Part Two Sidebar: A work injury and a prescription. One Maine woman’s story of the cycle of addiction
This story was produced as part of a larger project for the USC Annenberg Center for Health Journalism's 2021 Data Fellowship.
Other stories in this project include:
‘Lucky to be alive right now’: Rumford man credits doctors, awareness, luck for avoiding addiction
At the root of an epidemic in Maine: a prescription pad
‘What we’re really dealing with is a trauma epidemic’: Multiple resources needed to address opioid crisis
The opioid epidemic is putting immense pressure on Maine’s child welfare and education systems
Methodology: Where the child welfare and education data came from
It was her own experience visiting her father in prison that made Nikole Powell want to make sure her children never see her there.
A hot, dirty, stuffy van. The doors clicking and locking. The guards all over the place. And then there was the time that she cracked her head on a rock while playing a game of tag with another boy there and walked out crying, blood pouring down her face all over the dress her father liked.
“It was super traumatic,” Powell, now 33, said recently from a conference room at the Southern Maine Women’s Reentry Center in Windham, where she’s serving her third prison sentence.
“I just didn’t want my kids to go through that stuff.”
Nikole Powell waits on March 16 in the hallway of the Southern Maine Women’s Re-entry Center to make a Zoom call to her son on March 16. Residents of the program are allowed five outfits of their own once they have made it through a 30 day period. Until that time they wear the prison garb, as shown on the two women walking on the right. Andree Kehn/Sun Journal
Powell grew up in Alaska with her father and four of the seven brothers on her dad’s side. When she was born, her father was already using heroin heavily, she said, a theme that would haunt her. A couple of years before she was born, her dad, a carpenter, broke his back when a large A-frame fell on him in a work accident. His doctors put him on fentanyl patches — a transdermal, extended-release form of the opioid pain medication — and soon after he went off them, he started using heroin.
“He was constantly gone. He would leave for weeks at a time and he would come back so strung out that we just didn’t even know who he was,” Powell said.
Powell’s father beat her and her brothers. She didn’t go to school much and, when she did, she blamed the bruises on her brothers. Her brothers terrorized her so much, Powell said, that to this day she is afraid of the dark.
Powell’s father was in and out of jail most of her life, but he didn’t go to prison until she was 12, she said. It followed an incident when six members of her father’s rival motorcycle gang kidnapped her as she was walking with some friends, and then brutally raped her.
She says she was in the hospital for a few months. Her father and some others from his gang went after the rival gang, killing at least one and putting a few in intensive care, sending her father to prison.
It was only then, to the best of Powell’s recollection, that Alaska’s Office of Children’s Services got involved, setting off a three-year search to find her mother who had gotten married, changed her name and moved to Rockland, Maine.
When Powell was 15, she made the move to be with her mom, stepdad, an older sister and a younger brother. They were practically strangers.
The transition was “pretty rough,” she said.
“It was really hard because I had a lot of resentment for my mom at that point in time because I didn’t know anything about her and I always thought to myself, ‘Well, I have this really shitty childhood and you were never around.’”
Powell said she did not like her new home at first. She wasn’t used to having rules, being told what to do or going to school. She would get into fights with her mom and take off. When she was 16, she dropped out of high school and got her GED on her own. When she was 17, her mom kicked her out of the house.
“I was just doing whatever I wanted and they weren’t having it. They didn’t know how to handle it,” Powell said.
She joined the Army, but returned to Rockland after basic training because she got pregnant with her first son, giving birth to him when she was 18. A year later, she married her first husband, her son’s father.
Nikole Powell chats with her best friend on March 16 in the computer lab of the Southern Maine Women’s Reentry Center. The two women have known each other since 2003 when they were both incarcerated. Powell supported her friend when her friend’s sister passed away from an overdose. Both women have been involved in an effort to expand the state’s Good Samaritan law to protect an individual who calls authorities to report an overdose. Andree Kehn/Sun Journal
SHADES OF HER FATHER: A BACK INJURY, AND A PRESCRIPTION
At first things were OK, Powell said. But when she was 19, Powell sustained a back injury while working construction. She went to her doctor at Waldoboro Family Medicine and after trying ibuprofen and Vicodin, which Powell said “really messed with my stomach,” her doctor switched her to taking up to two short-release oxycodone 30 milligram tablets twice a day.
It was 2008, years before Maine lawmakers clamped down on opioid pain medications through a bill strengthening the state’s prescription monitoring program. Under that 2016 law, Powell’s doctor would have been prohibited from prescribing her such a high daily dose — 180 morphine milligram equivalents — of opioid pain medications without a qualifying exemption such as cancer or palliative care.
After Powell finished the treatment course, “I was really, really sick,” she said. She recognized the signs from watching her father go through it — the shaking, flu-like symptoms, mood swings — she was in withdrawal.
Like him, Powell developed an opioid use disorder being prescribed painkillers for a work injury. Unlike him, she didn’t need to look beyond her doctor’s office for her supply.
When she realized she was going through withdrawal, Powell recalls saying to herself, “Oh, man, I’m not doing this.”
For the next two years, she returned to her doctor, making up excuses for why she needed the oxys.
“And my doctor just kept giving them to me,” Powell said.
Dr. Paul Vinsel practices addiction medicine at Tri-County Mental Health Services and Central Maine Medical Center in Lewiston. When a person becomes dependent on a drug like an opioid, “their reward center is set so low that they don’t get the same pleasure out of the normal things that we get pleasure out of,” he said. Andree Kehn/Sun Journal
HOW OPIOIDS TRANSFORM THE BRAIN
Substance use disorder is a disease much like any other chronic illness.
Dr. Paul Vinsel, an addiction medicine physician at Tri-County Mental Health Services and Central Maine Medical Center in Lewiston, likens it to diabetes.
With both diseases, something has disrupted a person’s normal functioning. For type 2 diabetes, it could be poor eating habits and little exercise, or with type 1, the genetics a person is born with, that affects how the body processes blood sugar.
Substance use disorder develops out of a person’s dependence on a substance, like an opioid, to the point where it interferes with their ability to function normally.
When the brain is exposed to an opioid, regardless if it’s in the form of a pill that came from the doctor’s office or a balloon of heroin from the streets, it stimulates opioid receptors in the body’s nervous system.
It decreases pain, slows the body down and, with increasing doses, decreases breathing, Vinsel said. Most people tend to have two different reactions to opioids: For some, even though their pain may decrease, they feel ill; others get that “high” feeling.
Nikole Powell checks her commisarry balance on March 16 at a kiosk in the Southern Maine Women’s Re-entry Center. Andree Kehn/Sun Journal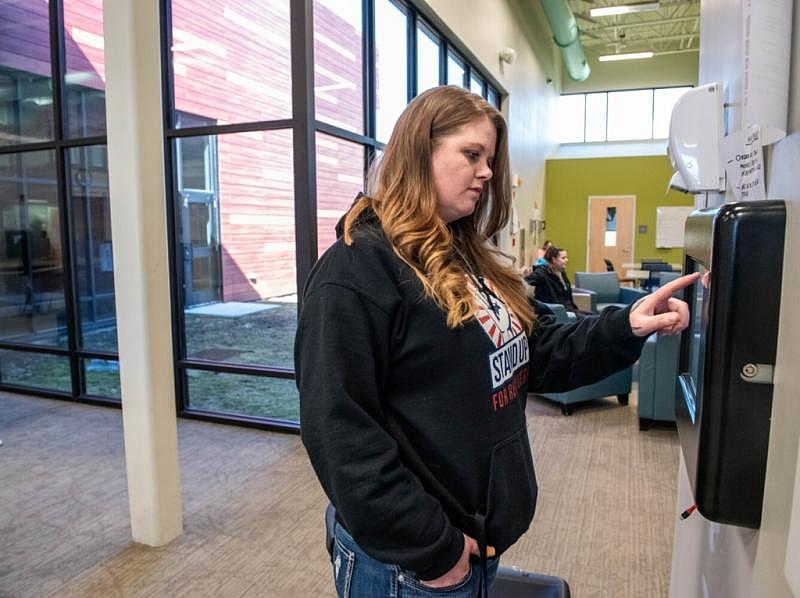
Over time, with sustained or growing exposure to opioids, the amount of stimulation the opioid receptors — the body’s reward center — get from the drug decreases.
It “transforms the reward system in your brain,” Vinsel said. The brain needs more of the drug to get to just a baseline feeling of normal, and without it, the body has a physical reaction — withdrawal — and causes cravings for the drug.
Meanwhile, the typical things that stimulate the reward center and make people feel good — “good food, going out in the beautiful weather, sex,” Vinsel said — no longer stimulate the reward center as much as the drugs do.
A person needs higher highs just to feel normal, and the lows without the drug get lower.
When a person becomes dependent on a drug like an opioid, “their reward center is set so low that they don’t get the same pleasure out of the normal things that we get pleasure out of,” he said.
Still, even with the risk that opioids can shift the brain’s reward system, there are people with chronic pain who can reasonably use opioids with a doctor’s supervision while maintaining a normal life.
It’s when the dependence spills over into a person’s social life — having trouble at work or maintaining relationships, giving up hobbies that they enjoyed or using much of their time in pursuit of that drug — that a dependence becomes an addiction, a medical diagnosis more commonly referred to now as substance use disorder, Vinsel said.
Nikole Powell checks her email on March 16 in her room at Southern Maine Women’s Reentry Center in Windham. Residents in the program are allowed email and limited internet access for education. Powell also has permission to work on legislative work. Andree Kehn/Sun Journal
DRUGS AS A COPING MECHANISM
Over the next decade, Powell struggled with substance use disorder. At first it was the oxys, but when she was 21, her doctor was fired for his prescribing practices. When her new doctor cut her off cold, she started to buy oxys from other people and then began to drink excessively.
“I think he was just too scared to lose the practice to continue letting people just get whatever they wanted,” Powell said. “He lost a lot of clients at that point in time because they were switching to a different doctor that was going to give them what they wanted.”
The first time Powell went to prison it was for 10 months on a charge of domestic assault against her second husband. She was 23. Her three boys, who are now 11, 12 and 14 years old, were all younger than 4.
Powell said she missed her kids, but she didn’t want them to go through the same experiences she did as a child. To cope, she started using drugs — heroin, crack, oxy — whatever people had on them when they got in “and you would just make it last for as long as you can.”
At the time, it was easy to slip drugs into the Maine Correctional Women’s Center, she said.
During her second prison stint, on another domestic violence conviction, she was in the “pods,” which she described as a secluded section for residents who break prison rules, for 10 out of the 12 months she was there.
After she was released, Powell said she didn’t drink or use any drugs except marijuana for four years. In February 2019, she and an acquaintance were driving back from New Hampshire and stopped at the Kennebunk rest area.
Nikole Powell stands in front of the Southern Maine Women’s Reentry Center garden on March 16. Powell worked at an organic farm when she was not incarcerated and enjoys the work. Powell says her favorite garden activity is weeding. Andree Kehn/Sun Journal
Unbeknownst to Powell, while she was inside, the acquaintance slipped methamphetamine into the joint he was rolling.
Next thing she remembers, she woke up in a booking room at the Knox County Jail. The man she was with admitted on a recorded phone call after she posted bail that he fed her meth, crack, heroin and ecstasy all in one night, and that he had planted drugs on her.
After four years without doing these kinds of drugs, Powell said she had no tolerance for the amount that was in her system. Recordings from the booking room where Powell was detained that were reviewed by her attorney show that she kept passing out and begging the corrections officers to take her to the hospital, according to Powell. The Sun Journal has not independently verified these videos.
She was not taken to the hospital.
After six days in jail, Powell bailed out. She thought she was doing OK but “with meth, and I didn’t even ever in the years that I had used oxys, never have I wanted a drug as bad as I wanted to do meth again.”
Powell said she started to use meth and other drugs, like heroin, heavily. She was living in Mexico, in Oxford County, at the time and also began to sell the drug — multiple pounds a week.
Her kids were with their fathers, “so once again, I was like ‘Well, my kids aren’t with me so this is all OK.’ And I was just justifying it and I started to notice that more and more, I wasn’t going to see my kids as much as I should have been.”
In September 2020, she was sentenced to seven years in prison, with all but four suspended, on charges of drug trafficking, drug possession and violation of bail conditions from an arrest unrelated to the February 2019 incident, as well as on charges from that February incident.
She moved from the women’s center at the Maine Correctional Center to the women’s reentry center down the hill in May 2021.
Unlike the past two times she was incarcerated, Powell said she found a drug-free environment in the reentry center. She also attends Narcotics Anonymous meetings and lives in a medication-assisted treatment-free section so there are no drugs of any kind around.
Last fall, she helped a friend move sections and injured her back so badly that she had to go to the medical unit at the main prison. Instead of a script for a high-dose opioid painkiller, clinicians there gave her cortisone injections, a type of steroid used to treat swelling. Despite pain so bad that Powell said she had to use a walker to get around, she wasn’t going to take a controlled substance.
She’s taking classes through Washington County Community College, she’s involved in a number of peer support groups, she’s a member of the Maine Recovery Advocacy Project and she works six days a week at Clynk in South Portland through a work release program.
“I have a really strong support network now,” Powell said.
She’s doing her best to parent her kids from prison and it’s been far from easy, she said.
But unlike the last time she was in prison, when she used drugs as a coping mechanism, “I think that using is the last thing on my mind right now,” Powell said.
The project was produced in partnership with the USC Annenberg Center for Health Journalism through its 2021 Data Fellowship program.
[This article was originally published by Sun Journal.]

