Southern California ERs look for answers to the crush of newly insured patients at their doors
This story was reported in partnership with the California Data Fellowship, a program of USC’s Center for Health Journalism.
Other stories in the series include:
Southern California emergency room use has actually risen after the passage of Obamacare
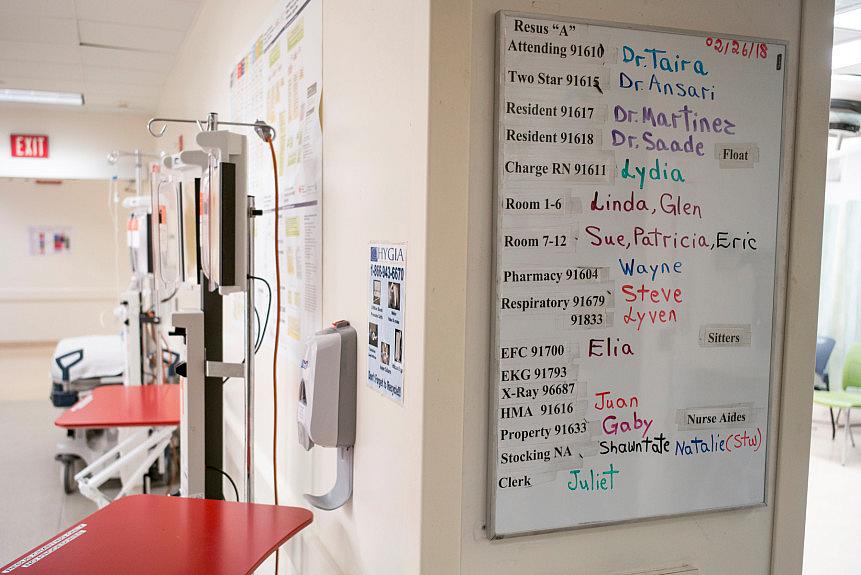
An assignment chart in the ER at County USC, one of the busiest emergency departments in the state. (Photo by David Crane, Los Angeles Daily News/SCNG)
Second in a four-part series that examines emergency room use in Southern California.
As the medical director for the Los Angeles County Fire Department, Dr. Clayton Kazan sees the crunch at the doors of the emergency departments and says more hospitals need to come to the table to talk about how to ease it.
“If you look at the numbers, the visits are up and the admissions are down,” he said, meaning those who need beds may not be getting them.
One solution to allay the high numbers may be a pilot project Kazan and the Los Angeles County Fire Department are trying out: a mobile integrated health care unit. The goal is to see if a “health care on wheels” model can help crowded emergency departments — which in Southern California saw a 27 percent increase in patients from 2010 to 2016 — by steering 911 callers toward urgent cares or other options.
His department has noted that the volume of 911 calls was up significantly and the department expected to field more than 400,000 calls for emergency medical services in 2018. The 911 system becomes the default health care provider; it’s a system that needs to change with the times, he added.
Kazan and other emergency department directors across Los Angeles say that urgent cares and community clinics need to extend their hours to care for the working-class people, who end up in ERs at higher rates. And there’s a need to educate the public on what their health insurance covers, he said.
“A lot of health plans pay for other resources,” he said. “People just don’t know all the resources they have.”
The California Hospital Association has co-sponsored AB-1795, a bill introduced in January by Assemblyman Mike Gipson (D-Carson) that would allow ambulance companies to take patients with non-life threatening mental health issues to urgent care centers, or those who are intoxicated to a sobering center — places they can receive targeted treatment.
Kazan and the Los Angeles County Board of Supervisors support the effort.
Jan Emerson-Shea, spokeswoman for the California Hospital Association, agrees there are ways to steer patients to other resources, but it’s not easy.
“This would be a small start as a way to calm the ERs from people who don’t have the clear medical need,” she said. “Most hospitals don’t have those services and the patients often languish.”
She also said hospitals are at the table when it comes to offering solutions, including setting up more urgent cares and merging with universities and clinics to expand their networks. And she noted more are effectively using technology, such as apps on smartphones and telemedicine, to direct people to the right place for their needs.
“What you’re going to see in the next decade or so, is the care delivery system is going to look different,” Emerson-Shea said. “I can tell you there is a lot of talk among hospitals in our field about health care consumerism. More and more hospitals and health care (organizations) have to rethink how to do business.”
From the other side
Staff at community clinics agree that more people need to be educated on what their plans cover, said Louise McCarthy, president and CEO of the Community Clinic Association of Los Angeles County.
“People with insurance often inappropriately use the ED because of a lack of effective education on how to use their insurance and the services available to them in the community — this includes services in the community clinics, including preventive care that could help them avoid an ED visit in the first place,” McCarthy said.
She said the staff within the emergency departments also lack information on where to send patients for more appropriate care.
“Additionally, with no out-of-pocket costs for an avoidable ED visit in Medi-Cal, there is no financial incentive for enrollees to use more appropriate care,” she added. “We’ve made major gains in expanding coverage in Los Angeles, but we haven’t succeeded at helping enrollees use their benefits effectively.”
McCarthy said clinics are more likely to offer culturally competent, comprehensive services for people seeking care at a cost significantly lower than a hospital visits and some are expanding hours and same-day appointments, such as Clinica Romero, which sees patients up to 8:30 p.m. at its Pico-Union location, while KHEIR’s Wilshire clinic is open Saturdays. Many clinics have urgent care centers.
As a result of funding through the ACA, Los Angeles community clinics now serve 1.6 million patients a year, up 23 percent since 2010, McCarthy said. These clinics have seen a 141 percent increase in the number of Medicaid patients served over the same time frame. Many clinics across Los Angeles continue to have capacity to serve new patients.
Better care and better access to clinics during off-hours will help, experts said, and though emergency department visits have risen, there is an upside.
The increase in percentage of emergency department visits and admissions by those with Medi-Cal is explained in part by a sizable 11 percentage point drop in the share of trips by the uninsured since 2010. The group made up only 8 percent of Southern California hospital-goers in 2016.
The regional dip in uninsured ER arrivals was most pronounced in San Bernardino County, falling from 20 percent in 2010 to 7 percent in 2016; the share was least affected in Orange County, falling from 13 to 6 percent. Los Angeles County hospitals in 2016 saw the highest rate of uninsured visits in the four-county area at a little more than 8 percent, still much lower than 19 percent six years prior.
But that uninsured 8 percent, which includes people who choose to pay out-of-pocket, still amounts to some 500,000 ER visits per year across Southern California.
“Unpaid hospital expenses still are passed onto insured patients, to the extent hospitals have negotiating power with private insurers,” said Gerald F. Kominski, professor of health policy and management at the UCLA Fielding School of Public Health.
“But the number of uninsured Californians has dropped by more than 50 percent, and even those who don’t qualify for full-scope Medi-Cal benefits can receive emergency Medi-Cal,” he said.
Regular access to care
Kominski said a study with the UCLA Center for Health Policy Research found that low-income individuals who were enrolled in county-based health programs with regular access to care had increased use of hospital inpatient and emergency department services for the first year or so of enrollment, but then had decreased use of those services in later years.
“We concluded that chronically uninsured patients have health problems resulting from inadequate access to regular care and that when they get regular access to care, their use goes up temporarily as they attend to their health problems,” he said. “Once that initial ‘pent-up’ demand is met, they use care at a much lower rate. I expect (emergency department) use in California will follow a similar pattern in the future.”
Despite those positive results, he said the trend of emergency department use visits rising is still worth monitoring.
“If ED use continues to rise, that would suggest inadequate access to primary care, and continued use of the ED to compensate for the lack of adequate community-based primary care,” he added.
After years of sustained rises in ER visits, there are hints that the tide of visits by Medi-Cal recipients could be subsiding at some Southern California hospitals. From January to March this year, CalOptima noted a 10-percent drop in ER visits by Medi-Cal patients in Orange County compared to early 2017, said Bridget Kelly, director of communications.
“More of our members are seeing their primary care physicians,” Kelly said.
Emerson-Shea said she would push back on critics who say that the ACA isn’t working at all, that it relies too much on federal government funds to cover people, and that it should be repealed or allow people to choose to be uninsured, if they wanted.
“I think it’s still absolutely true our health care system is stronger when everyone is included,” she said. “If hospitals are getting reimbursements, then they can continue providing service we all can rely on. That financial security can allow hospitals to beef up their care and reduce wait time.
“It’s not like the issue is solved, but the only path to solving this issue is getting everybody in it.”
[This story was originally published by the Los Angeles Daily News.]


