As health reform action moves to the state level, here are the trends reporters should watch
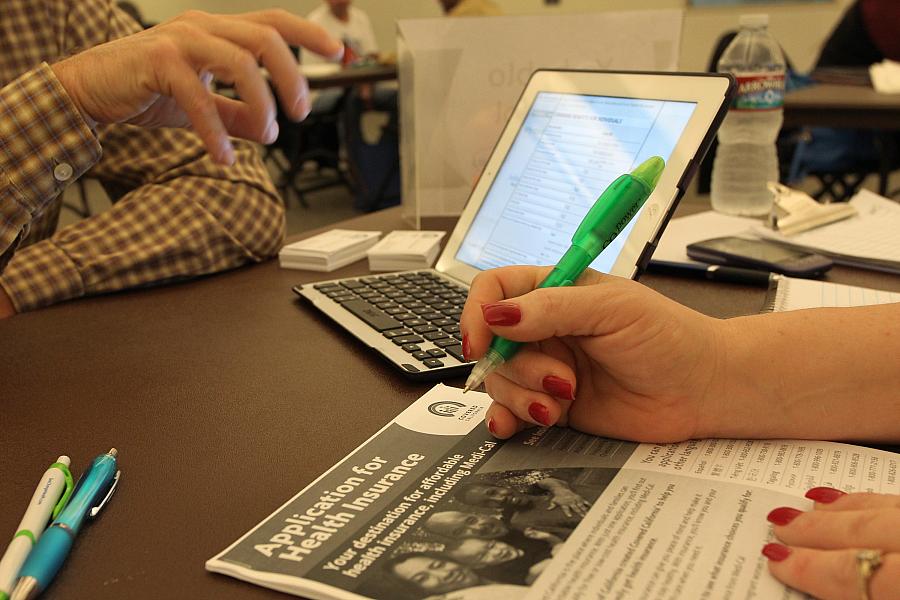
(Photo by David McNew/Getty Images)
As efforts to repeal the Affordable Care Act in Washington stall out, the action on health care policy now moves to the state level. What that means will vary by state. More liberal states might opt to replace the repealed individual mandate with their own state requirement, while more conservative states seek to add work requirements for Medicaid beneficiaries.
That shift in focus to the states was one of the key themes from a Health Matters webinar hosted by the Center for Health Journalism on Monday. Speakers Mary Agnes Carey, partnerships editor and senior correspondent for Kaiser Health News, and Nicholas Bagley, a professor of law at the University of Michigan Law School, detailed the potential state-by-state differences that may emerge in the wake of the repeal of the health law’s individual mandate by Congress in the December tax bill.
“Reporting on how that variation affects people on ground and its implication on state budgets will be an urgent priority in the coming years,” said Bagley, an expert in health care law.
A patchwork quilt of state policies
The Affordable Care Act was supposed to create a uniform health system that would assure near-universal coverage across the country. But that uniformity is now starting to look more like a patchwork quilt. The Supreme Court ruling allowed states the option of not expanding Medicaid, while the repeal of the mandate and proposed CMS rule changes could lead to further differences in coverage throughout the country.
“Those have all dashed the hopes of supporters of the ACA who hoped to have a single national solution,” Bagley said.
As a result, the country in some ways will likely see a return to the era before the ACA, a time in which there was enormous variation in health insurance and policy at the state level, he said.
Bagley outlined various ways states can shape the future of health policy, ranging from adding their own mandate to adopting Medicaid work requirements.
Already, at least nine states are considering their own health insurance mandate, The Wall Street Journal reported earlier this week. But they’ll have to confront the fact that the mandate has always been the most unpopular part of the health law, and the bitterness of the mandate was balanced out by a lot of sweeteners in the ACA, Bagley said. Figuring out a way to get healthy people into the exchange plans is critical, though, since prices for individual market plans could go through the roof without them.
Meanwhile, some states such as Idaho are trying to repeal some of the ACA’s provisions on their own. Before dismissing these efforts, Bagley urged listeners to keep in mind some states’ moves to legalize marijuana, despite their violation of federal law.
Another area of variation comes from a proposed CMS rule that would give states more flexibility in determining the minimum health benefits that insurers must offer in their ACA exchange plans – a change that could lead to variation in costly and controversial coverage areas such as fertility treatments or behavioral therapy for autism, he said.
And, there could be significant state-level variation as more states adopt Medicaid work requirements, something Bagley said will end up costing states more than they’re saving.
“They seem to have a different objective lurking underneath them, which is to get people who don’t deserve our help off the Medicaid rolls,” he said.
Other areas to watch
The big story in health care over the next decade will be the extraordinarily high health care prices, something Bagley called “a real blind spot” for the media.
In the medium term, there will likely be some state initiatives to get a handle on these rising costs. Already, states such as California and New York have tackled “surprise bills.” Another area to watch is Medicaid buy-ins, in which a state could allow anyone to purchase the public health insurance plan for low-income Americans. Bagley said this was basically “a back door way to price regulate providers.”
“Once you’ve bought into Medicaid, you’re taking advantage of the public payer’s leverage in setting a price,” he said. “And you’re allowing individuals to take advantage of those publicly set prices.”
While blue states may be the most likely to embrace price regulation, higher costs of care throughout the country could spur policy maker actions in unexpected places: “I think we’ll see some surprises,” he said. One example: Bagley said the repeal of the mandate will likely hit higher-income residents in red states particularly hard, and that could lead some Republican state legislators to buck ideology and adopt policies to lower premiums.
Covering a 50-state story
Amid this fast-changing climate, KHN’s Mary Agnes Carey offered reporters tips on what to watch.
Carey suggested keeping an eye on Affordable Care Act stabilization bills in Congress, which would reimburse insurance companies for some of the higher-than-expected costs associated with exchange enrollees.
Reporters should also follow a proposal that would allow short-term insurance plans that don’t comply with ACA requirements to be lengthened to 364 days, up from 90. These plans do not have to comply with ACA rules, which means they could reject people for preexisting conditions or not provide the same level of benefits.
In general, the overarching storyline to watch is how states are carving out their own health policy paths. “They can really change the narrative here,” she said.
Carey suggested reporters talk to their state insurance commissioners, who have a lot of power. Think about the decisions they’re making and what’s influencing them, she said. (Here’s a great resource for getting started.)
Other sources include local insurance brokers and consumers. Ask what kind of health insurance shoppers are buying and whether they’re interested in less generous, cheaper policies. Do they even know what short-term plans are? Another story idea: Find people who don’t qualify for ACA subsidies, and ask if they’ll still purchase insurance if they don’t have to pay a penalty.
“I think it’s a really good idea to look at this through the individual beneficiary’s view,” she said.
In states that are seeking federal approval for Medicaid work requirements, for example, are there people who don’t want to sign up for the health plan because of the bureaucratic hassle? How would an individual with a disability get exempt? And, how will states ask Medicaid enrollees to document work status or apply for an exemption?
Even though long-form pieces are useful, sometimes a nice, tight explainer really helps readers understand these complex topics, Carey said.
“The more you can unpack, simplify it, explain this stuff for people, the more readers are going to engage, because they like just-the-facts pieces.”
**
Watch the full presentation here:

