Doctors still foggy on valley fever symptoms
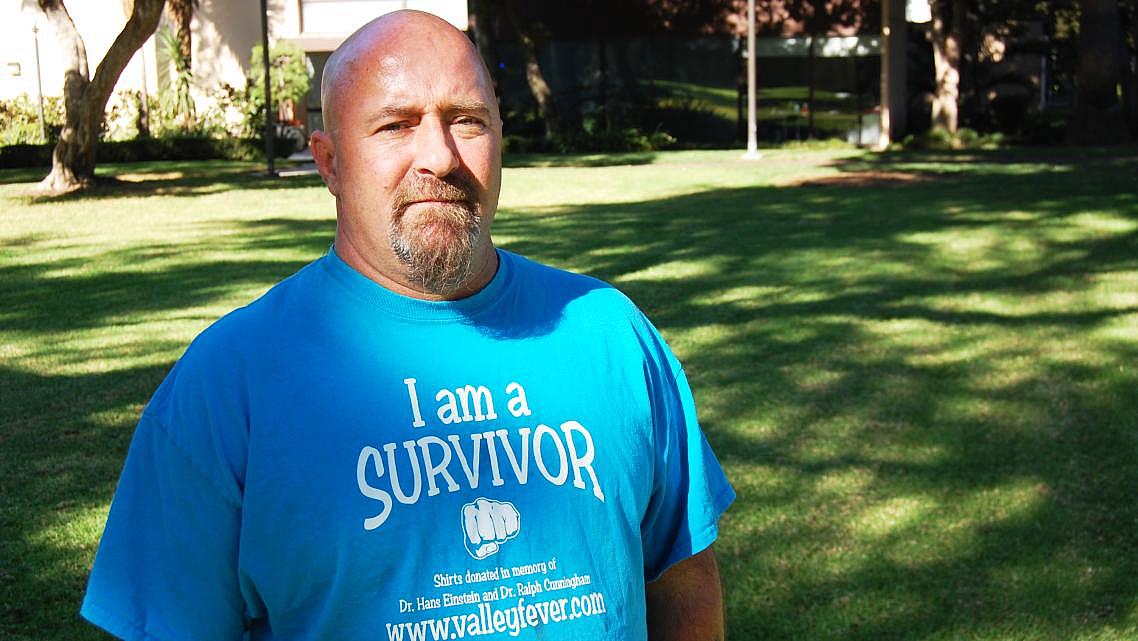
Rick Parker, a Southern California resident who was infected with valley fever while visiting the Mojave Desert in 2014, was misdiagnosed by doctors at least twice before they made an accurate diagnosis.
(Photo: Olivia Henry/The Center for Health Journalism)
Click HERE for Spanish version.
Rick Parker knew he had valley fever, but his doctors wouldn’t test him.
The 48-year-old was prospecting gold in Mojave, California, in 2013 when he inhaled some dirt. Not long after, he became fatigued, developed a cough, had lung pain and experienced chills..
The Phoenix native had heard all about valley fever while living in Arizona, where the disease infects thousands annually. But when he asked his doctors in Torrance, California, to test him, they refused.
Emergency room doctors at Torrance Memorial Medical Center told him that nobody in Los Angeles develops valley fever and diagnosed him with tuberculosis. Then his general practitioner said he had pneumonia, then tuberculosis again. Parker said she was about to begin treating him for lung cancer when he locked himself in her office and demanded that she test him for valley fever.
“I knew what I had, and I wasn’t going to put up with a lung cancer misdiagnosis and have them remove a lung for no reason whatsoever,” Parker said. After his tests came back positive, his general practitioner called to apologize, he said, and admitted he was her first valley fever patient.
“It’s frustrating, and it’s even more frustrating when you know what you have and nobody will listen,” Parker said.
Parker faced one of the most challenging aspects of valley fever: a lack of awareness among physicians, the very people whom patients tend to trust the most.
Valley fever, or coccidioidomycosis, is caused when fungal spores common in the southwestern United States get released into the air and inhaled. Most people don't develop symptoms, but others come down with a fever, cough, extreme fatigue and a rash, among other symptoms. In rare cases, the fungal spore can spread to the bloodstream, infect other organs, and cause cocci meningitis, leading to a lifetime of health issues and potentially death.
Cases have spiked recently, with infections in California last year reaching the highest number ever recorded.
All local doctors in California’s Central Valley and Arizona’s valley fever corridor, through Maricopa, Pinal and Pima counties, should recognize valley fever symptoms, public health officials say. But that’s challenging in a medically underserved region known for having a revolving door of new doctors. Once those doctors begin to understand the disease and become good at diagnosing it, they often relocate for new career opportunities, public health officials say.
Despite the high infection rate in Kern County and throughout Arizona, there’s no mandate that all new doctors undergo training on valley fever and how to diagnose it. There are no agreed-upon best practices for raising awareness among doctors. And it’s unclear whether medical professionals even know when valley fever cases are surging because counties have no uniform guidelines for when to declare an epidemic and are not equipped to disseminate the message effectively.
When cases spike, or when labs receive more requests for valley fever tests, the Kern County Public Health Services Department issues bulletins to hospital systems and health insurers. Whether they in turn notify other medical professionals is a mystery.
Health Net and Blue Shield in California – which insure roughly two-thirds of the Kern County market – did not respond to repeated requests for comment. Kaiser Permanente declined to comment for this story, providing only a prepared statement affirming its commitment to continuing physician education on relevant clinical issues, including infectious diseases such as valley fever.
House Majority Leader Kevin McCarthy, who formed a Congressional Valley Fever Task Force in 2013, said in an August interview that educating doctors in areas where the disease is endemic could lead to the greatest improvement in reducing the toll.
“Where do we go when we don’t feel good? The medical community,” McCarthy said. “They have to have the awareness programs to educate the medical doctors.”
When asked whether he would push for legislation that would mandate training for doctors new to areas where valley fever is endemic, he instead urged insurers to put pressure on health plans. Insurance networks, McCarthy said, need to do more to educate their doctors.
“A dream scenario would be every local physician being fully aware of valley fever as they’re incoming and new to our area, and that’s something we’re always working diligently on,” said Michelle Corson, a public relations officer for Kern County Public Health Services.
Dr. John Galgiani, director of University of Arizona’s Valley Fever Center for Excellence, recommends going even further, with regular briefings for doctors in endemic areas.
“Going to a course sounds good, but that information gets catalogued in the backs of doctors’ minds and doesn’t necessarily come bubbling up to the surface if the next patient in their clinic has valley fever,” he said.
Instead, repetition is key, Galgiani said.
“Changing practices requires constant and repetitive attention to staying on message and telling people this is important,” Galgiani said.
For more stories in this series, click here.


