From the Underground to Public Health Policy: A History of Harm Reduction in San Francisco
The story was originally published in KQED with support from the USC Annenberg Center for Health Journalism’s 2021 Data Fellowship.

Rachel McLean holds two pins on orange fabric hearts from the memorial for Pete Morse, at her home on March 10, 2022.
(Beth LaBerge/KQED)
It was 1998, and San Francisco was in the midst of a heroin overdose crisis. Rachel McLean was an outreach worker in the Haight, and she says it felt like a war zone.
When youth in the neighborhood fatally overdosed, outreach workers would host memorials by a bench in Golden Gate Park's Panhandle.
They'd order pizza, tell stories, make zines and write poetry. But then came one three-week stretch with a new overdose death each week.
"And by the time we got to the third memorial, no one could even talk about what they loved and remembered about that person because it was just too much," McLean said. "And I remember a bunch of kids were like, 'You know, 'eff this, I'm just going to go and get high.'"
Heroin prices had dropped and the purity had doubled. From 1997 to 2000, 384 people died from heroin-related causes in San Francisco, making it the city’s single-largest cause of accidental death.
In 2000, the San Francisco Health Commission made harm reduction — a philosophy that advocates for making it safer to use drugs rather than criminalizing those who do — an official public health policy. It's an approach with roots spanning from the Summer of Love in 1967, to the beginning of the AIDS pandemic in the 1980s, to the present-day fight to open sites in San Francisco for people to use drugs safely.

Vitka Eisen, president and CEO of HealthRIGHT 360, poses for a portrait at the medical clinic in San Francisco on March 9, 2022. HealthRIGHT 360 is a health care provider for lower-income and otherwise marginalized Californians. (Beth LaBerge/KQED)
Inside a 'hippie' clinic, health care was a right
The Haight Ashbury Free Medical Clinic opened its doors in 1967, committed to an ethos where health care was a right, not a privilege. Tens of thousands of flower children and teenage runaways were flocking to San Francisco to “drop out” of everyday society and experiment with drugs, sex and rock 'n' roll.
The clinic offered people who used drugs health care at a time when the city’s health department worried compassion would encourage the hippies to stay. It provided a safe space for people dealing with bad trips and heroin withdrawal and, later, for veterans returning from Vietnam with post-traumatic stress disorder.
Founder Dr. David Smith said it was illegal for physicians to treat people with substance use disorder with prescription drugs in the 1960s. Clinic volunteers were so worried police would shut the clinic down if people used drugs inside that the door was painted to read: "No dealing!/No holding drugs/No using drugs/No alcohol/No pets/Any of these can close the clinic/We Love You."
When the Summer of Love ended, many people went home, but generations of people searching for meaning stayed behind in San Francisco, where the hard drugs moved in and people’s health care needs overwhelmed the clinic.
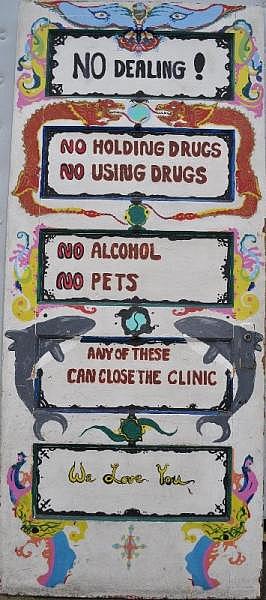
This painted door marked the entrance to the Haight Ashbury Free Medical Clinic. (Courtesy of David Smith archives)
“More than three years of life in the Haight, once the flower pot of America, now shattered into fragments of terror and despair, a ‘behavioral sink’ of pathologies feeding off the pill and the needle,” read a 1971 New York Times piece.
Still, the philosophy of the clinic — not only that health care is a right but also that addiction can be treated with medicine — persisted.
"It was harm reduction before there was such a term. It was never like, 'When are you going to get your shit together?' It was always, 'Hey, can I see what's going on?'" said Vitka Eisen, who was a patient at the Haight Ashbury Free Medical Clinic, as it was called in the 1980s.
The clinic smelled of patchouli, and a counselor walked around in a leather fringe jacket, Eisen recalled. She would go to the clinic before visiting her family in New York because she didn't want to be strung out on heroin when she went to see them. She’d pick up a “kick pack” of medicine to fight stomach cramping and nausea, and to help her sleep during withdrawal.
“After the seventh or eighth time, I was like, ‘I can’t do this anymore,’” she said.
She got treatment at Walden House, an addiction and mental health treatment program in San Francisco, and said she never used drugs again. Now she runs the treatment provider HealthRIGHT 360, the umbrella organization that includes what is known today as the Haight Ashbury Free Clinics.
'Carrying bleach was like having aspirin'
The philosophy of harm reduction spread internationally when activists and caregivers sought ways to reduce suffering and health risks during the AIDS crisis in the '80s. Volunteers handed out clean needles and encouraged cleaning needles with bleach.
Maia Szalavitz, the author of “Undoing Drugs: The Untold Story of Harm Reduction and the Future of Addiction,” says she was addicted to cocaine and heroin at the time. She was unaware that sharing needles put her at risk of contracting HIV until 1986, when she met Maureen Gammon with the San Francisco-based group Mid-City Consortium to Combat AIDS.
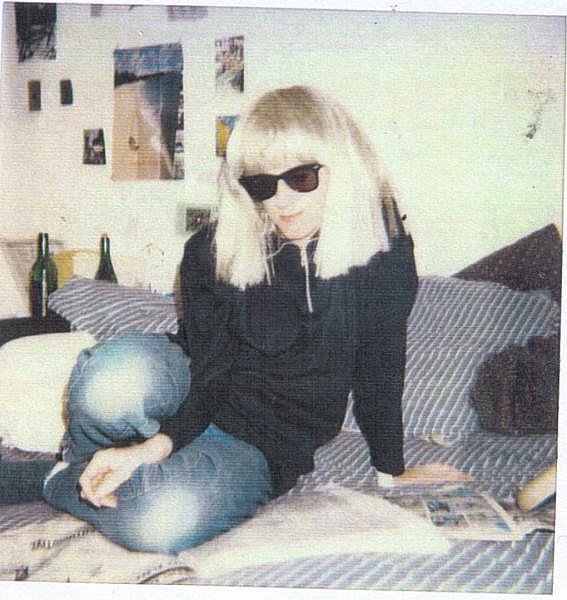
Maia Szalavitz, author of 'Undoing Drugs: The Untold Story of Harm Reduction and the Future of Addiction,' in the 1980s. (Courtesy of Maia Szalavitz)
“She told me I shouldn’t share, but if you have to share, clean the needle with bleach and then with water,” Szalavitz said. “Shooting up is a pretty compulsive thing, so I immediately incorporated this into my compulsive routine and she probably saved my life.”
Gammon said carrying bleach was as common as having aspirin.
“People just had [bleach], and it was not unusual to go into a corner store or taqueria or bar and ask for a bottle of beach and be able to get it,” Gammon said.
Inside the Ambassador Hotel
The AIDS crisis also forged a new generation of physicians, said Joshua Bamberger, an associate clinical professor of family and community medicine at UCSF.
He began his residency at San Francisco General Hospital in 1989, and said all his energy and focus went into caring for men who were dying of AIDS.
“Much of my work was really holding men in my arms as they died,” he said. “And as awful as that was, it also created an era of physicians and other healers who bonded over the important things in medicine, which isn’t necessarily slinging medication but providing love and care for people who are really suffering.”
Some hospices refused to take in people who had a history of drug use, or had clauses saying they’d only accept people on the condition they’d been sober for six months before being referred. But the people who needed to be referred often had two or three months left to live.
So, many people found refuge at the Ambassador Hotel, an SRO in the Tenderloin run by gay rights activist Hank Wilson beginning in 1978. It became one of the few places where AIDS patients who used drugs could live without having to die on the streets. In the 1996 documentary "Life and Death at the Ambassador Hotel," the site is described as a model in harm-reduction housing.
“The Ambassador was sort of a de facto AIDS hospital,” said Bamberger, who did rounds there, providing care alongside community members and friends of those dying. “When treatment options were limited, and [people] didn’t have a home, the Ambassador was a place where they could land.”
Val Robb, a nurse at the Ambassador Hotel, said she had to learn the culture of the people who stayed there. Many people who used drugs were distrustful of a health care system that considered them not worth treating.
"I started speaking the language more, which is, 'Let me work out a deal. You need me to do this. I want you to do that,'" Robb said. "I need you to go to the doctor. If you go to the doctor, if you let them examine you, then let's get you some codeine. It wasn't like, 'I'm Nurse Nancy doing this thing for you.'"
There were times Robb had to go against what she knew about health, such as offering guests cigarettes if they would let her examine them. But she said she still had to draw the line.
"Another guy, he says, 'Val, I'm trying to get high, and my partner couldn't hit the vein. Can't you?' I said, 'No, I'm a nurse with kids and a license, I can't do that,'" she recalled.
It took years before the city approved or funded some of the harm-reduction practices happening underground. The AIDS crisis hit its peak in San Francisco in 1992, and the following year Mayor Frank Jordan declared a state of emergency and announced that San Francisco would back a program to give clean needles to people who used drugs.
'Call it Lazarus in a hypodermic'
Meanwhile, naloxone, the medication used to reverse overdoses, was still only widely available in medical settings. Rachel McLean, the outreach worker, said she and others attended a conference on drug policy reform in 1999 where an Italian man gave a presentation on naloxone.
“None of us could even understand what he was saying because his accent was so strong. But we understood that he said that in Italy, community health workers give out naloxone on the street,” she said. “And all of us, our minds were just blown by that.”
At the conference, Dan Bigg with the Chicago Recovery Alliance brought a duffle bag full of naloxone.
“And people would just come and take it, and that's how underground naloxone started in San Francisco,” McLean said.
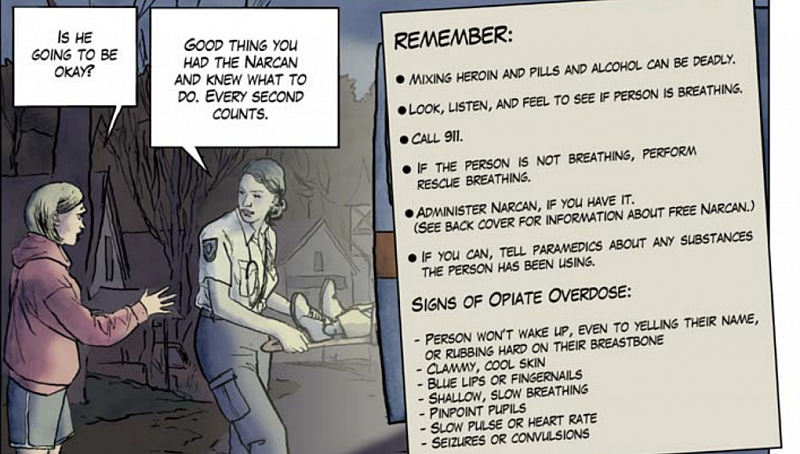
Naloxone education material used in San Francisco from the Massachusetts Department of Public Health. (Courtesy of Joshua Bamberger)
"It's a mission that's part Che Guevara, part Mother Teresa. The guerrillas aren't doctors. Nonphysicians, obviously, are barred by law from handing out prescription drugs — it's a felony that can carry up to 10 years in federal prison,” reads a 2003 article from A.C. Thompson in The San Francisco Bay Guardian on a visit to a San Francisco needle exchange site where volunteers were distributing naloxone.
Critics said providing people who used drugs with naloxone, more commonly known by the brand name Narcan, would encourage drug use. Clinicians worried about liability if people had an adverse reaction to the naloxone, or if they died even after naloxone was used.
While studying at San Francisco State University in the same year as the conference on drug policy reform, McLean was assigned to write a paper analyzing a public health problem. She drafted some ideas based on the knowledge she had absorbed from the community, and proposed opening safe injection rooms, testing drug supplies and training people who inject drugs in administering naloxone.
She presented the paper to members of a so-called “heroin subcommittee” created by the city to address overdose deaths, and members included the ideas in their final recommendations.
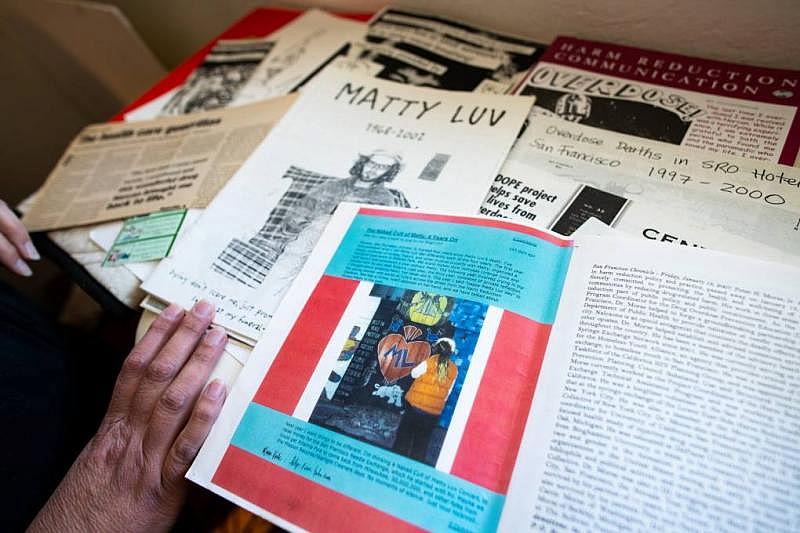
Rachel McLean looks through her archive of flyers, zines, educational information, and research on harm reduction at her home on March 10, 2022. A photo of friend and colleague Pete Morse can be seen, as can a zine about Matty Luv, singer of the San Francisco punk band Hickey, who passed away from a heroin overdose in 2002. (Beth LaBerge/KQED)
Soon after turning in her paper, McLean graduated from college, quit her job as an outreach worker and went to Mexico for three months, burned out by the trauma. But she would sometimes wake up at night to scribble notes about what an overdose prevention program would look like.
“The fire was still there,” she said.
Members of the heroin subcommittee ended up calling McLean. They remembered her recommendations from several years before and asked McLean if she would implement some of her ideas.
With a $30,000 annual budget, the Drug Overdose Prevention and Education (DOPE) Project began in a makeshift office in McLean’s kitchen in 2002. She started making phone calls to overdose prevention workers, and put together a curriculum to teach drug and alcohol treatment providers, sheriffs and deputies, the probation department, homeless shelter staff, and others how to reverse overdoses through rescue breathing. Without naloxone widely available, rescue breathing was something anyone could do to reverse overdoses, with some training.
Heroin overdose deaths plummet
Alex Kral, then a researcher with the Urban Health Study at UCSF, conducted a pilot study with other researchers in 2001 to 2002, training 24 people to use naloxone. There were 20 overdoses during the study. Trainees reversed all of them, 15 with naloxone, and most of those with an additional rescue method. The researchers presented the findings to the county’s public health director.
"We said, 'Look … you've got people dying of overdoses and you're not able to do anything about that,'" said Kral, who is now an epidemiologist with the nonprofit health research institute RTI International. "'Why don't you do something about it?' And [the director] said, 'Yeah, let's do it.'"
One year later, the San Francisco Department of Public Health partnered with the DOPE Project to distribute naloxone at syringe-exchange programs, SROs, reentry programs and other sites in the community.
Joshua Bamberger, who oversaw the program with San Francisco's DPH, said heroin overdose deaths dropped “unbelievably down,” plummeting from a peak of 155 in 1995 to 10 in 2010.

An altar includes a candle from a memorial for Pete Morse on the mantel of Rachel McLean's home on March 10, 2022. (Beth LaBerge/KQED)
“Nothing's gonna reduce death to the extent that getting 10,000 doses of naloxone out there in San Francisco in the early 2000s will ever do,” Bamberger said.
McLean, who now works for the state health department, still keeps a picture on her mantel of Pete Morse, who was at the forefront of bringing naloxone to the streets of San Francisco. He died of a drug overdose in 2007.
“I think about him all the time. I want to make sure that his contributions are remembered,” McLean said. “I don’t want to say that it broke my heart the most because I don’t want to compare it to all of the other deaths, but it’s still with me.”
The fentanyl overdose crisis
Naloxone has become a key tool in reducing overdose deaths nationwide. For years, it helped stave off the worst of the opioid crisis in San Francisco. But geography also helped for a time. On the West Coast, black tar heroin was the most common type of heroin, and that black color made it more difficult to hide white-powdered fentanyl inside.
Still, the number of people who injected drugs in San Francisco — mostly heroin — more than doubled early in this century, from 10,158 in 2005 to 22,000 in 2012.
By 2017, fentanyl had crept in to begin its rampage. That year, the city reported 36 deaths linked to fentanyl. That jumped to 90 in 2018. In 2020, the number of fentanyl-related deaths skyrocketed to 518.
An estimated 650 people overdosed and died in San Francisco last year, a spike driven by fentanyl, according to data from the San Francisco Medical Examiner’s Office.
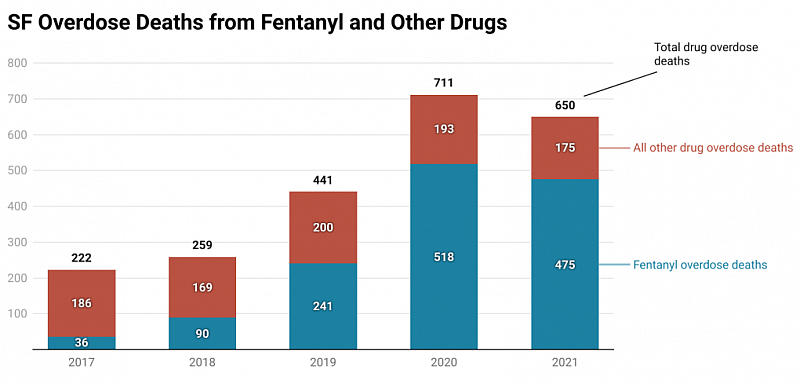
Data on fentanyl-related and non-fentanyl-related overdose deaths from the San Francisco Department of Public Health and San Francisco Medical Examiner's Office. (Chart by Matthew Green/KQED)
“I lost so many people to just fentanyl,” said Joel Webber, who goes by Turtle. He sat on a curb recently near Hotel Whitcomb, a city-run hotel on Market Street. People regularly gather nearby to use or sell drugs.
Webber said he received methadone treatment for 22 years, then started using fentanyl when he stopped his methadone treatment.
“If I could, I would blow up every f---ing fentanyl lab up with a button and end it. I’d get sick, but I’ll take it,” Webber said. “I just want it gone.”
Drugs like fentanyl are unlikely to disappear, and that means the city will need to try new strategies to prevent overdoses. A river of naloxone is not enough to confront the crisis, said Keith Humphreys, an addiction researcher at Stanford University School of Medicine.
One dose of naloxone often is not enough to reverse a fentanyl overdose.
“Maybe we can’t make fentanyl use safe,” he said. “Let’s say you make it twice as safe. It’s still just so deadly it just overwhelms the capacity of what we know how to do.”
Community and trauma in harm-reduction work
In 2021, President Joe Biden became the first president to make expanding harm reduction one of his drug-policy priorities. But people still argue that harm reduction encourages drug use. Several city leaders in San Francisco have criticized an overreliance on harm-reduction services and a lack of abstinence-based treatment options.

Kristen Marshall and the Dope Project team pose for a portrait during Overdose Awareness Day in 2020. The event gathers providers and community members to hold space for those lost and celebrate people still with them. (Courtesy of Kristen Marshall)
Kristen Marshall was the program manager for the DOPE Project until last winter.
"When you do this work, it's your life, even if you try to fight it. It's a lot of grief, it's a lot of pain, it's a lot of trauma. And that breaks a person down," she said. "It feels really hard for me as someone who is in this position when suddenly people are like, 'Well, this is your job. If overdose prevention is your job, what do you do? Harm reduction must not work.'"
Still, because of the vast supply of naloxone in the community, people are reversing more drug overdoses, many fentanyl-related, in San Francisco than ever before. The DOPE Project reported 81 overdose reversals in 2006. In the year 2021 alone, the group reported 8,985 reversals. Many of those overdoses were reversed by people who use drugs. In comparison, San Francisco police, who by then were carrying naloxone, reversed 144 overdoses in 2021.
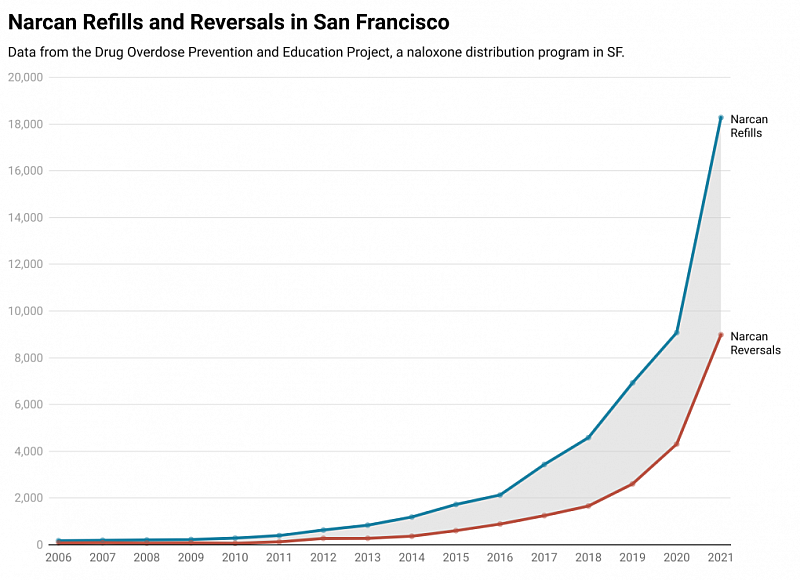
Reporting data from the Drug Overdose Prevention and Education Project, as documented in a San Francisco Department of Public Health report. (Chart by Matthew Green/KQED)
Marshall said the larger question she keeps asking herself is what happens after overdoses are reversed.
“So they go to treatment, then what? Where's their housing? So they go right back outside,” she said.
She believes overdose prevention efforts will inevitably fall short until root causes such as poverty, racism and isolation are addressed.
“We’re giving people Narcan and saying, ‘Live, live, live, live — you have to live,’” she said. “The question that I want to ask everyone is, ‘What are we living for? What is there for people to grasp?’”
This reporting was produced as a project for the USC Annenberg Center for Health Journalism's 2021 Data Fellowship. KQED's Kate Wolffe contributed to this story.


