The pandemic's long shadow over the mental health of Minnesotans — especially youth
This project was originally published in Star Tribune with support from our 2022 Data Fellowship.
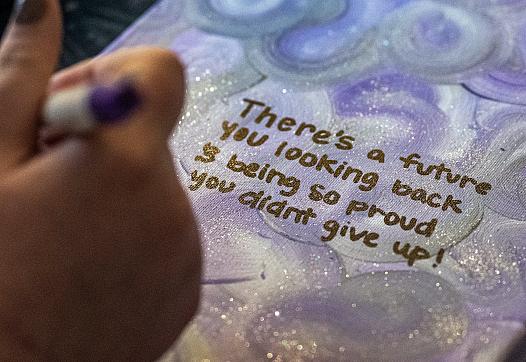
Image

Leinani Watson, 21, visited Minnehaha Falls in Minneapolis. Watson finds waterfalls soothe her anxiety.
Published on
July 28, 2023
The pandemic and social media were a toxic mix for Leinani Watson.
Throughout adolescence, Watson needed therapy and medications to treat mental health problems ranging from anxiety and depression to borderline personality disorder. Getting help was key to resisting self-harming impulses that sometimes sent her to the hospital.
But everything got worse with COVID-19. Watson was in the 2020 high school class that had graduation ceremonies online. Living in Spring Lake Park with her grandparents, she was particularly fearful about bringing the virus home. And as the isolation built, she sought connections on social media — the very platform where years earlier she learned techniques for harming herself.
Struggling to feel a connection with telehealth counselors, Watson delayed joining an online group therapy program. Once in-person sessions resumed and she joined, the group ultimately became a lifesaver.
"The pandemic really put a strain on my mental health," said Watson, now 21. "I still struggle, but for the most part I've found my will to live again. I realized that there is hope."
She's far from alone. The pandemic triggered widespread setbacks to mental health in Minnesota — particularly for kids, teenagers and young adults. Doctors say that while social distancing measures were crucial for limiting the physical damage from COVID-19, the mental health aftershocks continue.
This heightened demand for treatment is amplifying long-standing questions about whether Minnesota has enough mental health providers. Most rural counties are designated as shortage areas. Providers in the Twin Cities metro say they're struggling to hire enough staff and facing the difficult task of telling many patients — including youth — they'll have to wait to get the care they need.
Image

Leinani Watson is now happy with her mental health care. But she struggled to find the right program and provider.
Richard Tsong-Taatarii
Concerns are growing about burnout; caregivers are reducing hours or leaving the field entirely. And while telehealth has made it much easier for many patients to access mental health care — sometimes in just a day or two, and particularly across rural areas — broad adoption could be making it harder for providers to staff in-person treatment.
Patients with serious and persistent mental illness are having "a very difficult time finding a place to go" as the supply of such specialized care providers hasn't kept up with the growing need, said Steve Girardeau, a psychologist and legislative co-chair of the Minnesota Psychological Association. Long-standing access problems for kids and patients seeking a provider of color likely persisted or worsened during the pandemic, says William Robiner, a psychologist and researcher at the University of Minnesota.
Nearly 89% of the state's mental health workforce is white, compared with 78% of the population, according to the Health Department.
"The concept of 'shortages' is a slippery one — there isn't a statewide or even a regional number of providers that is 'right' or that would indicate that the market is in balance," said Teri Fritsma, the lead health care workforce analyst at the Minnesota Department of Health. "All that being said, for many years we have been aware of serious imbalances in the numbers of providers we need compared to the number we have."
'Huge' increase in needs
Insurers have seen increased demand for mental health services over the last several years driven by easier access through telehealth, reductions in stigma, growing awareness and a greater overall need among patients, says the Minnesota Council of Health Plans, a trade group for the state's non-profit health insurers.
This month, UnitedHealth Group — the Minnetonka-based health care giant that operates UnitedHealthcare, one of the nation's largest insurers — said it's seeing increases across the country, with the percentage of people accessing behavioral care over the last year growing by double-digits.
Minnesota health care providers say patients should keep seeking care, because they're employing new strategies in response to the demand, but they point to obvious signs of systemic stress.
This spring, nearly 7,000 children were on waiting lists for services across 21 nonprofit clinics surveyed by the Minnesota Association of Community Mental Health Providers.
PrairieCare says only six counties in Minnesota have pediatric psychiatric hospital beds, and staffing those beds has become even more challenging. Like the U.S., the state has a shortage of child and adolescent psychiatrists, said Todd Archbold, chief executive of the Brooklyn Park-based medical group.
Between January and April, pediatricians across nine clinics at Children's Minnesota made nearly 500 referrals for therapy — a significant increase, they say, over previous years.
Across all ages, referrals through mid-June to outpatient mental health from primary care clinics at M Health Fairview were up 15% over last year. The health system has launched services to help connect patients to outpatient therapies and programs that often have delayed appointments and start dates.
Among kids, Fairview has seen a huge increase in mental health needs, said Bobbi Jo Krieg, an outpatient therapist who works with pediatric patients at the health system.
"The world basically ran a giant experiment [during the pandemic] that would not be ethical to run — and we're seeing the outcomes of that," Krieg said. "You're seeing young people move through developmental milestones without the support they would have had. And you're also seeing teens who decreased their in-person socialization and increased social media consumption as a substitution — and there's plenty of studies out there to show that that increases anxiety and depression."
Even before COVID-19, more kids were coming to primary care with mental health issues, but the frequency and severity of problems since 2020 has intensified, said Dr. Eileen Crespo, president of the Minnesota chapter of the American Academy of Pediatrics.
Doctors are trying to provide kids in the clinic with stop-gap measures to help — suggesting mindfulness exercises, for example, when appropriate — because it can be such a long wait for therapy appointments, Crespo said. There's also a push at many clinics that pre-dates the pandemic to provide collaborative care, where mental health providers are embedded in primary care offices and offer near-term help with little or no waiting.
Pediatricians, she said, were not surprised by the U.S. surgeon general's report this May warning about the dangers of social media for youth mental health.
"We have just never had the volume of patients, who are all symptomatic at the same time, like we are seeing right now," said Crespo, who practices at Hennepin Healthcare in Minneapolis.
Waiting times vary
A Star Tribune survey of more than 20 mental health providers in June found that some therapists were offering appointments for adults within just a week or two. The waits at other providers were significantly longer — up to eight months at one health system.
It's difficult to generalize about wait times because they vary by age, severity of illness and services needed, but kids usually wait about seven times longer than adults because there are fewer providers with pediatric expertise, said Erin Pash, the chief executive at Mendota Heights-based Ellie Mental Health. Before the pandemic, the waiting list for mental health services at Minneapolis-based Washburn Center typically included fewer than 200 children, but it recently has had at least 500, said Craig Warren, the center's chief executive.
Options Family & Behavior Services announced this month it will close day treatment programs for both adults and teens because it's become too difficult to hire staff.
Wage requirements are rising much faster than insurance reimbursements, said Brian Sammon, chief executive at the Burnsville-based agency. And some therapists prefer the work-from-home flexibility with virtual visits, which leaves fewer staff for in-person work at his company's group therapy programs, Sammon said.
"We have people lined up out the door," he said. "We have a waiting list — and not enough staff to serve them."
During the pandemic, socialization decreased and isolation increased across the population, pushing most people down on a continuum that stretches from good mental health to severe mental illness, said Lew Zeidner, the vice president for mental health and addiction services at M Health Fairview. Meanwhile, a significant number of mental health caregivers reduced hours, stopped taking patients using health insurance or got out of the field altogether.
Image

Leinani Watson finds her jobs decorating cakes and working in a St. Anthony ice cream shop relaxing.
Richard Tsong-Taatarii
Mental health shortages
In Minnesota, the federal government says 70 of the state's 87 counties are mental health professional shortage areas. The designations consider several factors including the number of psychiatrists relative to the overall population or, in a few cases, the number of low-income residents in a county.
Counties in the Twin Cities metro and southeast Minnesota are not considered shortage areas, although the state says there are partial shortages in Anoka, Hennepin and Ramsey counties based on federal designations for certain census tracts.
Mental Health America, an advocacy group, reported this year that Minnesota ranked No. 23 among all states in workforce availability, a measure that includes psychiatrists, psychologists and other types of mental health professionals.
Increased wages and job vacancies point to wider shortages, said Fritsma of the state Health Department. While the licensed workforce has grown, state surveys suggest a greater share of mental health clinicians are being lost to other fields and non-patient care roles.
"I believe there are statewide shortages across the board in these professions," Fritsma said. "I think they've gotten worse during the pandemic. And I think they're worse still in rural areas."
As bottlenecks grow and health systems gyrate, patients suffer.
A national survey published by the Bowman Family Foundation this month documented a variety of problems for patients trying to use insurance benefits for mental health care. While health plans say they are expanding provider networks to meet the growing need, there's still not parity in access between mental and physical care, said Dr. Henry Harbin, a psychiatrist and former managed care executive who was senior author on the report.
"We have a pretty grim picture here," Harbin said. "Increased demand. Increased death rates. ... This is a system-wide problem. It's going to take a lot bigger set of actions — at multiple layers — to turn this around."
'Too depressed to even try'
Leinani Watson needed group therapy at the outset of the pandemic but couldn't find an in-person program. She tried coping without therapy, but she wound up hospitalized in June 2020 after harming herself.
Her sense of doom was pervasive. She was scared of getting sick, but she also wondered why she should keep living with all the deaths around her. Disconnected from others, she watched online videos where people broadcast how they used lockdowns for self-improvement.
"I felt guilty," she said. "While everyone online was posting their success, I sat in my dark room wondering why I couldn't be like them. ... I was just too depressed to even try."
In November 2021, Watson found help from in-person group therapy at Nystrom & Associates in Woodbury. Having completed the year-long program, Watson now feels she has turned a corner with the help of ongoing one-on-one sessions.
She enjoys her job decorating cakes and loves spending time in nature. In the coming year, Watson plans on returning to college to pursue a career in mental health. And as a biracial woman, she wants to share her story more broadly to help others search for the treatment they need.
"I am in a way better place than I was previously," Watson said. "Learning a lot of new skills through therapy is very helpful. And having somebody to talk to about what's going on in your life — and the person is not a person in your life — is also very helpful."