If anyone knows how mental illness can land someone in the criminal justice system, it’s Dianna Branch.
Branch, of Anderson, is the mother of a severely mentally ill adult son. She says his illness — and the drug use he believes eases his symptoms — has caused him to start fights with family, total seven cars and vandalize property.
“I don’t know how he hasn’t killed himself or somebody else,” she said.
While Branch can detail the exact steps her son normally goes through — crime, arrest, release a short time later — the one part of the process that continues to mystify her is how to get her son out of trouble for good. He has yet to be deemed gravely disabled by the court or even assigned a treatment plan that stops his cycle of hallucinations, drug use, and arrests.
“I mean, I know he’s going to die from it,” Branch said.
She is not alone in her struggle .
Local mental health experts say untreated severe mental illness is the root cause of some large portion of the North State’s substance abuse and crime problems. Yet the system is set up in such a way that, instead of getting treatment, many simply cycle in and out of jail. Advocates and officials point to a lack of resources coupled with a flawed and complex system of state and federal laws that make it too hard to get people into treatment.
“Because it’s not right this second ... if you’re not slitting your wrists or already killed somebody (you won’t get help),” Branch said. “It’s been going on 20 years that he’s proven a danger to himself. You can’t even believe the stuff he’s done to himself. Yet they say he’s not a danger because he’s not trying to kill himself right then?”
The Record Searchlight’s findings from a months-long analysis of the relationship between crime and mental illness in Shasta County show the extent to which the system is broken, and how its shortcomings contribute to a cycle of crime and violence that degrades everyone’s quality of life. Those findings include:
— Today, over 50 percent more inmates at the Shasta County Jail require medication for mental illnesses than in 2008.
— Local officials remain unable even to take the first step of quantifying how many people in the area are mentally ill and how many in the criminal justice system are there because of a crime related to their illness. Still, these officials unanimously acknowledge there’s a link that needs fixing. That means there are no specific reference points to begin to solve the problem. No one can put a price tag on what they still acknowledge is a costly and inefficient process of filtering mentally ill people through the criminal justice system.
— Many of the new programs that do exist to stop mentally ill offenders from committing new crimes are funded with little or nothing, serve relatively few people and are voluntary, meaning those who don’t want help won’t get it.
In the meantime, people like Branch’s son continue to self-medicate with drugs, which generally cause them to avoid the rehabilitation needed to get sober and receive psychiatric care. The Record Searchlight is not naming Branch’s son because he could not be reached for comment in this story.
“What we need are some legal tools that would help us better manage people and require people who have serious addictions to be treated,” said Donnell Ewert, director of Shasta County Health and Human Services Agency. “We’re not able to force people to get the treatment they need.”
But experts and stakeholders say there are more significant measures available to at least ease the system, if not outright change it — and some of them are already taking off, including Laura’s Law, which the county recently passed. It mandates court-ordered treatment for some who have repeated episodes.
“Our system is broken,” Branch said. “It’s not helping people. And it isn’t going to change unless we get it changed.”
‘ALLOWED TO BE MENTALLY ILL’
As obvious as it may seem that someone needs psychiatric treatment, the legal definition of “need” is a careful balancing act with individual liberty.
“You can’t just say, ‘You’re mentally ill, we’re going to take away your rights,’” Ewert said. “They’re allowed to be mentally ill.”
With the civil rights movement flourishing when it was created in the 1960s, California’s Lanterman-Petris-Short Act only lets officials detain people for mental health holds when they’re about to hurt themselves or someone else. Even if they’re obviously unwell, Ewert said, that’s not enough.
“I think the general public has a misunderstanding of what we do,” Ewert said. “If (potential patients) say they’re living in a tent because they’re waiting for aliens to pick them up and won’t eat till they pick them up, then maybe we can (mandate treatment). We’re a nation of laws … which is a good thing.”
The key in that example is the person won’t eat — endangering his own life. But when an officer, deputy or medical or mental health professional encounters a man waiting for those aliens in a tent but otherwise taking care of himself and letting others be, that person has to seek treatment on his own.
“We only can help the most severely mentally ill,” Ewert said. “We can offer help to the others, but they don’t necessarily take us up on it.”
Of those who are put under a 5150 hold, as the 72-hour detainments are called, 60 percent to 65 percent are assessed and released for not meeting the criteria, said Dean True, director of the county’s adult services division, which includes mental health. True said that’s not to say they’re being turned away, though — it could be that their psychosis was determined to be drug-induced, they were in a crisis that resolved itself, or something else.
The 35 percent or so who do meet the full criteria for a 72-hour hold are then found a bed in a psychiatric facility, True said.
Funding that was earmarked in the 1960s for more holistic programs to treat mental illness never materialized, and surveys not long after the act became law showed huge swells in homelessness and incarceration. It was an unfortunate byproduct of the “deinstitutionalization” model, since some people who don’t meet the criteria for a mental health hold are still too out of touch with reality to seek treatment, hold jobs or function successfully in society.
“That’s the really frustrating aspect of mental illness, is many times it comes with lack of insight,” Ewert said. “Generally, if you’re in severe (physical) pain, you’re going to tell somebody, whereas somebody with mental illness, everything’s making sense to you in the sense that you think, ‘Well, these are real things.’… And so that lack of insight makes it really hard to help that person, because they’re not seeking help on their own.”
When drugs are involved, the person may end up going to jail for their drug use or behavior while intoxicated instead of getting help. But on the flip side, someone whose symptoms are largely drug-induced may be admitted to a psychiatric facility if incorrectly diagnosed, making for a complicated system, True said.
“You aren’t going to make a person better by sending them to a mental hospital when their psychosis is drug-induced,” Ewert said.
Indeed, True said family members often think their loved one is having a mental episode when it’s actually drug-induced, and the patient is quickly released from the facility because it’s not the right type of treatment.
“We are called upon to make those differentiations on a regular basis, and there are family members in the community, absolutely, who disagree with our clinical findings,” he said. “They do get hospitalized, even though primarily it was a drug-induced psychosis. That will happen on occasion, because you don’t know. I mean, ultimately, you don’t know. We won’t know for a few days, perhaps, what’s underlying this.”
To get to an inpatient psychiatric facility, a person first needs to be medically cleared, which usually happens in an emergency room, True said. If the person seems to be under the influence of drugs or alcohol, True said mental health employees tell hospital staff to contact them whenever the patient is sober enough to be properly assessed.
Branch said what usually happens with her son is he’ll calm down enough by the time a mental health worker shows up to assess him that he’s no longer considered a danger. He may use drugs, she said, but he’s been diagnosed with bipolar schizoaffective disorder and needs treatment for it so that he’ll stop using those substances, not the other way around.
“Why does he have to go through this? It’s because they say he has a right to,” she said. “Well, why doesn’t he have a right to have a sane mind?”
Since not long after its enactment, some California lawmakers have sought reform in the 1960s act that created the definition of those rights, with one of its namesake creators, Frank Lanterman, reportedly expressing remorse over how the law had inadvertently prevented people from getting treatment when its intent was to help them.
A reform task force published a report in 2012 finding that the law’s mandates need to be updated to get more severely mentally ill people into treatment they don’t think they need.
But the recommendations have gone unheeded, with many remaining concerned about the legal implications of doing so.
“I just tell everybody I can,” Branch said. “We need to change the laws.”
LAW ENFORCEMENT’S ROLE
Alarmed by a series of suicidal letters her father reportedly sent her, a woman called local authorities in September for a welfare check at his Happy Valley home.
Shasta County sheriff’s deputies got to Tim Kyle Torngren’s house and — about an hour later — he was dead from their gunshots.
Deputies have said Torngren came outside armed with a gun, and scanner reports also indicated he had pointed it in the air. But it will probably never be known whether Torngren was hoping the deputies would shoot him — “suicide-by-cop,” as it’s called — or had something else in mind that day.
Those kind of interactions with law enforcement are not extremely rare for mentally ill people in crisis.
A Washington Post investigation found that police shot and killed 124 mentally ill people in the first six months of this year, making up about a quarter of the total 462 people shot to death by police in that time.
Much of the problem, advocates say, is that not enough officers are educated on how to de-escalate crisis situations, including in California, where they aren’t required to receive ongoing training for such situations and their initial training on it can be as little as six hours.
Those six hours — out of a total 664 hours required before getting a job as an officer in California — also focus on handling people with disabilities in general, including physical and developmental along with mental illnesses, according to the Peace Officer Standards and Training division of California.
“It’s astounding,” state Sen. Jim Beall, who represents the 15th district in the San Jose area, said of the meager requirement for mental-health training. “It should be more important than marching.”
That’s why Beall authored Senate Bills 11 and 29, which Gov. Jerry Brown passed last month and will require officers to get more training on mental health crises starting in 2016. Among the changes in the laws are increasing the initial training to 15 hours and requiring mental-health training for law enforcement officials who conduct training for other officers.
“I think it will result in less mentally ill people being criminalized,” Beall said. “We can start to treat it as an illness and not a crime.”
But even for the deputies who have had ongoing training — a number Sheriff Tom Bosenko said he didn’t know — Bosenko said situations will sometimes escalate to violence.
“(Deputies) still have to protect themselves or others,” Bosenko said, “up to and including lethal force.”
For an armed mentally ill person, the difference between a talk, a zap with a stun gun or a hail of bullets basically comes down to the specifics.
“If they pull a weapon, OK, what type of weapon? How far away are they? If a person had a knife and is 50 yards away, it’s different from if they’re 5 feet away.” Bosenko said. “(Deputies) use all of their skill sets in training to try and resolve the situation with the least amount of force possible.”
Of course, not all interactions between law enforcement and mentally ill people involve a weapon.
When someone is in a mental health crisis but hasn’t committed a crime and doesn’t meet the criteria for a mandatory 72-hour hold, there’s little that can be done, Bosenko said. Deputies can make referrals for treatment, but the person “would have to avail themselves (of) that voluntarily.”
More training “certainly doesn’t hurt,” Bosenko said, but it also would add to the length of the academy for new deputies, which “can get into a cost factor.”
At the Redding Police Department, the training scenario is similar: All officers train on mental episodes at police academy, but only some get extra training beyond that.
Lt. Pete Brindley said 64 of 102 sworn officers at the department have between eight and 40 hours of that ongoing training — specifically, Crisis Intervention Team training, a special program put on by the National Alliance on Mental Illness that teaches officers strategies for handling people having an episode.
“We’re constantly just trying to get more and more officers exposed to that training,” Brindley said. “A portion of our calls on any given day have to do with the mentally ill or those that are suffering from substance abuse. A lot of times they’re interrelated, and so ... we want to do whatever we can to mitigate those calls to try to prevent them from turning to a violent confrontation. The earlier we can get that intervention done, the better off everybody is, not only the patient, but the other citizens as well.”
But low staffing levels prevent all officers from going to the trainings.
“A lot of it comes down to staffing,” Brindley said. “Who we can send and when depends on our manpower and availability.”
Beall, a former San Jose City councilman and Santa Clara County supervisor, said he’s seen the benefits when police forces have all their officers do extra mental-health training beyond the academy requirement.
“The police officer can’t jeopardize their safety, but if they’re trained, they can make an attempt, if it’s the right protocol, to de-escalate and to talk them down and to try to find resources for the person,” he said.
And it’s not just the mentally ill person who benefits — Beall said Bay Area Rapid Transit officers are now all required to have ongoing mental-health training, and worker’s compensation claims have dropped significantly as officers get in fewer scuffles with mentally ill individuals.
Without ongoing training, the Redding Police Department is working on programs to help all officers better deal with mentally ill people.
Brindley said a pamphlet is in the works that officers will hand out to people who don’t meet the criteria for a mandatory 72-hour hold and aren’t ready to seek out treatment, so they at least know where to go if and when they are ready.”
The department also is working to train officers with the “TACT” model, which teaches them to modify their tone, atmosphere, communication and tactics when dealing with a person in crisis.
“It’s recognizing that if somebody is suffering from a mental health episode, they’re not necessarily going to react as somebody in a normal state would react, and recognizing some signs and symptoms of suffering,” Brindley said.
The idea is realizing law enforcement’s treatment of people in crisis may influence the outcome of that interaction, Brindley said.
“The tone of your voice may dictate that person’s actions. ... Let them know (we) are there to help and that we’re concerned for their safety,” he said. “Using that as a tool ... to try and de-escalate things so that it doesn’t come to that use of force. Are those tools going to work every time? Absolutely not. But the more options we can get the officers, the better off we are at (more safely) dealing with those situations.”
Training aside, the main problem Redding officers face is a lack of options to help the mentally ill people they encounter, Police Chief Robert Paoletti said.
“The frustration on the officers’ side is that there is no place to take them other than the ER or jail,” Paoletti said. “And we recognize that that’s not the best place for them to be. The only thing my guys can say is, ‘Look, you need to start behaving yourself.’ And that’s not a good negotiation point. We need crisis intervention where we can take people that day. When we don’t have those resources, a lot of them keep using drugs.”
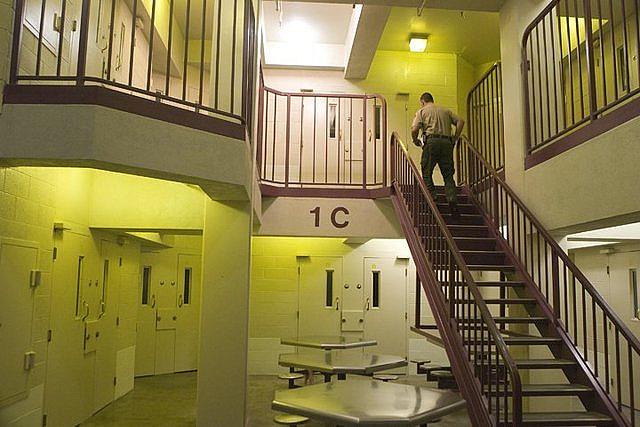
JAIL: ‘THE SAFETY NET’
When Capt. Janet Breshears came back to Shasta County Jail after doing other law enforcement work in the area, she was struck by the changes she noticed in its mentally ill inmates.
“I’ve been here almost 27 years — I know the difference from when I first started,” she said. “The mentally ill we had back in 1990 compared to now — it’s not even comparable, just the extreme violence. They’re much more violent. They’re much more psychotic. I don’t know why ... I mean, we all talk about it. Is it just us? Did I forget?”
Breshears said some believe mentally ill people now use stronger drugs and dangerous combinations of them to medicate themselves. The behavior associated with withdrawals also “can become very bizarre and violent,” she said.
While Bosenko said there isn’t a way to quantify exactly how many inmates at the jail are there because of a crime related to their mental illness, numbers do show that more and more local inmates are on medication for mental illnesses. Data provided to the Record Searchlight indicate treatment for psychiatric disorders in Shasta County Jail inmates has steadily climbed since 2008. Currently, about 20 percent of its inmates are on psychiatric medications, compared to 12.6 percent in 2008, with that percentage growing slightly almost every year between.
Other officials also said it’s hard to determine exactly how many are jailed because of a crime related to their mental illness, since there’s no such category for bookings and some people with mental health issues commit crimes that aren’t directly related.
As for once they get to jail, correctional deputies are trained to deal with mentally ill inmates, but the recent Blueprint for Public Safety from Matrix Consulting Group recommended more. “Essentially what happened is, our prisons turned into giant mental health facilities with staff not even qualified to deal with those situations,” said Jon Van-Fossan, a mental health practitioner who also serves as the county’s clinician for Assembly Bill 109 offenders, who would have been under state parole before the bill became law in 2011.
Indeed, study after study has shown that jails have picked up the burden as the state has pared down mental health services over the years.
For example, a U.S. Department of Justice survey from 2006 found that nearly 25 percent of jail and prison inmates with a mental illness had served three or more previous sentences, compared to about 20 percent of non-mentally ill inmates.
That survey also found that local jails had higher percentages of inmates with psychotic symptoms than both state and federal prisons.
“Jail really does nothing for someone who has a mental illness,” said Shasta County Supervisor Leonard Moty, a former Redding police chief.
Those inmates can be combative with others, and it costs more to treat them, said Leon Evans, chief executive officer of the Center for Health Care Services, who developed a jail diversion center in San Antonio, Texas that’s considered a national model.
“We’ve shut down our mental institutions over the years so law enforcement … are the safety net,” Evans said. “Do you see the problem? The wasted life, the wasted tax dollars?”
What’s more, punitive systems generally don’t register with severely mentally ill people the way they’re meant to, Van-Fossan said.
“When you give a consequence to somebody with mental health issues and you expect it to be a tool to actually learn from, it’s like throwing gasoline on a fire,” he said. “They’re stuck in their own heads. They’re just swimming in their emotions and feelings. It effectively makes things worse.”
Over at the jail, Branch’s son is in custody — again.
His rap sheet this time includes — among charges such as threats, battery and vandalism — a count of elder abuse. That’s because in his latest episode, Branch said, her son terrorized his father.
“He doesn’t know he’s doing it,” she said. “He doesn’t seem to want to hurt people. It’s more, he doesn’t understand.”
Branch remembers what her son was like before his symptoms started to manifest when he was around 23. He worked in construction and got all the tough jobs because he’s naturally strong.
“He actually had a really good work ethic,” Branch said.
A co-worker once even remarked that he was the only one who came to work every day on time, dressed nicely and with his own lunch.
“He said nobody else did that,” Branch recalled.
Now, Branch said, her son’s behavior has gotten so bad she recently put him up in his own trailer because she couldn’t take the stress of living with him.
“It’s like being terrorized all the time,” she said.
Some people ask Branch why she doesn’t just cut ties altogether.
“He’s my son,” she tells them.
SOCIALIZATION GROUP
Inside the jail, new programs are emerging to help mentally ill inmates manage their lives.
At weekly Socialization Group, a mental health professional gives those inmates a sort of hybrid between a support group and a life-skills class.
“You could easily isolate yourself (in jail), and it’s teaching them they all need to get along,” Breshears said. “It gets them interacting with others. They start to care about each other. They watch out for each other.”
Another one of the instructors is a fellow inmate: Shawn Bradley, who is not mentally ill but said he wants to use his time in jail for good by helping those who are.
“We’re locked up in here. Time is going on, but time has stilled for us in here,” he said. “If I can bring a smile ... or give them hope for the future, then I will do so. It’s like the only thing we have to look forward to out of our cells.”
He teaches fellow inmates social skills such as anger management, but also general life skills that sometimes elude the severely mentally ill, such as keeping appointments.
Bradley said he sees firsthand how the inmates’ illnesses cause them to commit crimes.
“There’s really nowhere for them, and so they go to jail,” he said.
But Bradley also sees their potential for redemption and recovery.
“These guys can do well,” he said. “They can fit in society. I think there’s a place for them.”
Bradley said officials seemed dubious when he first proposed helping out with the group, but he sent a letter asking for permission and received it.
He said it’s his first time in the criminal justice system — he was arrested for his alleged involvement in a Trinity County shooting death — and the group helps him stay sane, too.
“It’s a lot to handle in a place like this. It helps me feel normal,” he said.
Breshears said she’s also noticed the positive effects of socialization group.
If an offender doesn’t show up one week, Breshears said the others will push him or her to try again.
Still, others who enter the jail mentally ill leave without apparent recovery, even after multiple attempts.
Outside the jail on the same day Bradley described the socialization group, Leticia Reyes stood on the steps waiting for a ride.
Reyes is a self-described schizophrenic who has said the voices in her head caused her to break windows, landing her in the jail some four years ago.
Reyes said in a 2013 jalhouse interview that she didn’t want to take medication because she believed God would heal her.
After a stint at Napa State Hospital that was supposed to have restored her mental competency, two more psychologists decided Reyes needed another stay at Napa this year.
But it didn’t happen. She reached the statutory limit for having her competency restored — over three years in jail — the case was dismissed and she was released last month.
Reyes said in 2013 that she didn’t want to cause any more damage, so she would “try to stay strong” if she’s released.
“I don’t like destroying my community.”
‘GIVING PEOPLE HELP AND HOPE’
Matthew Fox knows what his life would be like without the county’s behavioral health court program.
“If I wouldn’t have had this opportunity, I’d be dead right now or in prison,” said Fox, who was 24 at his June graduation from the program. “They blessed me with a new life.
The program kicked off in January 2014, giving certain mentally ill offenders who commit felonies intensive supervision and therapy in an effort to stop the revolving-door effect.
“I think a lot of it is just showing these individuals respect and that we do care and that we do want them to succeed,” said Judge Greg Gaul, who oversees the program. “Many of them are obviously very salvageable.”
“If you spend the time and you work on the situation, you can solve those problems,” Gaul said at the June graduation.
Gaul went on to tell the story of Dan Brown, who — before the program — continually violated his probation. Among other things, he tested positive for methamphetamine numerous times.
But now, “He’s like the No. 1 guy in the program,” Gaul said. “He’s displayed honesty, integrity, dedication and kindness.”
As Gaul continued detailing Brown’s achievements in the program, Brown gave a thumbs-up and a satisfied, “Yeah!” before sharing a few words.
“I still hear voices, but I don’t let it bother me,” Brown said. “I am still a drug addict, and I am crazy. ... I can never do drugs again. Not even once. And I have to take my meds or I will go crazy. So if I do either one, I will be locked up, or worse.”
Brown ended each stanza of his prepared speech with a line symbolic of his recovery: “I could say more, but I’m moving on.”
He sat down and received a congratulatory handshake from Fox, who later stood up to speak for himself.
“In the last year, life has gotten so good, it’s amazing,” Fox said, tearing up.
Fox told the audience he got his son back in his life and now has “true friends who don’t want anything from me but my time.”
His recovery felt like a dream, “and I’m going to wake up in my dealer’s house or something.”
Fox concluded by showing the audience his booking photo depicting a scrawny man in a tank top. He’d nearly doubled his body weight since going off drugs.
Another graduate, Robert Salazar, stepped up to the podium, took out a folded piece of paper from his pocket and quietly began reading, his face propped up on his elbow.
“When I first got accepted into the behavioral health court program, I was unsure about everything,” he read. “I started to build trust once. ... I was put on the right medicine. My thoughts became more and more clear. ... I see things differently now. ... I feel like I have value and that they really care for me.”
Salazar told his fellow graduates they have value, too.
“This behavioral health court program is one of the best things that has happened to Shasta County,” he said. “It is saving lives, giving people help and hope that would be locked away in prison.”
Because of his successful completion of the program, Gaul followed up by noting that Salazar’s probation would be terminated early and his three felony cases were reduced to misdemeanors.
While it’s a life-changing opportunity for a select few, it can’t ease the overall problems in the county — at least not as the program is currently envisioned.
It’s kept small right now — about 15 participants — in part because of resources but also because it’s not the type of treatment that would work for a large group of people at a time, Gaul said.
In addition to size restraints, the program is only for people with felonies and not for those with personality disorders, such as antisocial. Their distorted worldviews require intense therapy, Gaul said, often for years.
“They really need one-on-one counseling,” Gaul said. “They’re extremely difficult to deal with.”
And it doesn’t work for everyone who actually is eligible.
“We’ve had a lot of people that have failed it; a lot of people are struggling with it,” Gaul said, noting some have failed multiple times. “We expected it.”
But they’re usually given another chance, Gaul said, and that seems to be part of the formula for success.
“We’ve got some really good success stories,” he said. “A lot of times, it’s just a matter of getting their mental health meds. It’s like night and day. You see these guys turn on and off in a matter of a couple of weeks.”
The program essentially doesn’t have any funding, just the in-kind donation of services from those who thought it was important.
“I think everybody agreed, we’ve got too many people in the jail and there needs to be some released. There are too many cases,” he said. “We just keep seeing the same faces. So let’s start dealing with those same faces and start turning them around.”
[This story was originally published by Record Searchlight.]