Whistleblowers Call Out California Group Home for Abuse Against Disabled Residents
The story was originally published by the KQED with support from our 2022 Data Journalism Fellowship.

Pat Turner hugs his daughter Katrina Turner, who is developmentally disabled and nonverbal, during an outing provided by the care home where she resides near Sacramento, Calif., on Oct. 23, 2023.
Beth LaBerge/KQED
Katrina Turner’s eyes lit up when her father, Pat Turner, and his fiancée, Elaine Sheffer, walked through the door of the beige stucco house in the Sacramento County community of Fair Oaks, where she lives. She made soft moaning sounds as her parents embraced her. Katrina is 43 years old, developmentally disabled and nonverbal, but she has her own ways of communicating.
Katrina’s family has been worried about her. Just a few months after she moved to this group home for people with disabilities who need 24-hour care, known as an Enhanced Behavioral Supports Home (EBSH), mysterious injuries started appearing on her body. There were holes in her walls, and Katrina had become less responsive.
Turner and Sheffer were used to facilities letting Katrina down. Children with disabilities are far more likely to experience abuse, and they said Katrina is no exception. Scars from past placements mark her skin, they said, and although she’s barely middle-aged, Katrina walks with the stooped shuffle of someone much older. But her family had hoped that here, at the Illinois Home — an EBSH named for the street where it’s located — Katrina had finally found a place where she’d get the 24– 7 care she needed.
Instead, Turner and Sheffer’s concerns have turned into a full-fledged investigation of the management and practices at the Illinois Home.
EBSHs are supposed to be more tightly regulated than any other type of group home in the state. However, a KQED investigation into the Illinois Home and the company that operated it until June 2023 has revealed that staff were not meeting even minimum standards of care. Allegations of mistreatment are difficult to prove because the main victim, Katrina, is nonverbal. However, investigation records, state reports, and testimony from whistleblowers suggest that she suffered abuse and neglect for months at the hands of staffers, and state regulators failed to act promptly.
As small group homes proliferate, so do oversight concerns
The Department of Developmental Services (DDS) is the state agency charged with supporting the roughly 400,000 people in California who live with developmental disabilities like autism, cerebral palsy, or Down syndrome. DDS oversees a budget of more than $14 billion, nearly as much as the state’s correctional system. The agency funds thousands of organizations that provide services — like day programs, behavioral therapy, and group homes like the Illinois Home, where Katrina lives. Only four residents live in each home, a system designed to meet the high needs of the residents. These homes, often just converted houses in residential neighborhoods, replaced the large state-run institutions that state lawmakers voted to move away from in 2012. Advocates had high hopes that in these smaller settings, disabled Californians like Katrina would finally get the care promised to them by law.
“We’re concerned that in practice, some of these homes are at risk of turning into the very types of institutional placements they’ve been designed to prevent, just on a smaller scale,” said Will Leiner, managing attorney at Disability Rights California, a nonprofit that advocates for the rights of disabled Californians.
We were hopeful because an EBSH home is overseen by the state. We were hopeful that this would mean there wouldn’t be such an opportunity for neglect or abuse… We thought everything was gonna be OK. But it’s not. It’s horrible
Elaine Sheffer
Leiner is also concerned by what he said is a staggering growth in the number of EBSHs.The first one opened in 2017, and now, just six years later, nearly 70 licensed EBSHs operate in California. And while they are smaller than the institutions that came before, they aren’t always well regulated. In 2022, the California State Auditor found that DDS had failed to ensure residential facilities like EBSHs received the inspections and oversight that state law requires. Furthermore, the State Auditor noted the same issue in a 2016 audit and “recommended then that DDS require the regional centers to address the issue. However, DDS has yet to take adequate action to ensure that the regional centers perform these reviews.”
Katrina’s life in group home care
Since she was a child, Katrina Turner has lived in group care facilities. She was often destructive, sometimes hurting herself or others, which made finding a stable living situation difficult. She bounced from one home to another, frequently experiencing mistreatment, according to her family. At one point, she spent over six months in a hospital room because the state wasn’t able to find a suitable placement for her.
Her family was determined to get her somewhere safe. So when they heard about an opening at an EBSH near their home in Sacramento, they were excited.
“We were hopeful because an EBSH home is overseen by the state,” Sheffer said. “We were hopeful that this would mean there wouldn’t be such an opportunity for neglect or abuse. She moved to the home, and we thought everything was gonna be OK. But it’s not. It’s horrible.”

Elaine Sheffer goes through paperwork related to her stepdaughter Katrina Turner at home in Sacramento. Investigation records, state reports and testimony from whistleblowers suggest that Turner suffered abuse and neglect for months at the hands of staffers at the Illinois Home.
Beth LaBerge/KQED
Katrina moved into the Illinois Home in March 2021. The facility was under investigation by the state at the time, something Turner said they knew nothing about.
Just a few months into her stay, a new company, Sevita Health, took over its operation. Sevita is one of the country’s largest operators of group homes and care facilities. Turner and Sheffer didn’t question the acquisition at the time, but about a year into Katrina’s residency there, her family began to suspect something wasn’t right.
Abuse and mistreatment
In February 2022, Elaine Sheffer received a surprising text and then an email from a Sevita staff member, Kylie LeBlanc.
A copy of the email obtained by KQED described a series of abusive incidents involving Katrina. Attached photos showed Katrina looking mournfully at the camera, with a deep, raised purple blotch spreading below her eye.
“When I walked in, Katrina had a black eye, and I was like, ‘Oh my God,’” LeBlanc said. “And my coworker said, ‘Kylie, it’s not even the worst part.’”
Along the walls of Katrina’s room, exactly at the height of her head, was a row of holes. LeBlanc believed they were caused by Katrina banging her head against the wall.
According to LeBlanc, the coworker told her, “‘I know people are locking her in the room. They’re closing the door and holding it shut while sitting in a chair.’”
Because of her history of self-injury, Katrina is supposed to be monitored at all times. Being locked in her room would have been confusing and frightening for her, LeBlanc said, and she may have resorted to self-injury.
Shift notes provided by Katrina’s family and another former Sevita employee showed that Katrina had repeatedly suffered injuries during night shifts in the weeks leading up to the black eye, including bruises.
Turner and Sheffer said they weren’t notified about the black eye by Sevita Health, as is required. They believed that, had LeBlanc not reached out, the family would have been kept in the dark. They also believed Katrina had suffered a concussion from the incident.
“She was also at that point having issues with throwing up and losing control of her bowels,” LeBlanc said. “Which is another sign of some kind of head injury or a concussion.”
Inaction from regulators and Sevita Health
LeBlanc said that she submitted complaints about the treatment of residents to Sevita Health’s HR department but that the company did not take action. So, she took her concerns directly to Alta Regional Center, a state-funded nonprofit conducting safety checks, and Community Care Licensing, a state regulator investigating complaints. She sent documents describing the concussion incident, as well as evidence that staff had been mismanaging residents’ medications. Documents KQED obtained from Community Care Licensing corroborate LeBlanc’s claims.
Additional shift notes show Katrina was repeatedly found drinking from a toilet and a sprinkler head outside. These reports suggested to Katrina’s family that she was not receiving enough water, indicating serious neglect.
After an initial meeting with representatives from the regulating agencies, LeBlanc was hopeful that change was coming to the Illinois Home.
“They said they were gonna do things to fix it,” she said. “And absolutely nothing happened.”
Alta Regional Center said it did take action. In response to KQED’s questions, Alta wrote that between March 2022 and June 2023, the Illinois Home was “required to develop a corrective action plan and the Regional Center stopped referring new individuals for placement there.” This practice is known as “sanctioning” and is a way to blacklist a facility. But, though the Illinois Home was prevented from taking in new clients, Katrina and the other residents remained.
‘Absolutely no oversight’
Around the same time LeBlanc was blowing the whistle on practices at the Illinois Home, Sevita hired a new administrator named Ileya Silva to oversee it. She’d worked in group homes for 20 years and had developed a reputation for doing things by the book.
Silva was shocked by what she found at the Illinois Home. It appeared to her that during the eight months between Sevita’s acquisition of the home in July 2021 and her hiring, there had been “absolutely no oversight.” A facility report from Alta Regional Center reinforces Silva’s account.
That means Sevita was not doing the typical things required to operate an EBSH, including internal audits, check-ins and inspections. Silva said employees were severely undertrained and lacked even the most basic knowledge of the regulations.
I don’t want this to be the situation where I turn on the news one day and one of the clients has died. I just can’t have that on my conscience — that I didn’t say something, I didn’t do something.
Ileya Silva
The Alta Regional facility report shows that staff members at all levels were behind on training and missing certifications. Some staff didn’t even have the required experience to work at an EBSH.
To compound the problems, the home was chronically under-staffed and employees worked long hours — sometimes 16 or even 24-hour shifts, according to Silva and LeBlanc.
And the Illinois Home wasn’t an isolated case, Silva said. Sevita operated two other group homes nearby and at least 20 other homes throughout California.
“It was very systemic,” Silva said. “They would send staff from other facilities, and they were at the same deficit. They didn’t have the understanding. They didn’t know the [regulations].”

Ileya Silva, a former group home administrator at the home where Katrina Turner lived, stands outside her home in Sacramento.
Beth LaBerge/KQED
KQED provided Sevita Health with a detailed list of allegations and questions. The company declined to comment on specifics, citing the privacy of their residents, but did provide a general statement: “Sevita promotes ethical practices at all levels of the organization, and we remain committed to our core values of integrity, respect, inclusion, and growth.”
Medication mismanagement
One of the clearest examples of just how bad things were at the Illinois Home was how staff handled medications. Every dose of every medication in an EBSH is supposed to be documented, both for the safety of residents and to prevent misuse.
“In this field, staff do steal medications,” Silva said. “It’s why there are so many checks and balances.”
Silva said the standard protocol was to destroy unused medications at the end of each month. At the Illinois Home, however, “they had a year’s worth of backed-up meds that had not been destroyed.
“I have photos of a giant, gallon freezer bag that had maybe 150 pills in it,” Silva said. “Didn’t state what the medications were, didn’t state who the medications belonged to.”
Silva also noticed that all of the residents were on multiple strong medications at extremely high dosages. Katrina, for example, was on anti-psychotics, sedatives, and other powerful medications.
“It’s not very often that you’re gonna see all of the meds, and so many of them, prescribed at the maxed-out level,” she said.
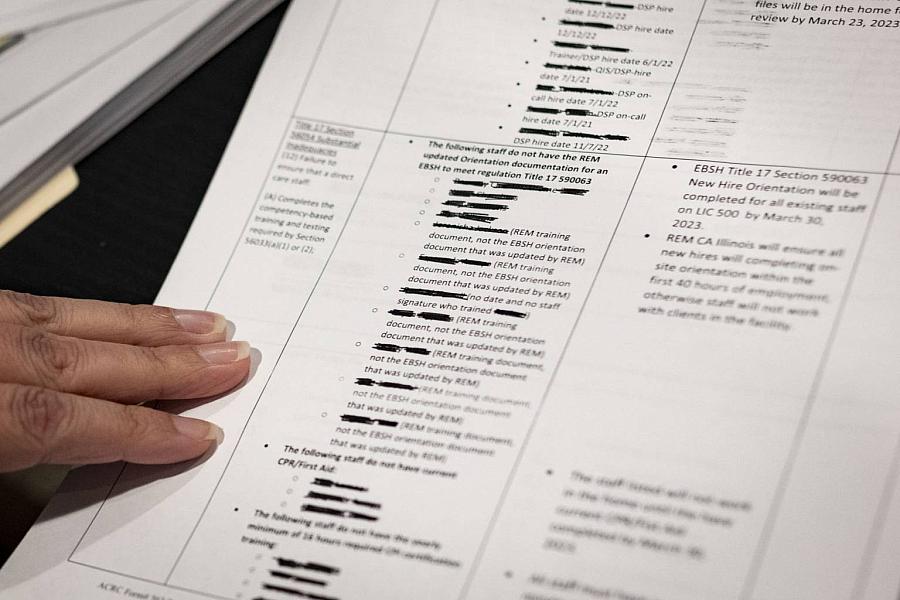
Ileya Silva goes through paperwork related to Katrina Turner’s treatment at the Illinois Home.
Beth LaBerge/KQED
California welfare code says that people with developmental disabilities have a right to be free from harm, including “excessive medication.” When medications are used to sedate a resident or make them more compliant, that’s considered chemical restraint by the state and is only permitted in very limited circumstances. Silva was concerned that all the residents in the home were being chemically restrained. It was a concern shared by Katrina’s family.
“She’s walking hunched over, and she walks like a little old lady,” Sheffer said. “And her mouth is open, and she’s drooling. And we’re like, this is not Katrina.”
Van ride violence
One of the most shocking instances of abuse came in June 2022. Illinois Home staff often transported residents to appointments and activities in a van. Katrina sometimes took her seatbelt off and attempted to stand up while the van was moving. Reports show that several staff members would slam on the brakes rather than gently helping her back to her seat, causing her to fly across the van.
“So that explains a lot of the bruises that she had on her lower back and the front of her legs,” Sheffer said.
Reports from a Community Care Licensing investigation indicate that three different staff members were “brake checking” residents over several months. One staffer is quoted as saying that the driver of the van “Will brake check two to three times. Then she was laughing like it’s a joke. Happens all the time.”
Silva suspended the three employees accused of brake-checking Katrina and the other residents. Shortly after that, one of the employees quit, and the other two were terminated.
“I don’t want this to be the situation where I turn on the news one day, and one of the clients has died,” Silva said. “And I just can’t have that on my conscience — that I didn’t say something, I didn’t do something.”
In response to the incidents, regulators increased pressure on Sevita to improve conditions, but the company would continue operating the home for another year. Community Care Licensing issued citations, but documents show the penalties were relatively low. As of August 2023, The Illinois Home had been fined just over $1,500. That’s in contrast to the home’s yearly revenue of over $1.5 million.
In response to KQED’s questions about the Illinois Home and the abuse Katrina Turner suffered, Community Care Licensing wrote, “The Department licenses facilities in accordance with state law.”
In a separate response, DDS wrote, “The actions described in these claims are inexcusable. They not only are inconsistent with the Department of Developmental Services’ (DDS’) expectations for care, but they also are entirely counter to what we stand for and what we expect in the care and support for the individuals who receive regional center services.”
Private equity firms reap profits amid a track record of abuse
Regulators may have responded slowly and with too little force, but Illeya Silva reserves the bulk of her anger for Sevita Health management, who she said could have taken it upon themselves to respond to allegations of abuse and mismanagement. Instead, she said management ignored regulations, failed to follow up on complaints, and fostered a culture of negligence.
Again, Sevita would not respond to specific allegations.
Sevita Health is part of a growing trend of private equity investment in the health care industry. The company is owned by two private equity firms: Centerbridge Partners and The Vistria Group. Private equity firms use money from investors to purchase private companies and then seek to increase their profitability, often by cutting costs. In health care fields, this can include reducing expenditures on staffing, training, and overhead.
In fact, the name Sevita Health only goes back to 2021, when the company rebranded itself. The company’s previous name, The Mentor Network, had developed a strong negative reputation.
“It has had a host of allegations of abuse, neglect, mistreatment of people under Mentor Network’s care,” said Eileen O’Grady, a lead researcher at the Private Equity Stakeholder Project, a nonprofit that researches private equity’s impact on communities and industries, including group homes. In 2022, she authored a report that digs into the allegations that have swirled around the company.
One of The Mentor Network/Sevita’s major lines of business is running youth foster homes. In 2017, a U.S. Senate investigation found that, over a decade, at least 86 children died at homes run by the company, many more than the national average. And the committee found that the company only conducted internal investigations in 13 of those deaths.
That Senate investigation was partly prompted by a sweeping 2015 investigation by Buzzfeed News. In one article, Buzzfeed “identified deaths, sex abuse, and blunders in screening, training, and overseeing foster parents at the nation’s largest for-profit foster care company.”
In 2020, the U.S. Senate investigated Sevita subsidiaries in Oregon and Iowa that ran homes for disabled adults. It found residents were subjected to abuse, including sexual abuse, substandard care, lack of training, and extreme neglect. In one 2017 case in Oregon, a resident’s bed sores became so severe after months of neglect they had to be relocated to a hospital over 200 miles away for treatment.
In 2018, a Sevita program supervisor in Iowa groomed a developmentally disabled resident for months before sexually abusing them. The supervisor was eventually arrested and pleaded guilty.
Throughout that time, The Mentor Network/Sevita was also highly profitable.
“The last two private equity firms that bought it in March 2019, CenterBridge Partners and the Vistria Group, have piled debt onto [Sevita Health] and used the proceeds of that debt to pay themselves hundreds of millions of dollars,” O’Grady said. “It’s unconscionable that they should be making profits hand over fist while the company is continuing to mistreat the people under its care.”
A dysfunctional cycle
Through the fall of 2022, Ileya Silva continued to push for more transparency and accountability within the company, which she said strained her relationships with her superiors.
“I was seen as a problem because I wasn’t moving in the manner of ‘we’re protecting company over all else,’” she said.
Eventually, Silva was suspended from her job.
On June 30, 2023, Sevita Health voluntarily gave up the operation of the Illinois Home after increased pressure from regulators — nearly a year and a half after Katrina’s black eye and concussion incident. According to the Department of Developmental Services, Sevita Health no longer operates any EBSHs in California. However, it continues to run 24 residential facilities and a number of day programs for adults with developmental disabilities in California.

Elaine Sheffer and Pat Turner spend time with Katrina Turner at Miller Park in the suburbs of Sacramento on Oct. 23.
Beth LaBerge/KQED
Katrina Turner’s family said they’ve met with the new home operators, and their impressions were positive. But, due to the trauma of the past year and a half, they remain unconvinced that the system will protect Katrina if things go south again.
One potential bright spot for Katrina’s family is a bill slowly making its way through the state Legislature over the past year. Assembly Bill 1147, or The Disability Equity and Accountability Act, aims to address some of the systemic issues facing California’s developmental disability system. Among other changes, the bill would force regional centers and private nonprofits that contract with DDS, such as Alta Regional, to be more transparent by subjecting them to the state’s Public Records Act. It would also strengthen DDS’s ability to hold regional centers and service providers like Sevita accountable for failing to meet standards of care. However, regional centers have succeeded in removing key components of the bill and remain strongly opposed.


