California doles out hefty payments for Hepatitis C drugs
Pauline Bartolone's reporting was undertaken as a participant in the 2015 California Data Fellowship at the Center for Health Journalism, a program of the University of Southern California’s Annenberg School of Journalism.
Other stories in the series include:
The obscurity of drug spending in California's Medicaid program
The other ‘high-cost’ drugs: What specialty drugs mean for California

Keith Cooper via Flickr
The high price of Hepatitis C drugs has sparked an unusual funding arrangement between California and private health plans in Medi-Cal, wherein insurers receive hundreds of millions of dollars to pay for the treatments.
The industry trade association for managed care organizations, which cover care for almost 80 percent of the Medi-Cal population, says the agreement was made after health plans raised “alarm” over the high-cost of the new Hepatitis C drugs. Health plans had to dig into reserves because of the drugs’ costs, according to an industry spokesperson.
“Dollars that were intended for a wide array of medical services started being gobbled up by just one drug,” said Charles Bacchi of the California Association of Health Plans.
Although the members of Bacchi’s trade group directly benefit from the supplemental payments, he says they’re not a “sustainable” solution to the underlying problem of high-priced drugs.
Here are some of the details about the supplemental government funding stream to Medi-Cal plans:
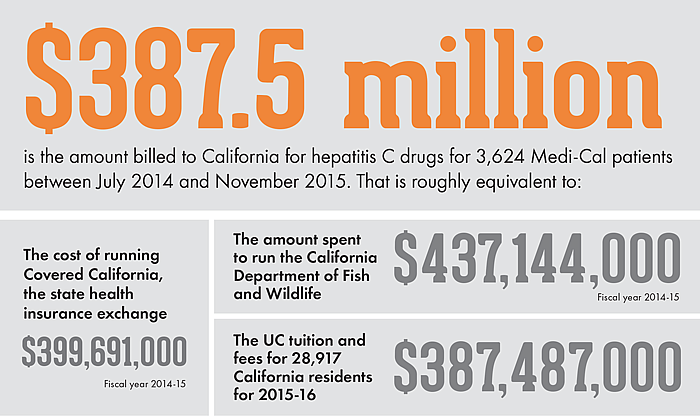
- Health plans invoiced California for $387.5 million for Hepatitis C drugs between July 2014 and November 2015, according to the California Department of Health Care Services. The payments come from a mix of federal and state dollars.
- During that same time period, 3,624 Medi-Cal managed care members with Hepatitis C were treated.
- By our calculations, the payments amount to $106,926 per patient. The number reflects other drugs used to treat Hepatitis C, and isn’t solely the price of Sovaldi and Harvoni.
- Payments to plans are expected to continue next fiscal year. The California Department of Health Care Services has budgeted $303.4 million for health plans for 2016–17.
California receives some money back from drugmakers in the form of rebates, but the ultimate price the state pays for drugs is not public.
Limiting the cost of pharmaceuticals is the basis of a ballot initiative expected to be before voters this November that would limit the amount the state pays for a drug to no more than the lowest price paid for the same drug by the U.S. Department of Veterans Affairs.
The state health care agency says its payments to insurers of Medi-Cal patients for Hepatitis C drugs are a “very unique” solution, one that they may use for other high-cost drugs in the future. The state says the current Hepatitis C payments may be reassessed in a year or two as it expects the price of the drugs go down.
“As the prescribing of the drugs levels off, as the population and the overall nature of who’s getting it settles down, we may get to a point where we look at carving that responsibility back into the plans’ … rate,” said Jennifer Kent, director of the California Department of Health Care Services.
But California’s spending on Hepatitis C drugs doesn’t end there.
For the rest of the Medi-Cal population — the 2.7 million people whose health care services are directly reimbursed by the state — a U.S. Senate Finance Committee reports the following for the year 2014:
- California paid almost $22 million to treat 280 Hepatitis C patients with Sovaldi.
- California paid more than $2.8 million for 57 Harvoni prescriptions.
According to the U.S. Senate report, 237,000 people in Medi-Cal are infected with Hepatitis C. That means less than 2 percent of that population has received the new Hepatitis C treatments.
“In order for taxpayers of the State of California to afford to provide people the necessary treatments,” says Bacchi, “we have to have drug pricing society can afford to pay.”
We’ll be exploring how a drug’s cost affects patient access. If you are a Hepatitis C patient, or other chronic disease patient who is having difficulty getting drugs, we’d like to hear from you.
[This story was originally published by CalMatters.]

