How neglect and abuse change children’s brains — and their futures
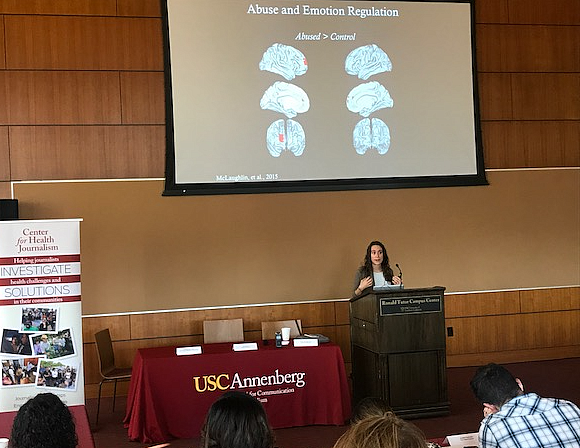
Katie McLaughlin, director of the Stress and Development Lab at the University of Washington, speaks to a room full of reporters.
Childhood adversity comes in different forms. When Katie McLaughlin, director of the Stress and Development Lab at the University of Washington, talks about stress and early childhood development, she brings up two different fictional children: One who faces the constant threat of violence at home, and one who is neglected.
“Not all adversity is created equal,” McLaughlin said. “Those two types of adversity impact the developing brain in distinct ways, and require different interventions.” She explained that around one in four mental health problems in adults can be explained by stresses in childhood. Stresses like poverty, neglect and abuse all manifest differently in the brain and can cause different mental health issues later in life.
Take the case of someone who grows up in a violent home. Studies show that 20 percent of children will be exposed to violence by the time they reach adulthood. Growing up in an environment characterized by danger influences a child’s ability to process threats. Seeing danger everywhere is an adaptive response, explains McLaughlin. “What the brain is doing is adapting to the environment it’s raised in,” she said. “But while the short term adaptations are useful, there are long term costs.”
McLaughlin’s work has shown that children exposed to violence tend to react more strongly to negative situations and have a harder time regulating these emotions. In an fMRI scanner, the brains of kids who are exposed to violence are more reactive — but only to a specific subset of images. “When there is something in the environment that could signal something dangerous, their brains are alarming at a high rate,” said McLaughlin.
And when those kids were asked to distance themselves emotionally from negative images, they were able to successfully do it — even though the scans showed their brains had to work harder than those of kids who hadn’t experienced adversity. This type of heightened response and the effort it takes to reset can make school more challenging and put these kids at risk of developing anxiety and PTSD.
The effects of a deprived environment for a young child — say, an institution or a home where there wasn’t healthy, regular stimulation — look different in the brain. “Our brain requires input from the environment to develop normally,” McLaughlin said. Visual input is required for visual development, and if there isn’t any visual input, those brain connections are eliminated — something called synaptic pruning.
Deprivation causes this synaptic pruning to go haywire. In the first two years of life, babies are building around 700 synapses per second — a rate never achieved again in life. But those synapses will get pruned if they’re not used. The overzealous pruning ultimately produces measurable reductions in cortical thickness and reduced grey matter in the brain, McLaughlin has found. That in turn raises children’s risk for ADHD and trouble with complex cognitive tasks.
McLaughlin says that neuroscience can do more than just shed light on the differences between types of childhood adversity. She points to trauma-focused cognitive behavioral therapy programs that can help kids modulate the strong brain response they have to threatening experiences. “Our findings suggest that teaching children these strategies could actually prevent the onset of problems with anxiety and PTSD later in life,” said McLaughlin.
Still, the researcher believes the problems of childhood adversity are best addressed with broader policy change. McLaughlin said:
“What we really should be doing is focusing on policies that alleviate poverty, promote access to high-quality child care, and prevent violence in our neighborhoods.”
**

