In Tennessee, there remains deep suspicion of pharmaceutical answers to a crisis that was caused by pharmaceuticals in the first place, Loyd said.
The state has strict regulations for clinics that distribute methadone. Over the years, unscrupulous pain clinics and pharmacies have drawn federal indictments for prescribing and dispensing opioids at rates topping national averages. Patients have long found themselves unable to find a local pharmacy willing to fill their buprenorphine prescription, forced to make long, daily drives to access methadone, or facing limited treatment options outside of faith-based, abstinence-only rehab.
Loyd, who recovered from opioid addiction through abstinence-only treatment, has pushed to expand access to medication in Tennessee. (He is also chief medical officer for Cedar Recovery, which operates 10 opioid treatment clinics across the state.)
“There’s a pervasive belief that you’re switching one medication for another, and if you just go to church more and pray more, it’ll just go away,” he said. “There’s also a tendency in our state to disregard what the feds say.”
‘Devastating’
When Scott learned he passed the bar exam in April 2021, he was already working at a law firm and had signed a contract to stay on once he got his license. His elation fell, however, when he received a second email from the Board of Law Examiners, telling him that his application had raised “concern” about his ability to practice law.
Before he could move forward, the board told him, he’d have to be evaluated by the Tennessee Lawyers Assistance Program (TLAP), a state-administered program that helps lawyers, judges, law students and bar applicants struggling with physical or mental disabilities, including substance use disorder. Participation in such programs can be voluntary — they offer confidential, free assistance to lawyers who need help — but they also help state boards evaluate bar applicants and monitor attorneys during disciplinary proceedings.
In addition to passing the bar exam, prospective lawyers have to demonstrate they possess the character and fitness to practice law — a high-stress, high-stakes profession, where a client’s very life can hinge on their attorney’s ability to perform their duties responsibly. To do so, applicants must provide a full accounting of past conduct, including criminal convictions and financial debts. Depending on the state, applicants might also face questions about expunged criminal charges or convictions, and mental health and substance use disorder diagnoses or treatment.
While almost all states will license people with criminal records, including felony convictions, to become attorneys, those applicants typically face increased scrutiny. There has been a national push to dismantle barriers faced by nontraditional applicants, including eliminating questions about expunged and juvenile convictions and mental health diagnoses.
In his bar application, Scott didn’t have to disclose his substance use disorder. But he did have to list every conviction, arrest and charge, including those that were expunged.
He disclosed that he had three prior low-level criminal convictions. In 1998, when he was 18 years old, he was convicted of misdemeanor criminal trespassing after he climbed through his aunt’s window to retrieve a Nintendo cartridge. In 2002, at age 22, he was convicted of driving while impaired, also a misdemeanor.
The third conviction, a misdemeanor, occurred in 2004 and was expunged from his record after he submitted his application. Scott also reported a series of other low-level charges that occurred before he sought treatment in 2011. All of them had been dismissed and most were ultimately expunged from his record. Two final misdemeanor charges, which occurred in 2019 and were pending at the time of his application, were also dismissed and ultimately expunged.
In his first meeting with TLAP that May, he said he was asked if he took any prescribed medication. He hesitated, then disclosed that he used buprenorphine. “I didn’t think it’d be as big of an issue as it became,” he said.
Soon after, he attended a brief hearing before the board. He had given them a 63-page document explaining his family history and each charge in detail, along with what he learned from each incident. The board did not mention his medication disclosure, but told him he should continue to work with TLAP.
The assistance program soon began to focus not on Scott’s criminal record but on his substance use history.
TLAP told Scott that he’d have to participate in its monitoring program and submit to an assessment at an addiction and behavioral health facility before it could make any recommendation to the board regarding his ability to practice law. He was given a list of seven approved providers to choose from. None of them were in Tennessee — one was more than 2,000 miles away, in Malibu, California — but all had experience in treating white-collar professionals, including lawyers.
Later that month, Scott paid a $2,000 fee and checked himself into the Palmetto Addiction Recovery Center in Rayville, Louisiana. By then, he’d been on his medication for more than a decade. Over that time, he’d attended counseling, passed drug screens and never relapsed. His doctor would later testify before the board that he was a “model patient.”
“I thought in my head I was fine,” Scott recalled thinking as he drove to Louisiana. “I’ve been in this treatment a long time. I’m not impaired. No one’s ever questioned my abilities.”
Once there, he underwent a physical examination, a psychiatric evaluation and psychological testing. Though drug tests revealed only buprenorphine in his system, he told staff that he had occasionally used CBD and a THC product called delta-8, both of which are legal in Tennessee, to relieve anxiety. He also disclosed he had smoked marijuana, but stopped before entering law school.
He immediately felt stigmatized, Scott said. No one at Palmetto consulted with his doctor. He was pressed to answer why he filled his prescription in Kentucky, explaining that he did so not just because he lived near the state line and it was close to the church he attended, but because Tennessee pharmacies wouldn’t fill it.
Before he left, he said, the facility’s medical director told him outright that he’d have to stop using Suboxone before he could practice. (Palmetto did not respond to requests for comment.)
Scott was stunned. Then he saw the evaluation results.
Palmetto diagnosed him with moderate opioid use disorder and moderate cannabis use disorder, issuing two recommendations: that he sign a five-year monitoring contract with TLAP and complete a TLAP-approved long-term inpatient program. That treatment, the report continued, “should include detoxification off all controlled medications including Suboxone.”
Scott’s doctor would later write a letter on Scott’s behalf stating that he disagreed with the diagnosis of cannabis use disorder and that Scott had previously been able to stop using cannabis without any difficulty. “We do not consider cannabis use to indicate a failure of a patient’s recovery process,” he wrote.
TLAP informed Scott it would stick to Palmetto’s recommendations, trapping him in a catch-22. If he didn’t attend abstinence-only treatment, TLAP would consider him noncompliant, giving the board grounds to deny his application to practice law. If that happened, he couldn’t reapply for bar admission for another three years.
But the idea of going off the medication that had given him his life back, that his doctor said was safe to continue using long term, terrified him.
“It was devastating,” Scott said. “Unless I showed signs of impairment, unless I had some kind of negative consequences from the treatment I used, why would you question it? Why would you try to make me stop?”
100% success
Addiction treatment can mean anything from equine therapy to the peer-supported spiritual programming of 12-step recovery groups. Of the treatment options for opioid addiction, methadone and buprenorphine have the “strongest scientific evidence,” said Dr. David Fiellin, director of the Yale Program in Addiction Medicine.
“Compared to ‘detoxification’ or treatments that don’t include medication, both have demonstrated that they uniformly do better with respect to keeping patients on treatment, decreasing the amount of illicit opioids that they’re using, improving their function in society, decreasing their criminal behavior, and decreasing their risk of infectious complications such as HIV,” he said.
When prescribed at appropriate doses, neither medication produces euphoria or a high, Fiellin said.
Professional organizations, however, have grappled with condoning the use of medication to treat opioid use disorder — especially in “safety-sensitive” positions, a term used to describe roles where any cognitive impairment of an employee can greatly impact the safety of others. Examples of such workers include law enforcement and doctors.
A third medication, naltrexone, has also been approved by the FDA to treat opioid use disorder. Naltrexone is not an opioid and can be administered as a monthly injection. It’s that formulation, often referred to by its brand name Vivitrol, that is often preferred by both corrections officials and professional organizations because it has less potential for abuse.
However, many addiction medicine experts consider Vivitrol to be a “second-line” medication. Research has shown that it’s much less protective against overdose, in part because it requires a patient to detox fully from opioids before beginning it, a process that can take weeks and elevates risk of relapse. That reduces a patient’s tolerance to even low doses of opioids, thereby leaving them more vulnerable to overdose if they return to use after its effects wear off.
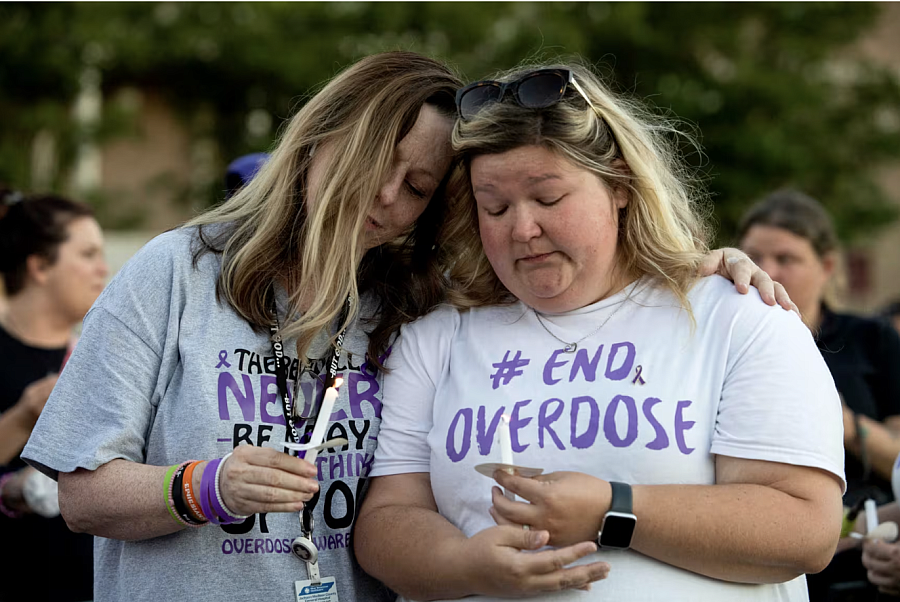
Coordinators with the Tennessee Department of Mental Health and Substance Abuse Services at an International Overdose Awareness Day vigil in Jackson, Tenn., in 2022.
Chris Day / Jackson Su / USA Today Network
Guidance recently issued by the American Society of Addiction Medicine states that patients should have access to the full range of FDA-approved medications. Regulatory agencies including state licensing boards, the ASAM said, should not “discriminate against the type of treatment an individual receives based on unjustified assumptions that certain treatments cause impairment.”
Scott began driving for Uber to make extra money for rehab and even tried decreasing his medication dosage. In the meantime, he said, he faced increasingly uncomfortable questions from his employer, who wanted him to stay on but wondered why he hadn’t gotten his license yet. He felt torn on what to do.
“I’ve had 100% success with my recovery,” he said. “What made it so hard is the science was on my side on this. What happens if I am right and then you put me into long-term treatment? Who knows what happens after that?”
He didn’t know that federal authorities at the time were actively investigating a similar scenario just two states over, in Indiana.
‘A very strong signal’
Though the protections afforded to people with substance use disorder by the Americans with Disabilities Act are more than three decades old, experts say the stigma and discrimination faced by people who use buprenorphine and methadone remains endemic.
Over the years, Friedman and her colleagues at the Legal Action Center have represented many clients who have been forced to make the choice between their legally prescribed medication and their livelihoods or access to services.
“We’ve personally witnessed people struggling with these orders to taper off,” she said. “Suffering and kind of agonizing about whether they should go back to an appropriate dose where they were thriving, or continue to taper against medical advice so that they can comply with some ill-thought-out and discriminatory order.”
Until recently, there had been little enforcement of ADA protections for people who take medication to treat their opioid use disorder. The Justice Department first published its argument that discrimination based on a patient’s use of medication was tantamount to discrimination based on disability in 2018, when it reached a settlement with a skilled nursing facility that denied admission to a patient who used Suboxone.
Since then, the agency has released guidance explaining how the ADA applies to opioid use disorder and expanded its work to various contexts, filing lawsuits and forcing entities into consent decrees.
The push to protect access to these medications is part of the Justice Department’s overall strategy to combat the opioid epidemic. Its cases have focused on people penalized for using the medications or who have been denied access to them — including in the criminal legal system, where few correctional facilities allow prisoners to use them.
“Our rigorous enforcement of the Americans with Disabilities Act should send a clear message that the rights of people with disabilities, including those with opioid use disorder, must and will be protected,” said the DOJ’s Clarke. “When it comes to opioid use disorder, we reject discriminatory and unlawful policies and practices that are rooted in nothing more than stereotypes, myths and misconceptions.”
Other federal agencies including the U.S. Equal Employment Opportunity Commission have also stepped up enforcement. But experts say it’s the DOJ that has sent the strongest signal and established critical precedent where there once was little.
Just last year, it reached its first settlement resolving claims of employment discrimination based on MOUD when it required a Tennessee county to make policy changes and pay damages to a correctional officer who was pushed out of his job because he used buprenorphine. The agency found that the Cumberland County Sheriff’s Office had violated the ADA by failing to make reasonable accommodations to allow him to work and use the medication.
Each time the Justice Department breaks new ground, Friedman said, it becomes easier for front-line attorneys to advocate for their clients in court. It also helps patients like Scott.
Like any good lawyer faced with a problem, Scott began to research. He learned his medication was federally protected, and then about a case remarkably similar to his own.
In March 2022, the Justice Department announced its findings that Indiana’s State Board of Nursing had violated the ADA by requiring that a nurse who was seeking to reinstate her license stop using buprenorphine in order to participate in a program that rehabilitates and monitors nurses with drug or alcohol addiction. The board’s abstinence-only policy violated the law, according to the Justice Department, in part by creating barriers that screened out people who used MOUD.
Indiana’s nursing board denied breaking the law, but agreed to pay damages and make policy revisions to ensure that nurses who use medication can remain on it while participating in a monitoring program.
Scott suddenly felt like he had “something to stand on.” He began to push back against TLAP.
‘Not fit to practice’
By the fall of 2022, Scott’s life had changed. He’d left his job at the law firm because he couldn’t get licensed, but got a new job negotiating contracts at a health care company. His first child, a boy, was born.
Scott had previously asked the Board of Law Examiners for more time as he tried to figure out how to comply with TLAP. He had decided he wanted to stay on buprenorphine, so he asked TLAP for permission to get a second opinion, this time from a Tennessee-based program, hoping a new evaluation would support his use of the medication. Though TLAP granted his request, by then Scott had grown increasingly frustrated with the process and traded a handful of contentious emails back and forth with the organization.
The board allowed him to postpone his final hearing to get the evaluation, but warned that failure to comply with TLAP would be grounds to deny him his license.
Scott paid $6,000 for the three-day evaluation, submitting again to drug tests, cognitive testing and extensive questioning about his criminal record and family history.
The results came a day before the hearing. When he read them, his heart sank.
The physician concluded Scott had used buprenorphine for more than a decade without any “legal, educational or occupational deficiencies or consequences,” and that his criminal history was “representative of living in poverty in a small community,” not of any underlying personality disorder.
Ultimately, however, he determined that Scott didn’t have a “foundation of recovery treatment” and was “not fit to practice law.” The physician diagnosed Scott with mild cannabis use disorder in “early remission,” as well as alcohol use disorder “by history.” Scott would later dispute both in writing to TLAP — he said he didn’t drink alcohol and was able to stop his occasional use of CBD and delta-8, the THC product, without issue.
Scott should follow Palmetto’s recommendation of attending abstinence-based treatment, the physician wrote, and also consider switching his medication to naltrexone.
Scott and his attorney had arguments on his criminal history prepared for his next hearing, but not the new evaluation. When they arrived at his hearing, they saw a representative from TLAP, which had also received a copy of the report. The stakes couldn’t have been higher. If the board denied his application because he hadn’t complied with TLAP, his bar score would expire before he could apply again.
He had one last option: withdraw and reapply as a first-time applicant, restarting the clock. He took it.
As he walked out of the room that day, he fought back tears.
‘I have a lot of work to do’
A year passed. By the fall of 2023, Scott was spending his days working from home beneath his unused law degree, vacillating between hope and frustration. By most standards, he was thriving. He’d been promoted, and his nearly 2-year-old son was enchanted with his new puppy.
But he hadn’t given up on his dream.
Scott reapplied for bar admission. At the end of November, he was called to a hearing that would determine, finally, whether or not he’d get to be a lawyer.
Scott received notice of the hearing on a Friday, just six days before it was scheduled. He contacted a new attorney, Greg Brown, who had years of experience representing professionals, including lawyers and doctors, before licensing boards. Brown spent that night reading through Scott’s file, and on Saturday morning, outraged over what was happening to him, officially took him on as a client.
Brown worked through the weekend, quickly drafting a legal strategy. He filed a response to the board stating that Scott would not comply with the requirement that he stop using his medication and attend abstinence-only treatment.
Four days later, Scott and Brown walked into a hearing room near the Capitol building in Nashville and sat at a white folding table facing four attorneys with the Board of Law Examiners. They expected to go head to head with TLAP and lose, and were prepared, Brown said, to file a federal civil rights claim afterward.
But no one from TLAP was at the hearing. Right away, according to the hearing transcript, the board made clear it didn’t want to discuss Scott’s medication or his noncompliance with TLAP at all. Though Scott had filed dozens of pages of supplemental material since the board first referred him to TLAP in 2021 — including court records, reference letters and detailed explanations of his legal record — the board wanted to focus its questioning on his past conduct. That included his criminal history, but also his communications with TLAP and the board, which had grown increasingly heated as time passed.
Scott’s past and his behavior during the licensure process were troubling, an attorney representing the board said at the hearing. “His conduct demonstrates that there is a lack of accountability for his actions and long history of conduct that gives rise to certain criminal arrests, and then an inability again to control his temper,” he said.
Scott testified on his own behalf, explaining his past criminal charges and apologizing for lashing out at TLAP.
The board highlighted one particular email that Scott sent to Buddy Stockwell, TLAP’s executive director, after he withdrew his application the year before. In it, he stated he was looking forward to working with the Justice Department to fix the character and fitness process in Tennessee. “It may be funny to you guys, but I’ve worked my ass off and I have a family to provide for. This isn’t over yet,” Scott wrote.
The board said it didn’t want to get into anything regarding the DOJ, according to the transcript. But it asked Scott to explain himself.
“I was very emotional,” Scott testified. “It hurt. I worked very hard to get here, and he had made requirements that I could not overcome.”
Brown began pressing the issue. The assessment Scott received before his last hearing, he pointed out to the board, “concluded that Mr. Scott was not fit to practice law because he’s on Suboxone treatment. That’s what it says.”
He asked if he could bring Scott’s doctor in to speak. “I don’t think that that is our focus,” a board member said. “That — the — any fitness issues or the particular treatment that he’s chosen to treat his addictions.”
Brown called Scott’s doctor anyway. For the first time, he testified before the board, saying he had no concerns about Scott’s fitness to practice law and that he had also treated other professional patients, including doctors and lawyers, with buprenorphine.
Other witnesses followed, offering glowing assessments of Scott’s character. After several hours of testimony, the board broke to deliberate. Scott steeled himself for bad news.
When they returned, the board announced Scott would get his license, without any conditions. Scott wouldn’t have to talk to TLAP again. It was over.
“I bet my eyes were big,” Scott recalled. “I was thinking, ‘This is unbelievable.’”
Before the hearing ended, a board member told Scott that the licensure process would have gone a lot easier if he had communicated better. Conflict, she advised, was an inevitable part of practicing law.
Scott nodded and thanked her. “I don’t plan to be back before any board ever again,” he said.
A month later, and nearly three years after he passed the bar exam, Scott stood in a courtroom in front of a judge and the Tennessee state flag with his right hand raised.
As his son watched him swear his oath of admission to the bar, he thought about the price he paid to get there. But he also thought of his grandmother Nellie and how proud she would have been to see it.
“Now, I have a lot of work to do,” he said. “It’s just the beginning.”
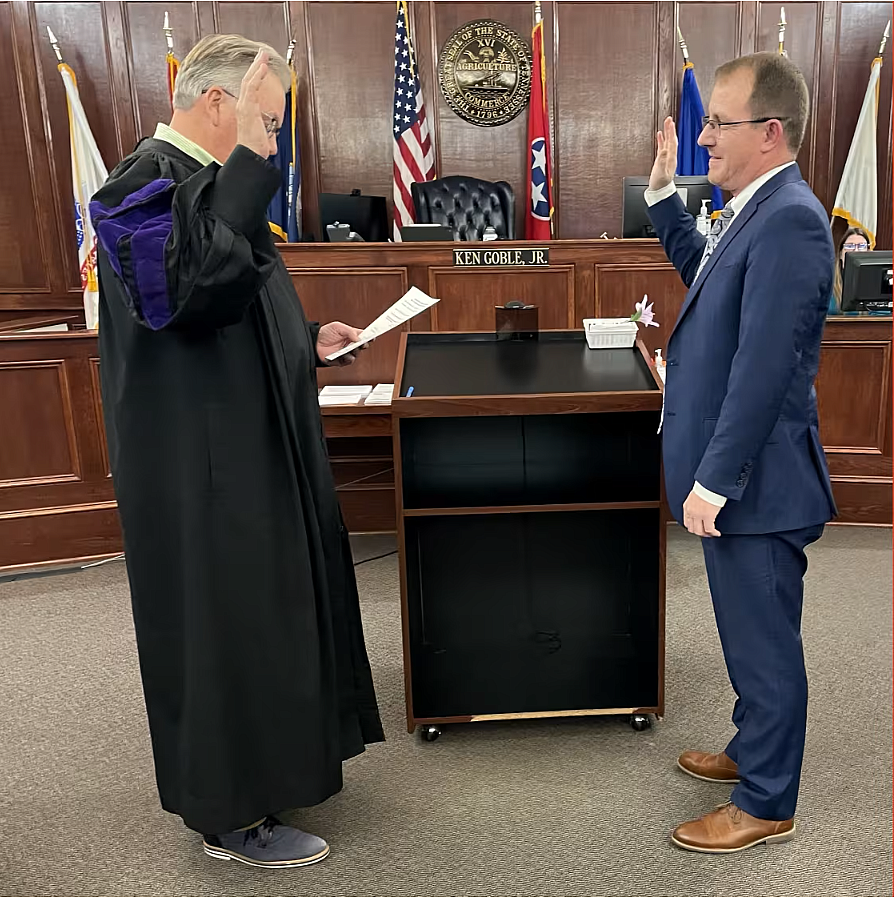
Derek Scott is sworn in to the bar in Tennessee.
Courtesy Derek Scott




