San Antonio’s wealthy, healthy areas have more hospitals and clinics — and there’s little motivation to change that
This story was produced as part of a larger project for USC Annenberg Center for Health Journalism’s 2021 National Fellowship.
Other stories in Laura Garcia's series include:
A broken system got worse: How COVID ravaged San Antonio’s South Side
Ayala: The health care system isn’t broken, it’s working as designed
Join us for a free San Antonio community health fair on May 28
Access Denied: How we analyzed the data
University Health makes plans to build two new hospitals
ACCESS DENIED: Our medical system is a maze, so patients need navigators — people like Maria Lee

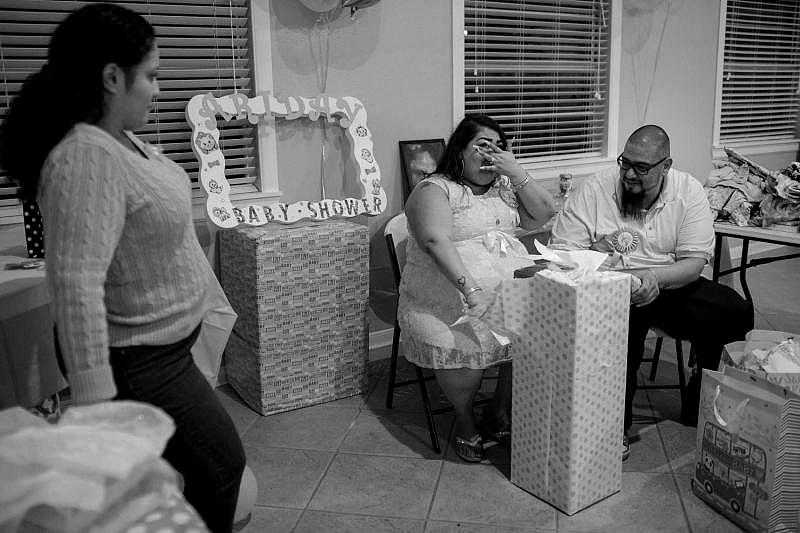
Josie Norris / San Antonio Express-News
Not long after Dr. Lyssa Ochoa moved to San Antonio to practice medicine, she set a goal of opening a clinic on the South Side, where people are generally sicker and medical facilities much scarcer than elsewhere in the city.
And that’s what she did, leaving a stable job at a large medical practice to fight health disparities on her own terms.
In 2018, she founded the San Antonio Vascular and Endovascular Clinic (SAVE) on the city’s Southeast Side, providing outpatient care for patients with circulatory problems who needed urgent treatment to avoid amputations. She opened an office on the Southwest Side and in the South Texas towns of Floresville and Pleasanton.
A year later, her business partner Carl Negley, a health care consultant, found a piece of land in the middle of the South Side. He proposed building an ambulatory surgery center there to perform same-day and outpatient procedures. He also proposed that they get married. She said yes.


As for Ochoa’s choice of location, her peers told her she was making a huge mistake and that the South Side was the “wrong place.” They said she should have located in Stone Oak on the North Side, where she could earn more.
Undeterred, she moved her staff into her new headquarters at 603 E. Amber St., and opened Mission Surgery Center, where general surgeons can perform outpatient procedures in urology, orthopedics and plastic surgery.
It’s the only such surgery center south of downtown, and Negley said it’s applied for federal certification to accept Medicare and Medicaid patients.
Since then, Ochoa has opened four more SAVE clinics throughout the city. Several times a week, SAVE staff members pack their medical equipment into a van and drive to meet patients at the clinics closest to them.
Location matters
Medical facilities in San Antonio are heavily concentrated in the northern parts of the city, placed in areas where patients generally are healthier and more affluent and where providers can collect higher reimbursements from insurance companies.
Meanwhile, in the southern part of the city, options for hospitals, medical specialists and surgical centers are limited. Those in the industry say there’s little motivation to change that.
The Express-News mapped the nearly 50 emergency care facilities in the area, including full-service trauma hospitals and freestanding emergency centers, and found that the majority of ERs are on the North Side.
Many are in the South Texas Medical Center on the Northwest Side. But residents in other high-income areas such as Alamo Heights, Stone Oak and Shavano Park also enjoy greater access to emergency care.
For every eight emergency rooms in these wealthy parts of the city, the South Side has one.
ER care is nonexistent on the East Side, which has no hospitals, unless one considers the San Antonio Military Medical Center, which accepts civilians only in cases of severe trauma, mass casualties or specialized burn care.
Obstetrics is another area of inequitable access. Expectant mothers on San Antonio’s South, West and East Sides have few options. During the 10 years before September 2021, there was only one hospital delivering babies on the South Side. Families on the Southeast Side and in rural communities south of Bexar County had to drive 8 to 25 miles from home to find a hospital with basic maternity, labor and delivery services.
Currently, there two major hospitals in the southermost third of the city.
Texas Vista Medical Center — a 327-bed facility at 7400 Barlite Blvd. (formerly Southwest General Hospital) — has operated for nearly 40 years. It’s owned by Steward Health Care of Dallas.

And there’s Mission Trail Baptist Hospital in the Brooks mixed-use community on the site of the former Brooks AFB. It is one of five Baptist Health System hospitals in Bexar County owned by Dallas-based Tenet Healthcare.
People in the northern areas of the city have no shortage of state-of-the-art health care facilities nearby.
The rapidly growing Alamo Ranch area, along State Highway 151 west of Loop 1604, has attracted a flurry of hospital construction by the Christus Santa Rosa Health System, Baptist Health System and Methodist Healthcare System. The U.S. Department of Veterans Affair built a massive outpatient clinic in Westover Hills.
A little farther north on Loop 1604 between Culebra and Bandera roads, University Health, Bexar County’s public hospital system, bought land for a hospital. Nearby, a UT Health San Antonio training facility-sports clinic is being built for student-athletes at the University of Texas at San Antonio.
University Health has acquired an additional 42.5 acres of land zoned for hospital development in Selma, near the Retama Park racetrack on the far Northeast Side.
In September, George Hernandez, University Health’s president and CEO, announced plans to build a hospital on a 68-acre tract across from Texas A&M University-San Antonio’s campus on the Southwest Side.
Hernandez, who grew up on the South Side near Burbank High School, rebuffs criticism that the system took too long to buy land or build in that part of the county. He said it was waiting for the right spot to become available.
“I don’t think there’s another public health system in Texas that has as many clinics as we do,” he said.
University Health has six of its own primary care clinics on the West and South sides and one on the East Side. They also partner with CentroMed, a nonprofit that operates eight of its 25 sites on the South Side, and with CommuniCare, which has two clinics on the West Side.
“Why build bricks and mortar when you have partners like that,” Hernandez said. “You have to look at what’s the best way to get the care out quickly. Sometimes, it’s building. Sometimes, it’s partnering.”
To be sure, multiple organizations operate free and low-cost medical clinics throughout underserved areas, such as Methodist Healthcare Ministries' two Wesley clinics. But they don't address disparate access to higher-level care, including various specialties and emergency medicine for life-threatening conditions.
Ochoa, who has surgical privileges at the two hospitals on the South Side, said it's not nearly enough.
Mission Trail opened in 2011, replacing Southeast Baptist Hospital. With 110 beds, it is the smallest full-service hospital in the Baptist system. The combined 437 beds at Mission Trail and Texas Vista Medical Center pale in comparison with the more than 5,100 beds available on the North Side.
Ochoa and Negley say city leaders need to step up, perhaps by offering incentives to health care organizations to build on the South Side.
“It’s much harder for a small business to say, ‘I’m going to go down there and take the risk and maybe the business isn’t successful.’ But that’s not true for big hospital chains. They are making billions of dollars,” said Negley. “The hospitals are making profits and consciously deciding that the profits aren’t enough to reinvest in the community.”
Ochoa cited the rapid population growth on the Southeast Side and questioned why Baptist Mission Trail Hospital isn’t growing along with it.
“I think from a social responsibility standpoint, these big businesses should be accountable to the community that they are serving. If they’re too small, then they need to expand and provide the services needed,” she said.
Baptist officials did not respond to requests for comment.
Baptist operates two smaller “neighborhood” hospitals in the area, one near Port San Antonio and another on South Zarzamora near Interstate 35. But those facilities are freestanding emergency centers rather than full-service hospitals.
Unlike privately owned, for-profit ERs popping up across the city, which focus on concierge health services, Baptist’s ERs can accept Medicare patients and those covered under Tricare, a government-sponsored health insurance program for active and retired service members and their dependents.
Some doctors say “micro-hospitals” can drive up costs for consumers who aren’t aware that urgent care facilities provide many of the same services at much lower rates.
Lives and limbs
A grim way to measure health disparities is by life expectancy.
The average number of years a person may live varies by up to 18 years across San Antonio, depending on what neighborhood you live in. Life expectancy is strongly influenced by so-called social determinants of health, such as access to healthy food, recreation, living wages and medical care.
For example, it’s harder for someone living in a neighborhood with a high crime rate, few street lights and no sidewalks to get adequate exercise and remain fit. It’s harder still if the person works multiple jobs, or if they can’t afford a health club membership — or if they can but have no way to get to its gym.
In contrast, it’s easier for a person who lives near a park or walking trail and who works 40 hours a week at decent pay to stay active and avoid chronic health conditions.
Residents in census tracts on the South Side can expect to live into their early 70s on average, according to data from the Centers for Disease Control and Prevention. For people in certain census tracts on the North Side, life expectancy is 84 to 88 years on average.
The average life expectancy for all of Texas is 78.6.
Another chilling measure of health disparities is loss of limbs to diabetes. The most recent data available, from 2015, shows that ZIP codes on the South, West and East sides had the state’s highest rates of hospital admissions for amputations of lower extremities.
Such amputations are often a last-ditch effort by a surgeon to save a patient’s life after an infection or uncontrolled diabetes blocked blood vessels.
“It’s completely preventable,” Ochoa said. “There’s so many stages that it’s preventable and controllable.”
As a vascular surgeon, Ochoa treats patients’ veins and arteries and tries to make sure they are clear enough so that oxygenated blood can flow to every part of the body.

On the West Side at the Texas Diabetes Institute, there’s another surgeon working to save lives among the disenfranchised.
Dr. Thomas Zgonis is a podiatry specialist whose work is protecting infected toes and legs from amputation. When surgery is necessary to save a patient’s life, he helps them recover and regain mobility.
Zgonis is eyeing University Health’s recent land acquisition on the Southwest Side as a future site for a new clinic that could focus on prevention and help patients avoid amputation.
Diabetes is a true epidemic, he said, especially in parts of the West and South sides, where up to a quarter of the adult population shares this diagnosis.
Salvador Martinez, a 63-year-old West Side resident, was on his way to a job interview when he tripped on an uneven sidewalk. He fractured his shinbone and contracted a severe infection. A month later, doctors surgically removed his left leg below the knee.

“It was a freak accident. I didn’t even know I was diabetic,” he said. “I’ll be honest. Those first couple of weeks” after losing the leg “I went through some dark moments in my life.”
After the surgery, he waited three years for a prosthetic limb because of the cost and problems with insurance.
In March 2021, Martinez contracted another infection, and Zgonis had to remove part of his remaining foot.
But during a checkup last fall, Martinez said he was thankful to be able to stand again and hoped to be well enough to go watch his favorite national team, Mexico, play in the World Cup someday.
Another patient, Ray Anthony Alcaraz, knew that he had diabetes but didn’t realize how much it mattered where he went to get medical care.

The day after Thanksgiving in 2020, he ended up in a local hospital with an ulcer on the bottom of his foot. One doctor told him he would lose both legs, but he remembers another doctor fought to save one of them.
“When I was getting discharged, she told me, ‘I don’t want to see you here at this hospital. Where you need to go is University (Hospital), but don’t tell them I told you that,’” he said.
Later, he was able to get on CareLink, a financial assistance program through University Health, and made an appointment at the Texas Diabetes Institute.
Zgonis was able to do another surgery so that his remaining leg would heal properly. It worked.
Because he is uninsured and now can’t work, Alcaraz waited over a year for a prosthetic leg to help him walk again.
Change in priorities
Linda Hook has been a public health nurse in San Antonio for nearly three decades.
She started her career in the Metropolitan Health District’s public health nursing department. Ultimately, she became director of the department. In 2008, she started teaching nursing students at the University of the Incarnate Word.
“This is the most segregated city for health in the world. I shouldn’t say that out loud, but it really is,” she said.
Linda Hook - a longtime University of Incarnate Word professor and public health nurse who has helped organize numerous vaccine clinics in San Antonio - calls San Antonio "the most segregated city for health in the world." Josie Norris / San Antonio Express-News
She runs UIW’s free wellness clinics in underserved communities on the South and East sides.
Hook says medical care is not equitably distributed across the city, but she hesitates to describe it as the result of disinvestment.
“I would say it was a change in priorities,” she said, interviewed at a clinic in a church building on the East Side. “San Antonio struggles because the money is short.”
At one time, the city’s public health department operated more than 30 clinics and paid nurses to make home visits. But in the 1990s, federal legislation limited reimbursements for direct care, forcing such programs to rely on grants.
There was also mounting pressure for Metro Health to provide other public health services, such as animal control and restaurant inspections, which meant less money for medical care.
Now, two years into the COVID-19 pandemic, Metro Health must brace for change.
Bexar County announced plans in late April to create its own public health division — separate from Metro Health — using $60 million in federal American Rescue Plan Act funds.
County Judge Nelson Wolff said residents outside the city limits were left behind during the COVID-19 pandemic.
County Manager David Smith’s presentation on the need for a county health division cited the first article in this series, which showed that COVID-19 death rates were up to 16 times higher in parts of the South Side compared with parts of the North Side.
At least 5,320 Bexar County residents have died because of COVID-19. Many of them were at greater risk because they suffered from conditions that can be prevented or controlled, such as diabetes and obesity.
“We’re trying to help people before they get really sick,” Wolff said. “They might not have lost their lives had they not had one of those underlying conditions.”
Dark history, troubling present
On April 6, 1968, when the HemisFair World’s Fair opened in San Antonio, local leaders touted the city as a gleaming city of the future in an effort to boost tourism.
Texas Gov. John Connally alluded to the new Tower of the Americas and its rotating restaurant in the sky when he said the world’s fair had “turned the downtown area from slum to jewel box.”
A CBS News film crew captured a different side of life in San Antonio: the squalid living conditions and extreme poverty of Mexican-Americans on the West Side.
The documentary “Hunger in America” included scenes of a malnourished baby crying and of a crowded ER waiting room at Robert B. Green Hospital downtown, predecessor of University Hospital.
Then-County Commissioner A.J. Plouch told the filmmakers that there will always be hunger because of fathers who refuse to work: “Some men aren’t worth a dime.” He also said that impoverished children didn’t need to go to school beyond eighth grade.
Plouch later tried, unsuccessfully, to keep the coverage off the air in San Antonio, according to a Texas Public Radio report on the documentary’s 50 year anniversary.
Such callous disregard for San Antonio’s neglected neighborhoods goes back decades before “Hunger in America.”
Beginning after the Great Depression, federal officials discouraged home mortgage lending in lower-income areas across the country, a practice known as redlining that made it harder for Latinos and Blacks to purchase and improve homes and build wealth the way white Americans could.
Public health experts say the effects of redlining and other forms of economic discrimination are long-lasting and contribute to uneven access to healthcare.
“It has been part of the foundation on which we built this city,” Mayor Ron Nirenberg said.
In August 2020, six months into the pandemic, the city council adopted a resolution that declared racism a public health crisis and committed the city to promoting health equity.
Accompanying the resolution was a report that compared white residents of Bexar County with Blacks and Latinos.
Twice as many Latinos live in poverty as do whites, and more than a quarter of Latino adults don’t have a high school diploma, compared with less than 5 percent of whites, the report said.

Nearly 20 percent of Latinos were uninsured — twice the percentage of whites — and 24 percent of Latinos said they had delayed medical care within the past year for financial reasons, compared with 10 percent of whites, according to the report.
Nirenberg expressed hope that local leaders will use the influx of federal pandemic recovery dollars to focus on overlooked areas of the city.
Julian Castro, former U.S. Secretary of Housing and Urban Development and former mayor of San Antonio, endorsed that idea. He said the money should be used to lift up parts of the South, West and East sides by improving infrastructure, schools and housing.
“People are tied with one arm behind their back when it comes to getting ahead,” Castro said. “It makes a difference whether you’re born in a poor neighborhood in San Antonio or a more affluent one.”
May 28 Event
Building on Express-News Reporter Laura Garcia's in-depth series on health care disparities in San Antonio, she will engage a panel of experts in a frank discussion about such inequities on the South Side, as well as solutions. It's part of a free community engagement event in partnership with HealthTexas Primary Care Doctors, Methodist Healthcare Ministries of South Texas, Inc. and the USC Annenberg Center for Health Journalism. Various health care resources and medical screenings will be available. COVID-19 vaccines will be administered courtesy of Lela Pharmacy and DisabilitySA.
When: 9 a.m. to 1 p.m. Saturday, May 28
Where: Wesley Health and Wellness Center, 1406 Fitch St., San Antonio, TX 78211
Laura Garcia reported on health disparities as a USC Annenberg Center for Health Journalism 2021 National Fellow and a grantee of its Dennis A. Hunt Fund for Health Journalism. Data reporter Libby Seline contributed to this article. Assistant city editor Tony Quesada edited the series.
laura.garcia@express-news.net

[This story was originally published by San Antonio Express-News.]

