps remind asthma patients to use a “peak flow meter,” a device that measures exhales and identifies when they are likely to have an attack.
The app now has a pediatric version and has even been used for different diseases.
Improved systems could save lives
Dorian James has spent nearly 30 years working with asthma patients. He worked at St. Joseph in the 1990s, the Allergy, Asthma & Sinus Center in the 2000s, and spent five years at Children’s Hospital’s Community health asthma management program (CHAMP).
During that time, he observed how often asthma is mistaken as a simple disease, despite its complexity.
Dorian James former Community Health Asthma Management Program (CHAMP) . ANGELA PETERSON / MILWAUKEE JOURNAL SENTINEL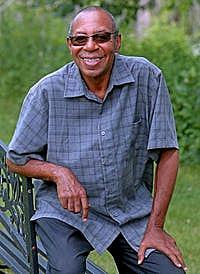
For example, James said important asthma management components, such as inhaler technique, are often oversimplified in emergency rooms. Children often need spacers to ensure the full dose of medication is being delivered.
“There’s a large number of the asthma population that is unstable for no other reason than because they’re using their inhaler improperly,” James said.
Everyone is different, James said. “It’s not only different from person to person, but it can be different in the spring and fall when allergens are out versus in the summer when it’s hot or winter when it’s cold. It can be different (depending) on the time and day. That’s the degree of sensitivity.”
In many ways, the relatively new commitment to improving asthma outcomes represents a far cry from how health systems responded in the past.
James said the asthma clinic at St. Joseph was so successful, it began cutting into profits from emergency room visits.
“We were having such success and the ER rates were dropping so significantly, they decided to close it,” he said. After the Affordable Care Act passed, a provision made the hospital liable if someone returned to the hospital with the same issue within a certain time frame. By then, James had left, but he said two people he trained reopened the clinic. The hospital is now under new ownership.
James said he believes the asthma program at Children’s Wisconsin is a good model to follow. It features a team with one specialist to concentrate on the disease, a nurse to educate patients, a social worker to help with social determinants of health and a psychologist to help patients with the impact of asthma. The only thing missing, he said, is home remediation, which is included in the state's plans for expanding its efforts.
Andrew Beck, a pediatrician at Cincinnati Children’s Hospital, has seen the results when a hospital devotes significant resources to improving the outcomes of asthma and other chronic diseases.
“Think about system-level costs,” he said. “If you reduce morbidity, (emergency department) visits, hospitalizations and you keep children in school and parents at work, that saves a heck of a lot of money to the broader system.”
More importantly, reprioritizing diseases like asthma can improve someone’s quality of life and maybe, even save their life.
“Inequities are real. If you think about … the years of productivity lost, not to say anything of the emotional loss that a premature death could have, I’m sure it’s measured in billions, if not trillions,” he said.
TALIS SHELBOURNE reported this project on the intersection of asthma, housing and health systems with the support of a grant from USC Annenberg Center for Health Journalism's 2022 Impact Fund for Reporting on Health Equity and Health Systems.
Meet the team- Reporter Talis Shelbourne
- Editing Thomas Koetting
- Photos & Video Angela Peterson
- Data & Graphics Daphne Chen and Bill Schulz
- Digital Production Jordan Tilkens
[This article was originally published by Milwaukee Journal Sentinel.]
Did you like this story? Your support means a lot! Your tax-deductible donation will advance our mission of supporting journalism as a catalyst for change.

