Born to die: Florida’s infant mortality crisis | A special report
The story was originally published by the South Florida Sun Sentinel with support from our 2023 Data Fellowship.

Tiffanie Williams holds framed photos of her stillborn son Liam, who died in 2016.
(Will Dickey/Contributor)
For 24 hours in a Jacksonville hospital, Tiffanie Williams clutched her son to her chest, stroking his face gently and singing him hymns.
Liam, only 10 ounces and 10 inches long, smaller than a water bottle, never met his mother’s gaze. He never squirmed or grasped his mother’s finger.
Williams could hear babies crying as she recovered from her delivery in the maternity ward.
Liam never cried.
Liam had visitors. His father. His aunts. His grandmother.
One of his visitors was a pastor who performed the rites of passage over Liam as Williams wiped away a continuous flow of tears. Liam, too premature to live outside the womb, never took a breath.
“I got to keep him and hold him all night,” said Williams, who cradled Liam’s limp body close in her hospital bed.
She was handed a pen. Then a death certificate. Her hand trembled as she signed it. Next came a list of funeral homes. She stared at it.
She handed Liam to a nurse and left the hospital with grief she never thought possible. Three days after his birth, Williams buried her son.
Each year in Florida, this “gut-wrenching heartbreak,” as WIlliams describes it, occurs hundreds of times: More than 1,300 babies a year, about four a day, die in Florida. In the early 2000s, the infant mortality rate was higher, but dropped slightly and then plateaued about a decade ago. Despite a declining birth rate, and millions of dollars spent by the state in the past 10 years on maternity programs, research, outreach and reports, the rate of infant mortality remains unchanged.
Why are Florida’s babies born to die? The state provides money, hospitals provide care, and healthcare groups provide support, but it all makes little difference for many mothers-to-be. The problem is getting worse — and Florida’s tightening restrictions on access to abortion raise the risk even more, with the increasing likelihood that unhealthy and disadvantaged mothers will have no choice but to give birth to children who might die in their first year or require long-term care.
Health experts say the losses of new life will continue unless the state rethinks how it fails mothers before and during pregnancy. The biggest risk to an infant’s health is always the mother’s health. When mothers have preexisting conditions, like diabetes, obesity or heart disease, their babies face a higher risk of death. Everything from Florida’s impenetrable insurance structure to its ineffective investment in maternal and prenatal health contributes to the high rate of babies who die within their first year of life, sometimes within their first minutes.
To understand why Florida babies are dying, the devastation those deaths leave behind, and the recommendations about how to keep more babies alive, the South Florida Sun Sentinel talked with more than four dozen doctors, mothers, midwives, nonprofit leaders, and researchers. The Sun Sentinel also reviewed state and federal birth and death records, Florida’s budget for maternal care, and the March of Dimes Report Card for Florida, among other sources of data.

Tiffanie Williams with framed photos of her stillborn son Liam, who died in 2016 at her home in Jacksonville.
(Will Dickey/Contributor)
Consider these findings:
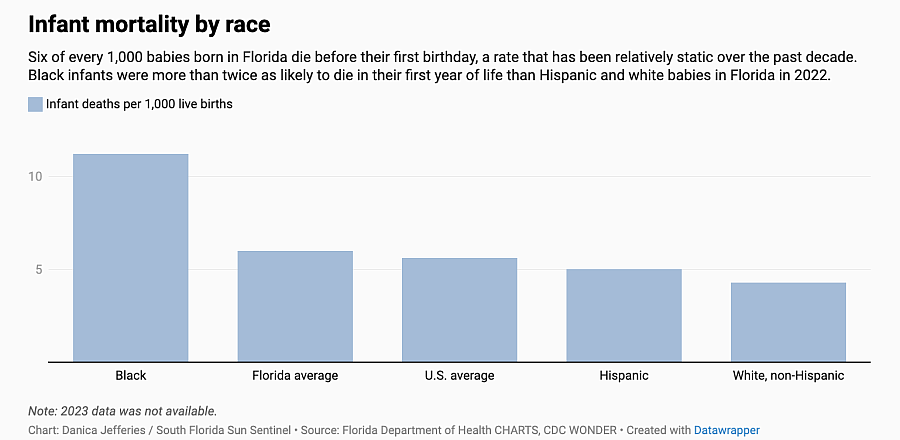
- Six of every 1,000 babies born in Florida die before their first birthday, a rate that exceeds the national average of 5.6.
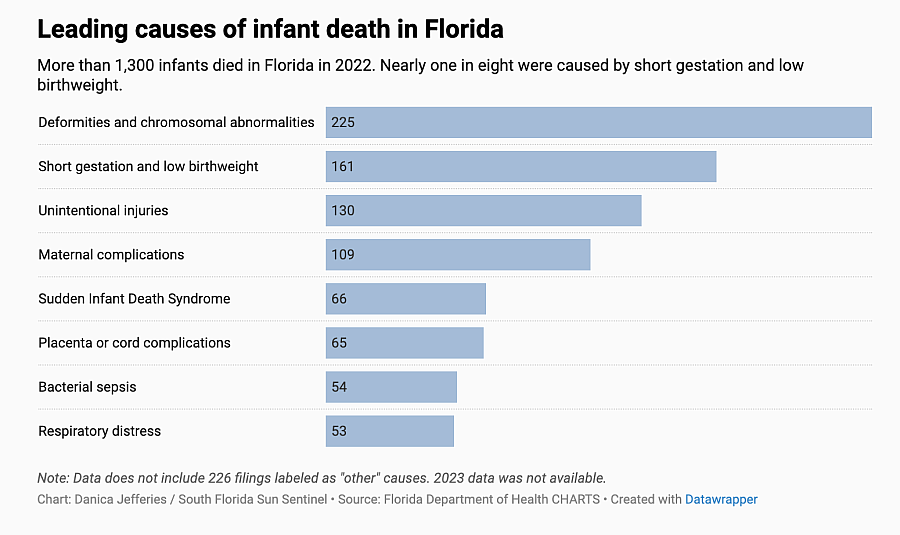
- Florida babies die mostly from birth defects that affect eating or breathing, infections prevalent in preterm and low birthweight babies, and Sudden Infant Death Syndrome.
- Most infants in Florida who die under the age of 1 die within their very first month.
- Black babies in Florida die twice as often as white non-Hispanic and Hispanic babies.
- Florida’s birth rate has been declining, making the unfluctuating infant death rate more significant.
- In some Florida counties, particularly those that are rural, the infant death rate is double digits and as much as three to four times the national average.
The cause of and solutions for infant mortality are complicated, but the call for action has never been louder.
“Think about the billions of dollars that they have spent along the way to end this scourge, and there isn’t any improvement,” said Jennie Joseph, founder of Common-sense Childbirth School of Midwifery. ”Somebody better figure it out.”
Jamarah Amani, executive director of Southern Birth Justice Network, says she sees why babies are dying each time she takes her mobile maternal healthcare van into the poorer black communities of Miami-Dade County. The women who are pregnant don’t have health insurance, don’t trust doctors, get ignored by doctors, or can’t get in to see a doctor.
“Too many women are not getting healthcare prior to pregnancy or in between pregnancies,” she said. “Many of the complications that occur during pregnancy are related to preexisting conditions that were not treated or are not being managed.”
In the United States, the infant mortality rate in 2022 soared to the largest single-year increase in two decades; Florida recorded 6.5% of all infant deaths in the country, slightly higher than its proportion of births, according to the birth and death data at the Centers for Disease Control and Prevention.
Researchers say the problem isn’t going away soon, but there are ways to address the causes and reduce risks.
“We just can’t keep letting this happen,” said Williams, whose son’s death at birth haunts her every day.
Where Florida is going wrong
In 2023, Florida commissioned its first comprehensive statewide look at infant mortality. The report shows the most common causes of infant deaths in Florida in 2022. They include congenital malformations such as spina bifida and neural tube defects; unintentional injuries like drowning or suffocation; disorders related to preterm birth or low birthweight; maternal complications of pregnancy; complications of placenta, cord and membrane; bacterial sepsis, an infection often contracted during labor; and Sudden Infant Death Syndrome, the death of a baby younger than 1 without a known cause.
To some degree, many of these are preventable, says Fort Lauderdale obstetrician Dr. Delisa Skeete Henry.
“More women need preconception care, earlier prenatal care and education,” she said. “They need to be educated on taking prenatal vitamins and folate, how to know the danger signs for preterm labor, and the proper care of a newborn.”
Compared to a decade ago, pregnant women in Florida are older, less healthy and have more complications during birth, according to Florida Department of Health maternal health records. They also are living in a state where access to insurance — or the right insurance — is a barrier to primary and prenatal care.
One of every three women of childbearing age in Florida has one or more chronic health conditions, according to the March of Dimes. A medical condition such as hypertension, diabetes, obesity or malnourishment nearly doubles a mother’s risk for a preterm birth or a stillbirth.
Florida’s pregnancy screening program reveals 63,000 mothers were obese at the time of pregnancy in 2022. The rate of women considered obese during pregnancy jumped 35% from a decade earlier.
“We have to get mothers to start their pregnancies healthier,” said Patrick Bernet, an associate professor of healthcare management at Florida Atlantic University who researches pregnancy outcomes and focuses on disparities. “Getting the mothers to start pregnancy healthier and in better situations in life is the best way to improve outcomes.”
Florida’s infant mortality rate of 6.0 has declined since the early 2000s when it was as high as 7.5 in 2003. However, it is inconsistent across the state, reaching into double digits in some counties, particularly those that are more rural.
In Northeast Florida, the infant death rate had become so high that community leaders, hospitals and health providers formed a committee to review each death. After studying every case in the region in 2018, the panel discovered there’s a huge gap by race — with Black infants dying at nearly three times the rate of white babies.
“Our analysis showed the maternal health of the mother was the driving factor,“ said Faye Johnson, CEO of Northeast Florida Healthy Start Coalition. “Until we improve that, we won’t see things turn around.”
Joseph, the Central Florida midwife, says focusing solely on the poor health of mothers won’t fix the problem. She says Florida’s healthcare structure needs to be examined and improved for more babies to live to see their first birthday.
“It is arrogant for the healthcare system to say this is a patient problem and not an ‘us’ problem,” said Tracey Wilkinson, an associate professor of Pediatrics and Obstetrics & Gynecology at Indiana University School of Medicine. “That is a lazy answer.”
Wilkinson says if Florida wants to improve its infant mortality rate, it needs to understand the fear and mistrust that prevent women from getting care when they are pregnant or thinking of becoming pregnant.
Women in Florida may be undocumented and fear deportation, may worry about a huge medical bill, or feel concerned that if they are bleeding, a doctor will accuse them of trying to self-abort, she said.
“When a pregnant woman is weighing the risks of getting care and believes not getting care is less risky than the alternative, then something needs to be done,” WIlkinson said.

Midwife Jamarah Amani, left, talks to Rebekah Antoine, 33, of North Miami Beach during a prenatal visit at the Southern Birth Justice Network in Miami. Antoine is pregnant with her fourth child.
(Carline Jean/South Florida Sun Sentinel)
Where Florida stands
Florida state health officials say they have prioritized the reduction of infant mortality for over a decade. The Department of Health has had some programs in place, such as safe sleep education and newborn screenings, and a state spokeswoman called attention to Gov. Ron DeSantis’ $95 million recent allocation for new initiatives.
For example, the state launched a Telehealth Minority Maternity Care Pilot Program in 2022 in two counties, Duval and Orange, to reach minority neighborhoods where maternity care is lacking and address health conditions that lead to poor outcomes. It expanded that program to 18 additional counties in 2023. During the 2024 Legislative Session, Senate President Kathleen Passidomo’s Live Healthy bill expanded this program statewide and allocated $23.4 million in the state’s annual budget that was approved this month.
“In fiscal year 2023-2024 this program has already served over 3,700 women with zero maternal or infant deaths among these clients,” said Weesam A. Khoury, deputy chief of staff with the Florida Department of Health.
Florida has a State Health Improvement Plan that sets priorities for maternity care to be accomplished by the end of 2026:
- Increase the percentage of very low birth-weight infants born in hospitals with Level III or higher neonatal intensive care units from 78.1% in 2020 to 86.3% in 2026.
- Reduce the average length of stay for hospitalized infants born to mothers with substance use by two days.
- Reduce the rate of congenital syphilis by 11 per 100,000 live births by 2026.
- Increase the percentage of maternity service hospitals with written breastfeeding policy to 100%.
The plan does not indicate how those goals will be achieved. None apply to prenatal health for mothers.
Another of the priorities in the plan is to reduce the Black infant mortality rate from 10.7 per 1,000 live births in 2020 to 9.6 per 1,000 live births. According to Khoury, provisional 2023 data reflects the target already has been exceeded with a rate of 9.3.
“Under Governor DeSantis’ leadership, this is the first time in a decade the rate has been below 10. This is a significant achievement,” she said.
But publicly available data shows that the rate of 10.7 in 2020 rose to 11.1 in 2021 and 11.2 in 2022. It is unclear when the official rate for 2023 will be released.
Where the problem starts
At the core of infant mortality in Florida is an insurance quagmire, say mothers, doctors and researchers.
Too many women aren’t seeing a doctor before they get pregnant or when they become pregnant because they lack health insurance, or the right kind of health insurance, they say. The result is mothers dying in childbirth or babies dying from deformities or conditions that may have been preventable.
One-fifth of Florida women ages 19 to 44 have no health insurance, which is worse than 46 other states.
When it comes to private insurance, Florida has one of the lowest rates in the U.S. of residents who are offered coverage through their employer, as well as those who actually take it, according to The Medical Expenditure Panel Survey — Insurance Component published by the US Census Bureau. And when Floridians do sign up, they opt for high-deductible plans and often forego care that requires out-of-pocket costs, the data shows.
At the same time, Florida is one of only 10 states where the Affordable Care Act’s expansion of Medicaid for low-income adults has not been implemented. That means thousands of women of child-bearing age can’t get Medicaid health insurance for primary care who would have coverage in expansion states like Virginia or New York.
Once an uninsured low-income woman becomes pregnant, she is eligible for full Medicaid coverage at no cost, but accessing that benefit is complicated.
“The woman has to understand the application process, who to call, how to fill out forms, and that takes time,” explained Dr. Mark Palazzolo, an obstetrician from Woman’s Health Centers in Central Florida. “Then the application has to go through processing, and now it’s getting later in the pregnancy and you have to find a physician who takes that insurance.”
The problem extends beyond just getting Medicaid coverage. Florida obstetricians say unless Florida raises its Medicaid reimbursement rate, giving pregnant women this coverage isn’t the answer.
Many obstetrical practices prioritize patients with private insurance over women on government-funded managed care plans that reimburse their services at low rates.
“A lot of practices in Florida refuse to take patients on Medicaid HMOs,” Palazzolo said. “So, access to care boils down to reimbursement problems. Patients are not getting access to the care they need — and the problems that creates are even worse for patients of color.”
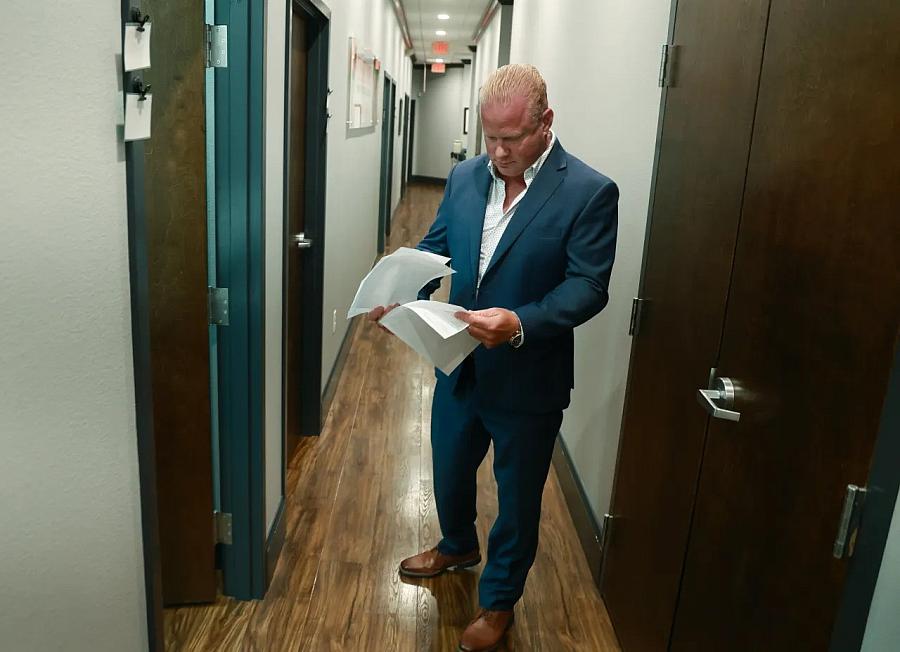
Dr. Mark Palazzolo, an obstetrician and gynecologist, looks through a patient’s information before entering an exam room at the Women’s Health Center in Kissimmee.
(Rich Pope/Orlando Sentinel)
At obstetric practices that do take Medicaid, the wait times for appointments often stretch weeks or months, creating delays that can have dangerous consequences. Medical conditions like gestational diabetes and high blood pressure, more common in Black women, often can be treated if detected early — but if not treated, can lead to maternal or infant death.
“There are some genetic defects we cannot change, but there are some — if we diagnose ahead of time — we can do preventative measures,” Palazzolo said.
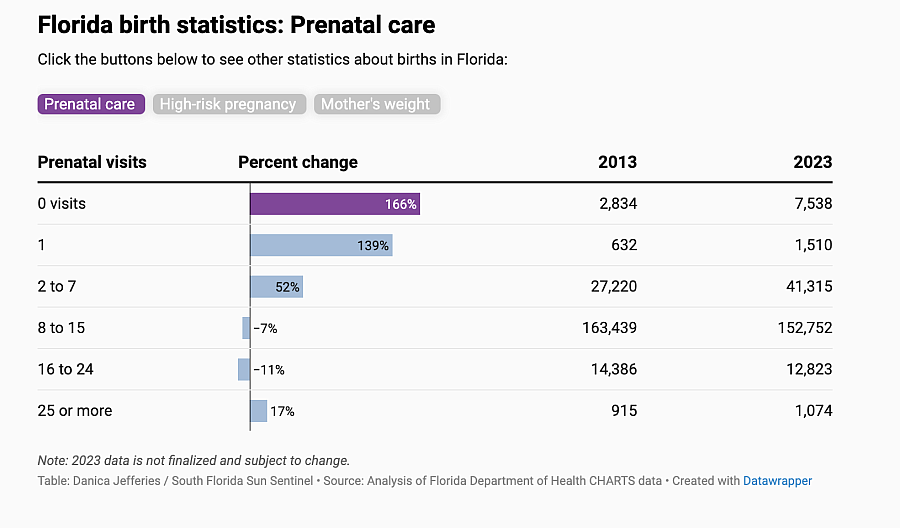
In the United States, experts recommend 13 to 14 prenatal visits with an obstetrician or a midwife, starting between weeks eight and 10 of pregnancy.
Yet for the last eight years, Florida has seen an annual increase in births to women with no prenatal care as well as an annual increase in women with high-risk pregnancies, according to data from the Florida Department of Health.
Inside hospital emergency departments, Florida doctors treat pregnant patients with pelvic pain, vaginal bleeding or other complications of pregnancy that could have been prevented with prenatal care.
“Prenatal care shouldn’t begin in the emergency department,” Palazzolo said.
Access to care getting worse
For moms in Florida’s rural communities, maternity care options have become more limited — and that puts mothers and their babies at risk of poor outcomes.
Florida has fewer obstetric providers than the national average: 138 per 10,000 births compared to the national average of 150 per 10,000 births.
“A young doc coming out of residency doesn’t want to be on call 24/7,” says Dr. Skeete Henry, who has been trying to add more obstetricians to her Fort Lauderdale practice.
Providers say the demand for obstetrics care may become even greater with new abortion restrictions in Florida. In 2022, Florida prohibited abortions after 15 weeks. Now, a six-week abortion ban is pending the outcome of a Florida Supreme Court decision on a challenge to the earlier 15-week ban.
Florida’s abortion records for 2022 and 2023 show the top reasons for the procedure are economic status, the psychological health of the mother, a medical condition of the mother, or a serious birth defect. All of those reasons contribute to infant deaths. If abortion is removed as an option, women in those situations may find themselves giving birth to babies who die.
As the need for care rises, hospitals have been increasingly scaling back or cutting maternity services for financial reasons. Maternity wards are often considered by hospitals to be “money losers” because of how reliant they are on payments from Medicaid, which reimburses at lower rates than commercial insurers.
The situation is particularly dire in rural counties. A January 2024 Center for Healthcare Quality and Payment Reform report reveals Florida has the highest percentage (86%) of rural hospitals without labor and delivery services in the entire country. This means those hospitals are outside of major metropolitan areas such as Miami, Jacksonville, Tallahassee or Orlando. The report says the median drivetime in rural areas to a hospital with labor and delivery services is 50 minutes.
From the western fringes of Palm Beach County to the northwest tip of the Panhandle, large swaths of Florida are labeled maternity-care deserts, meaning they are without a hospital or birth center offering obstetric care and/or obstetric providers.
Since 2019, at least 20 hospitals in Florida have closed their labor and delivery wards. The most recent closure, this month, was North Shore Medical Center in North Miami, which serves a population that is mostly Haitian and Black.
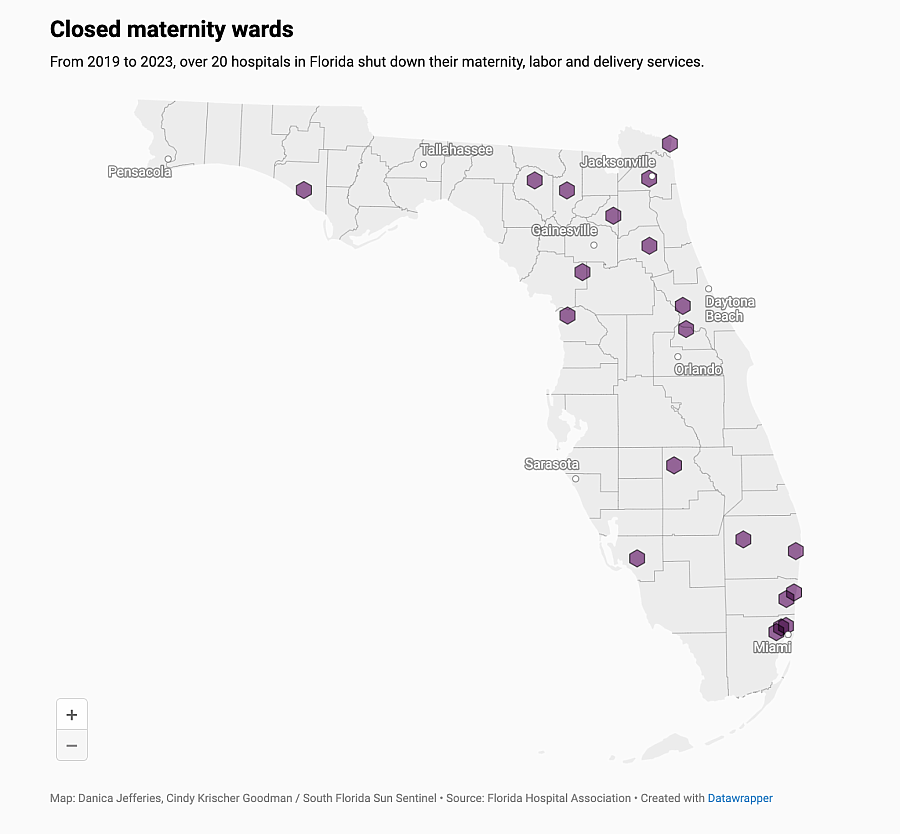
March of Dimes research shows that the farther a woman travels to receive maternity care during pregnancy, at the time of birth, and in emergencies, the greater the risk of poor outcomes for the mother and child.
“Every minute counts when a woman is pregnant,” said Caroline Valencia, director of maternal and infant health initiatives for March of Dimes in Florida. “Something can change quickly on the way to get emergency care.”
Valencia said she learned of a single mother on Florida’s West Coast who drove herself 45 minutes while in labor because the ambulance operators would not allow her to bring her young child with her. “I am sure she is not the only one who has done this. While these mothers are driving, there is so much that can go wrong,” Valencia said.

Midwife Jamarah Amani of the Southern Birth Justice Network in Miami says “Too many women are not getting healthcare prior to pregnancy or in between pregnancies. Many of the complications that occur during pregnancy are related to preexisting conditions that were not treated or are not being managed.”
(Carline Jean/South Florida Sun Sentinel)
Florida is not alone when it comes to labor and delivery department closures. Hospitals and healthcare districts across the nation are shutting down maternity wards, citing the decreasing numbers of births; staffing shortages; low reimbursement from Medicaid, the federal-state health insurance program for low-income people; and finances that no longer make sense.
A key factor in maternity ward closures is the decreasing number of births. In Florida, Department of Health records show the rate of births per 1,000 residents in 2022 decreased 6% from only five years earlier.
Lakeside Medical Center, a public hospital in western Palm Beach County, closed its labor and delivery ward in December 2022. The Belle Glade hospital says it closed the unit because of low volume. And nine months after Lakeside Medical’s birth unit closed, a mother in labor said she experienced the consequences.
Mariyah Boldin of Belle Glade was eight months’ pregnant when she felt sick and called 911, Towana Johnson, the baby’s grandmother, told a local news station. First responders took Boldin to the nearest hospital, Lakeside Medical Center. But when hospital workers saw she was pregnant, they rerouted her, Johnson said.
The ambulance raced her to the nearest hospital that does deliveries, Palms West in Loxahatchee, about 60 miles away.
After an emergency C-section, Boldin learned the baby’s umbilical cord had detached in the womb and her son had died. Johnson believes he could have lived if care was provided sooner.
Lea Pascotto, manager of supportive care for Avow Hospice, visits grieving families in West Florida. She has gone to homes to sit with mothers who delivered babies that never took a breath.
“Let me tell you, their grief is raw,” she said.
Pascotto says has seen how distance to a maternity ward can be a factor in outcomes. Immokalee in Collier County, for example, is a small rural, agricultural community.
“Those families don’t have a hospital. They have to come into Naples a good 45 minutes away. When looking at Florida, a lot of rural places don’t have hospitals, which is especially problematic for moms with high-risk pregnancies,” she said.
Previously, Pascotto worked as a chaplain at Naples Community Hospital, where she faced the human side of Florida’s high infant mortality rate. “There were instances when I went in and a mother just had a stillborn and she was clutching the lifeless baby to her chest. She would just be sitting there bawling.”
Consider this, she said: “The woman is going through hormonal changes of pregnancy, going through labor, but not having a baby afterward. It is supposed to be the happiest day of her life, and all of a sudden there’s a different life plan.”
Jenn Clayton, a registered nurse and founder of Cherryblossom Birth and Bereavement in Jacksonville, says the maternity ward closures are adding to infant deaths in poorer Black communities.
“Putnam County closed their only labor and delivery unit and that’s a problem,” Clayton said. “The county has the highest drug use in our state and highest rate of poverty in Florida. Basically, they took away access to care from families that have the highest risk of complications.”
Regardless of income or education, Black women lose more infants in the first year of life and have higher rates of preterm births and stillbirths. The disparity has medical professionals and Black mothers seeking solutions.
In 2022, the rate of fetal and infant deaths in Florida was similar for Hispanics and white non Hispanics, But for Black non-hispanics, the rate for both was more than double that of the other races.
Tiffanie Williams, the Jacksonville mother whose son died before birth, says the findings are a reflection of the medical racism, bias and barriers to health care that Black women endure. Too often, she says, doctors dismiss the concerns of Black women. But Black women die of pregnancy-related complications at two to three times the rate of white women regardless of their socio-economic status or education level, according to the CDC.
Williams, who has a doctorate in health sciences and works as a mental health counselor, said she knew something was wrong months before the stillbirth of her son Liam.
She had been battling severe nausea. Severe.
But when she told her doctor how ill she felt, the response was, “That’s just indicative of a strong pregnancy.” Williams, who battled weight issues most of her life but had worked to become fit before pregnancy, later discovered she had hyperemesis gravidarum, a condition in pregnancy in which she couldn’t keep down food. It causes vomiting, dehydration and can lead to preterm birth. At her final appointment before being hospitalized, she begged the doctor to listen: “I said I do not feel good. Y’all are gonna have to admit me. This is not okay. I feel like I’m about to die.”
On top of that, Williams’ cervix later weakened, a condition more common in Black women. She had it stitched closed to prevent a premature birth, but the stitch didn’t hold and her water broke, sending her into preterm labor.
“I am not saying if those doctors listened to me, my baby would be here. Situations happen, but I wonder if doctors listened more whether situations like mine would have been prevented,” Williams said.
Seven years later, Williams, 41, is a mother to 17-month-old twin boys. With her second pregnancy, she said, she found a specialist who used a different method to keep cervix closed during pregnancy. She also advocated early for medication for nausea.

Tiffanie Williams plays with her twin sons Levi, left, and Leighton, at their home in Jacksonville, Florida. Williams lost a child, Liam, in 2016, and with the pregnancy with her twins, she said, she used a doctor who paid more attention to monitoring her preexisting conditions.
(Will Dickey/Contributor)
Orlando attorney Jack Cook represents parents whose babies died for reasons he asserts were preventable. Too often in Florida, he says, the triage departments of hospitals are not prepared for the pregnancy-related emergencies they now face. Pregnant women who arrive at the emergency department with abnormalities are not being admitted.
“A lot of problems start right there at triage,” he said. “Why are they sending high-risk moms with issues home?”
Attorney Sean Domnick, a medical malpractice lawyer in Palm Beach Gardens, says healthcare providers play a role in the high infant mortality rates, too. Most no longer want to take high-risk patients, he said. “Their care decisions are dominated by dollars and cents. It pains me that this is their mindset. For people who profess a culture of ‘every life is valuable,’ they need to act like it.”
He also sees another contributing factor to infant deaths.
“What I see is incredible delays in nurses or midwives making the call to a doctor that needs to be made, and the baby suffers,” he said. “And then there are doctors who, when called in, won’t come to the bedside when they need to be there or they will be slow to react. During the pregnancy, we see doctors not identifying or adequately responding, and the baby dies in the womb.
“I have been doing this for 30 years, and the volume of cases we see is increasing,” he said.
Babies are dying before they are born
An increasing number of babies in Florida aren’t making it to birth.
Every year more than 1,500 pregnancies in Florida end in fetal deaths, with the top cause being complications of the placenta, cords and membranes, Florida Department of Health records show. These complications often cause a stillbirth, the death of an unborn child at 20 weeks or more.
Florida’s fetal death rate has exceeded infant mortality every year for the last 10 years. Stillbirths happen twice as often for Black mothers than for white non-Hispanic mothers and Hispanic mothers. A national study of stillbirths found that nearly one in four may be preventable. In Florida an organization called Count the Kicks advocates for making kick-counting a common practice for every Florida mother in the third trimester of pregnancy.
Bianca Castillo, 30, wants to see more education. She had a liver condition that put her at risk, but her doctor didn’t diagnose it.
In a Miami hospital, Castillo, 37 weeks’ pregnant, delivered her daughter Scarlett via C-section. She had chosen the name before she found out her daughter had died in her womb.
Castillo says she had been insisting to her obstetrician that something wasn’t right. Her blood pressure was high, and she felt itchy and fluish, but her doctor dismissed it as anxiety. Then it got worse.
“I drove myself to the hospital, and when I got there they ran tests and everyone got quiet,” she said. “There was no heartbeat.”
Initially, the doctor at the hospital induced her, but 36 hours later when she didn’t dilate, he did an emergency C-section.
Groggy and sedated, Castillo held her daughter’s tiny limp body.
“I felt numb. I didn’t even know such a thing as stillbirth existed.” she said. “There has to be some type of change in healthcare. Burying a baby is tough. Delivering a baby and not coming home with it is devastating.”
Castillo said the stillbirth was preventable. Three years later, Castillo has a healthy son. During this pregnancy she learned about the liver condition that predisposes her to preeclampsia, a dangerous hypertensive disorder that occurs during pregnancy.
“I had a specialist with my second pregnancy who listened to me and figured it out and gave me the medication to control it,” she said.

Midwife Jamarah Amani, left, comforts Ashly Hinds, 30, of Coconut Grove during a post-birth care visit at the Southern Birth Justice Network in Miami.
(Carline Jean/South Florida Sun Sentinel)
Where do we go from here?
Hospitals, health organizations, and state and city officials have mobilized in recent years to address Florida’s high rate of mothers and babies dying. They have focused on improving data collection and creating awareness campaigns that encourage medical professionals and others to listen when women say something doesn’t feel right.
In an October 2023 report to Florida Gov. Ron DeSantis, the president of the Senate and the speaker of the House of Representatives, the state’s Department of Health offered recommendations to improve fetal and infant mortality in Florida. It included actions such as improving safe-sleep education at local events, engaging local obstetric providers to complete online instructional training to improve prenatal risk screens, providing information to families about free services through Medicaid, getting more preconception health material distributed in Spanish, and creating more resource directories.
Williams, who launched the Liam Lives Foundation, says in her small way, she tries to do her part to help. Her foundation hosts infant loss support groups and provides financial support for funerals and memory boxes for families around the world.
Although time has passed, the hurt of losing Liam never goes away, she says.
“I think there is a fundamental disconnect, and there needs to be some more training or education or some other system put in place to make sure that providers are providing true culturally competent and trauma-informed care,” she said.
”Something needs to change.”


