By his fourth week waiting for help in the emergency room, Zachary Chafos’s skin had turned pale white from lack of sun.
This article was produced as a project for the USC Annenberg Center for Health Journalism’s Data Fellowship.
Other stories include:

A photo of Zachary Chafos dressed as one of his favorite Pixar characters, Mr. Incredible, at his home in Clarksville, Md
(Matt McClain/The Washington Post)
They’d brought Zach to Howard County General Hospital on Nov. 12, 2020, amid a severe mental crisis. All his life, he’d been the joyful center of their family. But after months of pandemic isolation, Zach had become uncontrollably angry and begun physically assaulting his parents and his younger brothers.
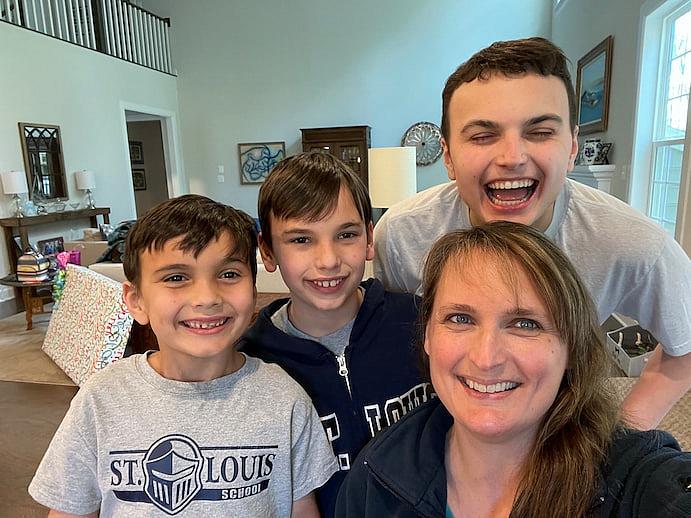
Zach with his mother Cheryl and his two younger brothers Christopher, 8 and Anthony, 12, on April 21, 2021 (Family photo) (Family photo)
Now he and his parents found themselves in medical purgatory, waiting for psychiatric treatment that never seemed to arrive. Every day, Zach’s case manager in the ER would call to see if a psychiatric bed had opened up. Every day, the answer was no.
In the state of Maryland, there are roughly 1,040 licensed psychiatric beds for adults in general and private hospitals and another 240 for children and teens. The majority are almost always full.
As a result, patients rushed to the emergency room often spend days or even weeks waiting for beds to open up in psychiatric hospitals and wards. The younger the patients are, and the more severe their cases, the fewer beds there are, and the longer they often wait.
The problem is a national one, with kids and teens from California to Maine languishing in ERs. Many are deeply depressed or suicidal — mental health issues that were already on the rise before the pandemic but have since reached unprecedented levels.
A children’s hospital in Colorado became so overloaded last year with psychiatric patients that it declared a state of emergency. A group representing more than 200 other children’s hospitals warned that the number of kids showing up in mental crisis has far outstripped resources.
But the situation is especially acute in Maryland, whose emergency rooms suffer from some of the country’s longest average wait times for those in need of psychiatric treatment.
For the past decade, Maryland officials have promised to address the problem. Yet the wait times have only lengthened during those years, especially among children and teens, a Washington Post analysis of statewide hospital records shows.
For Zach, everything about the ER made things worse. His autism meant he had little understanding of his surroundings, and his speech was mostly limited to one- or two-word sentences. The only place the hospital could house him during lengthy stays in 2020 and again in 2021 was a sunless room in the middle of an ER filled with the overwhelming sound of other patients in pain. Later, his parents would look back on those weeks, especially the final ones, with deep regret and guilt.
Amid the pandemic, his parents were allowed to visit Zach just once a day. He’d struggled with debilitating epileptic seizures since age 14, prompting his parents to measure his medication down to the milligram. In the ER, doctors changed his doses, Zach’s medical records show, and he had two massive seizures within his first several days there.
A spokeswoman for Howard County General said officials could not discuss the specifics of Zach’s case because of medical privacy rules. They also declined to talk about how emergency room wait times are affecting the hospital.
According to his parents, Zach was rarely allowed to leave his room, except to shower. An aide and a security guard were assigned to watch him around-the-clock, making sure he didn’t harm himself or others.
“It’s like he was in prison, except even hardened criminals get sunlight and exercise,” his mother Cheryl, 47, said.
Confused and frustrated, Zach lashed out at his nurses and doctors repeatedly. They tied down his arms and legs with restraints and injected him with a sedative called haloperidol, according to his medical records. The drug reduced his aggression but made his whole body shake so violently that he couldn’t hold a cup of water still enough to drink from it.
Zachary Chafos was given a sedative called Haloperidol and it made his whole body shake so violently that he struggled to hold a cup of water still. (Video: Courtesy of Chafos family)
“They were afraid to walk into his room, afraid to take his vitals,” said his father Tim, who sympathized with the hospital’s plight. “ERs just aren’t made to hold an autistic kid for weeks on end.”
But watching his son’s uncontrollable shaking reduced Tim — a retired Army colonel — to tears. He spent an entire Thanksgiving Day visit holding Zach’s hand, trying to help him regain control of his body.
“I wanted to give him my strength, to see if we could stop the shaking together,” he said. “But also I wanted him to know we hadn’t abandoned him.”

Cheryl Chafos and her husband, Tim Chafos were desperate to get help for Zach. (Matt McClain/The Washington Post)
The visits left Tim and Cheryl unable to sleep, debating late into the night whether to pull Zach out of the ER.
Their heated discussions, however, always ended the same. The hospital had warned them that the second their son left, he would lose his place in line for a psychiatric bed. The next time the family sought help, they would start all over again at the bottom of the list.
There was nothing the hospital could do. There was nothing Zach’s parents could do, except keep waiting for a bed.

An observation room used for patients that often have psychiatric issues at Greater Baltimore Medical Center. (Matt McClain/The Washington Post)
It took 28 days for the ER nurses to find a psychiatric bed for Zach.
Among patients who wait the longest, Zach was in the worst possible category: a teenager with mental health problems as well as neurological developmental delays.
Only one Maryland hospital — Sheppard Pratt, a renowned private facility in Towson — treats such patients in its neuropsychiatric unit. The unit is expensive to run, Sheppard officials said, requiring four times the number of staff as a standard psychiatric ward. There are eight beds for children and five for adults. They are in constant demand.
After being diagnosed and treated, the longest any patient should stay in the ER is four hours, according to a recommendation by the Joint Commission, a nonprofit organization in charge of hospital accreditation.
No one knows exactly how many mentally ill children and teens in America are left to linger in the ER. A recently published national sample of 88 pediatric hospitals found all but one regularly keeping some children overnight because they’re unable to transfer them to a psychiatric unit — a practice known as psychiatric boarding.
In Maryland, the proportion of psychiatric ER patients staying more than 24 hours has increased at an alarming rate in the past 10 years, The Post discovered by analyzing hundreds of thousands of discharges from the state’s emergency rooms. In 2010, just 1 percent of children 12 and younger with mental health problems stayed in the ER longer than a day. By 2020, more than 10 percent were getting stuck more than a day — and sometimes weeks. The percentage of teens ages 13 to 17 staying more than 24 hours also rose sharply, from less than 3 percent to more than 13 percent.
In 2019, 15-year-old Reina Chiang became one of them.

Reina Chiang and her mother, Kana Enomoto, pose for a portrait. Chiang has started a nonprofit to help others struggling with mental health issues. (Matt McClain/The Washington Post)
For weeks, the Bethesda teen had been hurting in ways she couldn’t control, feeling unwanted and totally alone. Finally, she told her therapist she wanted to die.
But her three days in the ER at Shady Grove Adventist Hospital only intensified those symptoms. “I just sat there day after day feeling even more alone,” said Reina, now 18, doing better and in college.
To keep her from harming herself, an orderly was assigned to watch Reina around-the-clock, accompanying her even on trips to the bathroom. When she slept, she was instructed to sleep with her body turned toward the orderly, so her face would be visible at all times.
Officials at the Adventist hospital said they could not discuss Reina’s case but acknowledged that ER wait times for teens in mental crisis is a growing problem.
For Reina’s mother, Kana Enomoto, the decision to take her to the emergency room was made in desperation. She’d tried calling to find a crisis center or mobile crisis team to help Reina.
“I thought for sure we’d get help. We live in Montgomery County, this progressive, well-off place full of resources,” Enomoto said. But the only centers she found open at the time were for adults.
Enomoto was aware of the system’s shortcomings. She’d worked her entire career to improve it. Just three years earlier, she’d been among the federal government’s highest-ranking officials in charge of mental health, leading the Substance Abuse and Mental Health Services Administration and overseeing its $4 billion budget.
Now, with her daughter in the ER, Enomoto felt helpless.
“I figured, I have great insurance. I have friends and connections everywhere in this world. But none of that helped,” Enomoto said. “The system is broken on many levels.”
ER doctors say the psychiatric cases they now grapple with daily are more frustrating than any car crash or gunshot wound because there’s so little they can do.
“It makes it hard to go into work, to be honest,” said Jeff Sternlicht, who has worked at Greater Baltimore Medical Center since 1998 and now runs its emergency department. “It’s caused so many of our nurses to quit. We all got into medicine to help people, not to deny them help.”
Since the 1960s, the number of psychiatric beds has been falling nationwide, part of a well-intentioned effort to move patients from state-run facilities and into community-based treatment programs. The problem is that those promised community resources never materialized, even as demand soared.
Roadblocks to mental health help only worsened the problem: denial by insurance companies; abysmally low reimbursement rates for providers; and growing shortages of psychiatrists, therapists and school counselors.
All of it has meant that people often don’t get treatment until they are in crisis.

Dr. Jeffrey P. Sternlicht remodeled the ER at Greater Baltimore Medical Center to better manage the flood of patients with psychiatric problems. (Matt McClain/The Washington Post)
At Sternlicht’s ER in Towson, psychiatric cases now take up so many beds that he’s had to physically remodel the space.
He expanded the locked area where violent mentally ill patients can be housed — equipped with heavy metal doors, 24-hour surveillance and panic buttons. He sectioned off another part of the ER for psychiatric patients with less-severe symptoms. He installed makeshift garage doors in several rooms, so that nurses can instantly lock away cords and flammable gas when dealing with suicidal patients.
He started hiring ER nurses specifically with psychiatric training in the hope they would be less likely to quit. His ER now employs full-time case workers whose only job is to dial psychiatric hospitals in the area nonstop so they can pounce on a bed the second it’s vacated.
None of it has been enough.
There are days when nearly every bed in his ER is filled with psychiatric patients awaiting transfer.
“People think it’s not their problem, but one of these days you’ll come to us with chest pains,” he warned, “and we just won’t have a bed for you because every single one has a psych patient in it.”
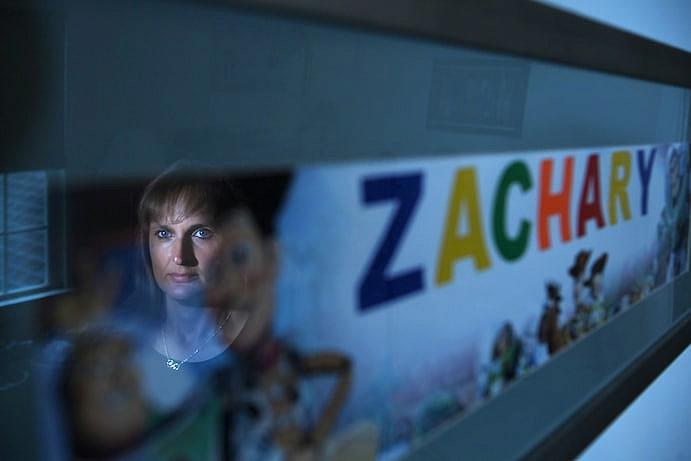
Cheryl Chafos is reflected in a framed photo in her son's bedroom. (Matt McClain/The Washington Post)
After finally being transferred to Sheppard Pratt, Zach Chafos stayed two weeks. He got intensive therapy and an adjustment to his medications. Once doctors and nurses stabilized his behavior, they sent him home to Clarksville.
His parents were thrilled at first to have him back under their roof.
Zach had always been a happy child. The second-oldest of four boys, he exuded joy even amid a life filled with treatment for his autism, seizures and intellectual disabilities.
As a teenager, he would spend hours bouncing on a trampoline in their basement and watching Pixar movies on a nonstop loop, shouting out his favorite characters’ lines.
Zachary Chafos sings along to one of his favorite songs from the movie "Toy Story" entitled “You’ve got a friend in me.” (Video: Courtesy of Chafos family)
But a few months after returning home, his manic mood swings and aggression suddenly returned worse than before.
“He’d bang on the door and the floor. He’d punch himself in the chest,” Cheryl said. Her son, who weighed 160 pounds but still had the mind of a child, was now hitting Cheryl so hard she regularly had bruises up and down her arm.
Worst of all, he started hitting his younger brothers. Cheryl and Tim would find their younger boys — then ages 7 and 11 — cowering at times and running to lock themselves in the bathroom.
Finally, on a late spring day in 2021 — six months after his lengthy ER stay — Zach flew into such a rage that Cheryl grabbed her two younger sons and ran barefoot outside.
She called Tim at his office. “I’m outside right now with the boys,” she said through tears. “I don’t know what to do.”
They had been researching group homes and long-term residential treatment centers that might take Zach, who’d turned 19. Exploring those options made them feel as though they were giving up as parents. But now, even if they could somehow get their insurance to approve, none of the long-term homes would be willing to take Zach while he was violently unstable.
That’s how, on June 28, 2021, Zach and his parents found themselves back at the one place they’d hoped to avoid: the ER at Howard County General.
They went in carrying a DVD player and stacks of empty notebooks for him to draw in. They brought Zach’s favorite plush toys, his favorite Pixar characters: Mr. Incredible, Woody and Buzz Lightyear.
Their plan was to get him into a psychiatric bed and stabilized again. Then try to transfer him into a long-term treatment center.
“We thought the wait couldn’t possibly be as long as last time,” Tim said.
They were wrong.

A hallway in the emergency department at Greater Baltimore Medical Center, which is often crowded with patients in mental crisis. (Matt McClain/The Washington Post)
A decade before Zach wound up in the ER again, several Maryland hospitals, including Howard County General, proposed a way to make finding a psychiatric bed dramatically easier: a statewide online bed registry.
Instead of ERs repeatedly dialing psychiatric units all day across the region, they could simply check an online dashboard showing in real-time which facilities had open beds.
But the 2011 attempt at a bed registry was short-lived — crushed by bureaucratic red tape, mistrust of state officials, lack of buy-in from hospitals and insufficient political and legislative backing.
More than 10 years later, Maryland’s ERs are still calling psychiatric units one by one and manually faxing patients’ charts to find a match.
In 2020, the Maryland legislature unanimously passed a bill requiring state health officials to create a real-time bed registry by the end of 2021. But it was vetoed by Republican Gov. Larry Hogan, who cited a lack of funds amid the pandemic. Lawmakers in the Democratically controlled General Assembly overrode the veto when they reconvened in February 2021. But then state health officials ordered a feasibility study that took months. The deadline — Dec. 1, 2021 — for having a registry in place came and went.
“It’s taken so long and been incredibly frustrating,” said State Del. Joseline A. Peña-Melnyk (D-Prince George’s), who sponsored the law. Peña-Melnyk began pushing for mental health reforms in 2019 after spending almost 24 hours in an ER with a constituent and her suicidal son waiting for a bed.
“I get calls and texts from families from the ER at all hours now,” she said, “and they’re heartbreaking.”
In an interview, Maryland Health Secretary Dennis R. Schrader rebutted criticism that state officials have been slow to act. “The notion that we haven’t been doing anything is ridiculous,” he said. “This is systemic. And we are coming at it from a systems perspective.”
He and state officials pointed to recent increases in state funding for the suicide prevention lifeline and efforts such as a $45 million Baltimore program to reduce unnecessary ER visits by expanding crisis response resources.
“These are major changes. Change doesn’t happen overnight,” Schrader said.
But solving psychiatric boarding, many studies say, will require major investments in more group homes and long-term residential treatment centers willing to take children and teens with particularly difficult-to-treat forms of mental illness, as well as mobile crisis programs that can stabilize adolescents where they live.
“We will never be able to create enough beds, especially if we have nowhere to put those patients afterward,” said Jeff Richardson, chief operating officer for Sheppard Pratt’s community-based behavioral health programs. “We have to invest in a better community-based system of care.”
Another urgent first step: creating a functional online bed registry.
State health officials predict it will take several million dollars, and many more months, to build the real-time system required by last year’s law. In the meantime, they have debuted a temporary pilot version, run by Sheppard Pratt, that gives a map of beds available by type and facility.
But several emergency rooms contacted by The Post earlier this year said they didn’t know the online portal existed. Those who did know said they found it unhelpful, because the portal relies on hospitals to voluntarily submit their information, and is updated only twice a day.
“The problem is there could be three beds open one minute, but by the time you try to transfer a patient, they’re all taken,” said Drew Pate, chief of psychiatry at LifeBridge Health and its five hospitals in the Baltimore area. Case workers at his ER are still calling daily to find beds. “It boggles my mind that we live in a society where I can order something with one click from Amazon, but I still can’t find out where open beds are for my patients.”
Schrader said the temporary bed registry is just a first iteration that state officials can learn from and build on. When told that many emergency room workers didn’t know the online registry existed, he said, “We’re trying to teach people how to use it.”
The day after his interview with The Post, Schrader sent a letter about the bed registry to every hospital in the state, requesting “that all hospitals ensure their discharge planners are aware of and use this vital resource.”
Weeks later, he convened a meeting with Peña-Melnyk and others involved in the bed registry effort and promised to meet with them every month until the end of the year, when the Hogan administration leaves office.
The latest estimate for when the new system will be fully ready, according to state officials: March 2024.

Cheryl Chafos visits Zach's grave at Arlington National Cemetery in June. (Matt McClain/The Washington Post)
During his second stay in the ER, Zach was surrounded by others in severe distress, his parents said. A 23-year-old depressed woman who screamed at all hours. A suicidal 25-year-old man who had gotten in a fight with his girlfriend and sat yelling in handcuffs.
Cheryl befriended another mother whose son was autistic and in crisis. The woman wore a bike helmet during her visits because of how often her son hit her.
After about two weeks, a nurse pulled Cheryl aside and suggested they stop coming to visit. Whenever Tim and Cheryl left the ER, she explained, their son would get agitated and sometimes violent. Stay away for a while, the nurse told her, and give Zach a chance to get into a routine.
“We basically just left him there,” Cheryl said. “It was brutal.”
For almost two decades, caring for Zach had consumed them both. When Tim retired from the U.S. Army after a 30-year military career, they chose to live in Clarksville because of the area’s robust services for people with autism. Cheryl had spent years shuttling Zach to appointments with neurologists and therapists.
Suddenly cut off from him, she lay in bed at night unable to sleep. Is he eating? Is he getting showered? Does he think we abandoned him? The thought of it upset her so much, she’d throw up some nights.
Zach’s 955-page medical file chronicles his days alone in the ER. The bright lights and loud noises often set him off. When enraged, he’d hit nurses in the face and grab their hair. It sometimes took as many as three ER staffers and four security workers to subdue him. They held him down, injected him with sedatives and closed his door to try to calm him down.
His inability to communicate frustrated both him and ER workers, according to their daily notes: “Patient has list of phrases from Pixar movies that he has memorized and repeats but no real ability to answer abstract questions.”
The one thought he was able to convey: “shouting and punching the wall in his room saying I want to go home.”

Cheryl Chafos is reflected in a mirror beside a photo of Zach. (Matt McClain/The Washington Post)
On her son’s 48th day in the ER, Cheryl got word that a bed had finally opened up at Sheppard Pratt’s neuropsychiatric unit. She rushed to the hospital to pack up Zach’s toys, DVD player and clothes.
When she arrived, her son looked markedly different. His uncut hair had grown curly and unruly. He had bags under his eyes and moved slowly, as if in a daze.
But when she went to hug him, he still hugged her back.
She thanked the ER staff for doing their best under difficult circumstances. “It was like we had all paid the price of admission,” she said. “Now he’d finally get the help he needed. Everything would be okay.”
But that final day in the ER would be the last time Cheryl saw her son alive.
Because of the pandemic, visits to the psychiatric hospital were difficult to arrange, with limited hours and advance notice required. Cheryl and Tim wound up talking to Zach twice in video calls.
Then, 10 days after Zach was admitted to Sheppard Pratt, Cheryl got another call. It was the doctor in charge of the neuropsychiatric unit. Zach, he told her, was dead.
Cheryl, who was at her youngest son’s soccer practice, stood on the field in shock. Tim was the one who drove them to the psychiatric hospital. As soon as Cheryl saw Zach’s body, she started screaming. Tim ran to his son and touched Zach’s face.
His eyes looked as if he were still half-asleep. But his lips were already turning purple. They’d learn later that Zach had died of an epileptic seizure, according to his death certificate.
Officials at Sheppard Pratt declined to discuss Zach’s case or death. His parents said they are still trying to understand the circumstances surrounding his fatal seizure.
But in the months since, they have struggled with feelings of guilt, second-guessing the choices they made and the long periods Zach spent in the ER.
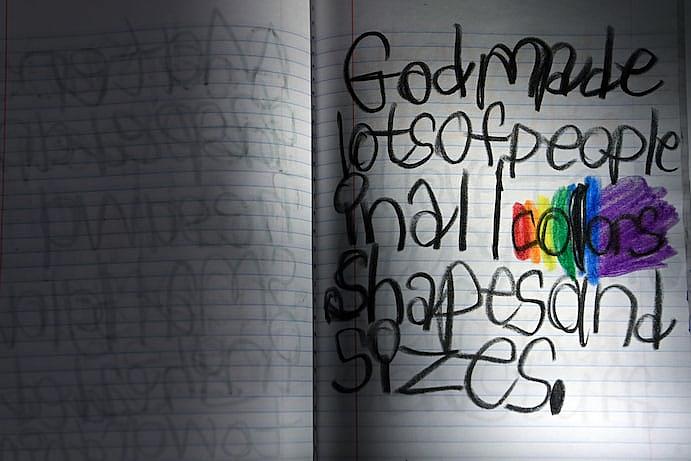
A note written by Zach, who often colored in the ER. (Matt McClain/The Washington Post)
“Those were the last days of his life. Trapped in a room with no sunlight, no fresh air, none of the people or things that he loved,” Cheryl said one night, as she and Tim sat on the floor of Zach’s room.
His favorite stuffed toys were scattered across the bed. Their backs still bore the initials — “ZC” — that hospital workers had scrawled in black marker to prevent Zach from losing them. Stacked nearby in the closet were hundreds of pages he’d colored to pass the time.
“Sometimes I think what if I had just put up with him hitting me,” Cheryl told Tim.
Her husband wiped tears from his eyes. “Sometimes,” he said, “I think what if I just listened to you and pulled him out of the ER.”
Their house is quiet these days. No walls being punched or arms being bruised. Their two younger children no longer live in fear of being hit.
But they would trade that peace to have Zach again. They would give anything for another chance to get him the help he needed.

Figures of Buzz Lightyear and Mr. Incredible adorn Zach's headstone at Arlington National Cemetery. (Matt McClain/The Washington Post)
Data analysis methodology
To quantify the length of psychiatric ER stays in Maryland, The Post obtained data on state ER visits between 2010 and 2020 from the Healthcare Cost & Utilization Project at AHRQ. The Post analysis focused on ER patients with a psychiatric condition as their primary diagnosis, using diagnostic codes identified by the Maryland Health Care Commission. The data set includes most patients who were awaiting a psychiatric bed but not those admitted to a psychiatric unit in the same hospital as the ER.
This article was produced with assistance from the USC Annenberg Center for Health Journalism’s Data Fellowship.
Story editing by Lynda Robinson. Photo editing by Mark Miller. Video editing by Amber Ferguson. Data editing by Meghan Hoyer. Copy editing by Susan Stanford.
[This article was originally published by The Washington Post.]
Did you like this story? Your support means a lot! Your tax-deductible donation will advance our mission of supporting journalism as a catalyst for change.