Connecting to AANHPI seniors on mental wellness
This story was originally published in KALW with support from the 2022 California Impact Fund.

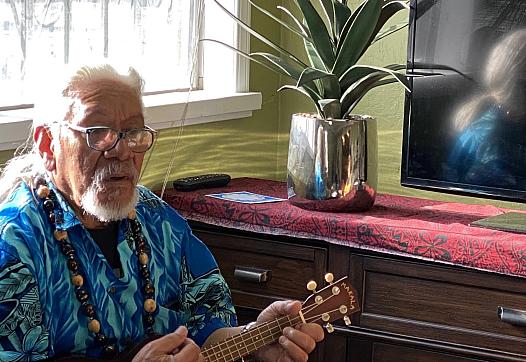
Dr Helen Hsu wants to see more clinicians from diverse backgrounds.
Hella Mental Health
Research shows that adults of Asian American Native Hawaiian Pacific Islander (AANHPI) descent seek mental health services much less than any other demographic group in the country.
And seniors in those AANHPI communities are particularly vulnerable. With families out all day, they can often experience loneliness, anxiety from anti-Asian hate crime, and language barriers to accessing mental health services.
But AANHPI communities are incredibly diverse. So there’s no ‘one size fits all’ solution for this. What does seem to be working is community-led, culturally-appropriate programs that meet AANHPI seniors where they’re at, and recognize their diverse needs.
As part of this mini-series on AANHPI seniors and mental health, clinical psychologist Dr. Helen Hsu unravels some of the challenges facing older people from these communities, and what’s working to help them.
Helen H. Hsu, PsyD, is a bi-cultural, bi-lingual clinical psychologist, clinical supervisor and educator. She is founder of Hella Mental Health and outreach director at Stanford University. She is the former president of the Asian American Psychological Association and the American Psychological Association, Division 45: Society for the Psychological Study of Culture, Ethnicity, and Race. She lives in the San Francisco Bay Area.
Hana Baba:
Tell me the basics of why you think we should be talking about AAPI seniors and the risk of mental health issues.
Helen Hsu:
I think the culturally responsive care that we know now helps all people for their health, their mental health. It's a big issue among Asian American, Native Hawaiian, Pacific Islander communities, because we have so few culturally tailored resources. This is a very large ageing population, AANHPIs have higher numbers of multi generational households. So elders living with maybe a nuclear family, but we have very few services,
Baba:
What are some of the factors that can contribute to mental health issues in AAPI, senior communities in particular, I mean, I can think about my African communities, when when they come here to this country, one thing I can think about is isolation.
Hsu:
The loneliness and isolation, the lack of transportation options, if you can't drive. A lot of our home countries… you didn't need to drive, you had a place to go, you could walk to or take a bus. So here you might find yourself in a huge city or in a distant suburb. Nobody speaks your language, offers your food, you don't have a place to go. So there's isolation and there's also what every person really craves is a sense of purpose and motivation. And so yes, losing that role as an elder in the community, maybe not working anymore, or not having skills that are seen as valuable, here.
There is a good body of work that the Asian American Psychological Association had put out about the impact of anti-Asian hate crimes specifically, which as we know, escalated dramatically during the pandemic. And it impacted seniors definitely, because they were literally being attacked, even murdered, just going about their daily business. So it even further curtailed little independence, they did have that now they had to be afraid, just going to their local market or taking their morning stroll.
Baba:
And then there's the stigma. Can you talk about the stigma attached to talking about mental illness, even?
Hsu:
You know, I was just talking to somebody this morning about tailoring a training program for Asian American specific mental health outreach, public health education. And she said, ‘I noticed that we tend to call it mental wellness in these communities and not mental health’. And I said, Yes, there is a tendency in a lot of our heritage countries to view health as a holistic thing. And so it's okay to talk about maybe being out of balance, about taking care of your mind and body.
But as soon as you say the word mental health or mental illness, or diagnosis, sometimes there's that real stigma of you're saying something is permanently wrong with me, or there's something wrong with my family, or I've never heard about this because we don't talk about it in our culture. So I have this misconception that somebody's either in the hospital, disabled, or normal, with no in between. And of course, the reality is most of us are somewhere in between all the time. But there's a real fear of losing face, of someone thinking something's wrong with me, something's wrong with our family.
Baba:
I want to talk about this UCLA Centre for Health Policy Research reportthat talked about culturally competent services. They said without community specific knowledge of culture, traditions and values, mental health professionals can mis-diagnose, or completely discount the signs of mental health concerns, because individual patient systems of beliefs and values have a significant influence on their like, even their willingness to engage.
So in your experience, what needs to happen to create this community specific knowledge as they are mentioning, San Francisco General, they used to have these culturally competent focus units in the psychiatric ward at San Francisco General back in the day, they are no longer but that was the idea kind of behind them. Why is this even important?
Hsu:
It's absolutely life changing important, right? Whether or not someone gets care and whether they need to get care in time could be the difference of severity, even life and death. And so cultural responsiveness training, engaging the community and community experts is fundamental to how we do that.
And it's not that difficult actually. Sometimes I feel like systems will say, well, that's just too hard. But there are models that do already exist. Like you mention that there were models already in place at San Francisco General. For example, I often, when I teach, talk about the Central Valley of California. There was a program that integrated Hmong shamans into the hospital. So the hospital staff can learn about what kind of spiritual and cultural practices help people feel better and heal better. And the shamans themselves learned about this is what they do at the hospital and how it works. And we can share that with our community, which genders more trust, otherwise they would just never go, or they would just try to go home as soon as possible against medical advice.
And Waianae Coast Comprehensive Health Centre on Oahu has, you know, hospitals, dentists, mental health professionals. They also have a Kupuna elder council that gives advisement, they have traditional lomilomi massage, they have a healing garden. And so this brings people in, in a way that again feels non stigmatising, supportive, healing.
Baba:
So your new book, The Healing Trauma Workbook for Asian Americans. In it, you say it blends contemporary psychology with ancient mind body approaches to help you build resilience in the face of racism, overcoming trauma and internalised oppression, reclaim your mental health, celebrate your heritage. Can you explain a little more and give us some examples of this approach?
Hsu:
In doing psychological work for about 20 years now, what I found was that we have some pretty good tools. But Asian American Native Hawaiian Pacifica peoples clients would say, ‘Well, this is pretty good, and it's a little bit helpful. But none of the materials currently in existence talk about the intergenerational trauma that my family has endured. Maybe the daily microaggressions and racism I'm experiencing, the impact this has on my self image and my identity’.
Or, ‘I have a Western therapist suggesting things to me that are actually against my values’, is something that happens unfortunately, often that a well intentioned Western therapist doesn't understand that your client has very deep values that are maybe different and something should be approached in another way. And that our heritage cultures have long had practices, which helps support mind and body health. So Tai Chi and Qigong and yoga and drumming circles and storytelling circles, elder consults, and of course, prayer, rituals, chants – these have all existed for 1000s of years and have been helpful. And of course, now, Western research is catching up like, ‘Hey, singing really helps depression’. Well, yes, we've known that. ‘Hey, yoga, or Tai Chi is like, helpful’. Well, yes, we've known that even if we use different language for it.
Baba:
Meditation. Yes. When meditation came out, well, not came out. But you know, the research, the trend. People have been doing this for 1000s of years, and you're just catching up?
Hsu:
Now, the research is discovering: ‘Hey, wow, meditation changes brainwaves. Hey, you know, dance actually improves moods art actually helps trauma victims, integrate and organise their experiences’. So these are all wonderful things that I think American-style, capitalistic siloed medicine hasn't quite figured out yet. How do we integrate this in the care?
Baba:
So, if somebody's listening to this now and is thinking about their mother, their father, they're not well, and they want to help them? What can they do?
Hsu:
I mean, speaking with elders is its own thing. But often I really normalize, like, hey, there are things we can do proactively to help you be healthier in mind and body. And a lot of our elders do think about health as a mind, body, spirit, and community experience. So what are things that we could do?
Ideally, often with elders, if you can find community, that's the best place, a community centre or family gatherings, to normalize? To give examples, finding language accessible resources and supports. I work with a lot of college and graduate students and often we're looking up information, say in their parents’ native language about mental health and mental well being, and we prepare that and they actually share that with their parents. Because for bi-cultural, multiple cultural people and families, we often even struggle with the fact that within the same family, we don't quite have the language to talk about these things
Baba:
There's a reverence there, right? Like, am I going to my father and tell him, something's wrong with him? In many cultures, that can't even happen.
Hsu:
You know, I'm at an age now where a lot of us are trying to make very difficult decisions about elder care and safety. And yes, you can go to your respected elder and say, you need a neuro psych eval, I think you're getting dementia. I mean, there's a grief in even having to say that are realise that, and we'll need support going through that.
But also, that's never gonna go well with your elder, but can you talk about, here's some screening tests, I really care about you, I want you to do this, it's something very normal that everyone at this age does, just to make sure we protect your well being as long as possible. So the focus is not on let's diagnose you with dementia, the focus is on if you get a clear exam, that's so great, we'll be so happy. And if there's a cause for concern, then we'll know and we'll start doing things to protect your, you know, strong mind, as long as we can.
But what we have now is that sometimes not being able to have these conversations, not getting the screening means people get much, much sicker than they need to be. And maybe we could have had some treatment that would have slowed the dementia, but we never got it. The growing body of research work, which confirms and validates that these ancient healing techniques that people have been doing all over the world for generations do have efficacy is very promising. And how can we apply that and of course, have things evolved for modern life… very, very slowly.
But there are more clinicians of diverse backgrounds and experiences who are able to bring more of that into our communities. One good example of a promising programme is the very tiny but minority fellowship programme that the American Psychological Association has and that's an example of a programme that recruits, encourages, partially funds, and gives a lot of professional training and mentors to historically marginalised or underrepresented, young people who want to get into health care. And I feel hopeful.