Part 4: How can LA combat its fentanyl crisis? MacArthur Park offers clues
This project was originally published in Los Angeles Daily News with support from our 2023 California Health Equity Fellowship.

Jennifer Haid does outreach work in MacArthur Park in Los Angeles. She founded the nonprofit Humankind LA to help people struggling with homelessness and addiction.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
A walk through the alleyways around MacArthur Park reveals the harsh landscape of Los Angeles’s fentanyl epidemic.
People pass out with a burned piece of tin foil in one hand and a butane torch lighter in the other. Those who are awake often hunch over to cope with the bone-deep aches of withdrawals.

A man passes out in a Los Angeles alley near MacArthur Park after using fentanyl as others watch to make sure he was not overdosing.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
But a closer look also shows seeds of hope.
There are grassroots efforts working to connect people who use fentanyl with help. There’s a passionate young councilmember trying to launch an overdose prevention team and a harm reduction center offering resources to people who use drugs. There are public health professionals advocating for easier access to addiction-fighting medication.
“We are trying to saturate this area with life-affirming responses and services,” said Councilmember Eunisses Hernandez, who represents MacArthur Park, an area where, she says, overdoses are a daily occurrence.
Grassroots success
Jennifer Haid is a seed of hope.
She founded a one-woman nonprofit called Humankind LA in 2020 to help people experiencing homelessness around MacArthur Park access services and housing.
Haid has about 100 current clients, more than 90% of whom she estimates are addicted to fentanyl. There’s Alejandro, who is eager to get off the streets and off of fentanyl. There’s former client Richard, also known as “Finny,” who was homeless for around a decade and reports dramatically reducing his substance use since Haid helped him find housing this year.
“They are so strong and resilient,” she said. “I’m up all night thinking about them.”
Fentanyl is a highly addictive, synthetic opioid 50 times as potent as heroin. It was the primary contributor to the 55% uptick in the county’s homeless mortality rate from 2019 to 2021, according to the most-recent available data from the county’s Department of Public Health.
“We are trying to saturate this area with life-affirming responses and services.”
Los Angeles Councilmember Eunisses Hernandez
And MacArthur Park, near Downtown Los Angeles, has one of the highest concentrations of people who use fentanyl in L.A., said LAPD Sgt. Greg Fuqua.
Haid said her clients there face three primary challenges: isolation, hopelessness and addiction.
Her success hinges on her ability to stay in touch with people, convince them that change is possible and be there the moment they are ready to act.
“If somebody is deep inside a well, they have to know that what’s outside of the well is better than what’s inside,” she said. “If they don’t know that there is hope, there are people who care, there are options and there are choices, why would they do the work to get out of the well?”

Haid speaks with Alejandro near the Los Angeles alley by MacArthur Park that is known for fentanyl use. Haid is helping Alejandro register for housing.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
Haid starts small.
She dispenses a hug here, a word of encouragement there. She then moves to smaller tasks, such as connecting with a parent to get a birth certificate mailed and going to the DMV to get an ID, and using those documents to register a client for housing. After that, come big steps like matching the client’s housing voucher to an apartment unit or enrolling them in substance use treatment.
Addiction builds barriers
Fentanyl addiction can get in the way of all of this.
The drug’s “high” is relatively short and people who use frequently can start feeling withdrawal symptoms just two to three hours after smoking, said Ricky Bluthenthal, professor of public health sciences at USC. Therefore, many people are constantly chasing the substance.
“It’s an infuriating life; it’s definitely all-consuming, and you don’t have time for anything else,” said Richard, who was homeless for 10 years before Haid helped him find housing. “Setting the time aside to go meet with someone about housing is definitely not a priority. It’s nearly impossible when you’re dealing with addiction.”
For many people living around MacArthur Park, the pursuit of fentanyl begins first thing in the morning and can take several hours of shoplifting or panhandling to get enough money, Richard said. Shoplifted goods need to be resold to willing street vendors around the park. Then the money is used to buy drugs from a dealer — at which point, Richard said, exhaustion and withdrawals set in.
People living around MacArthur Park are vulnerable to theft and struggle to hold onto a phone, ID or other important documents. This makes it nearly impossible to register for housing or substance use treatment, and stay in contact with outreach workers.
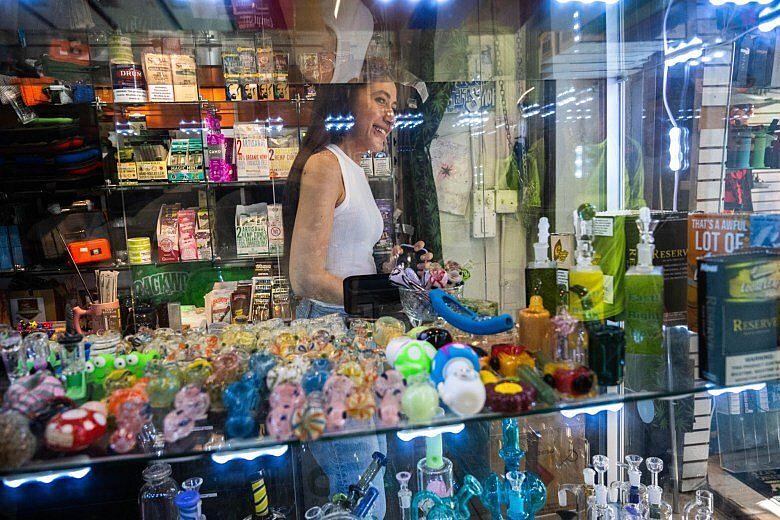
Lillian, co-owner of Mac Park Smokes on Alvarado Street, helps Haid by safely storing documents for Haid’s clients. She also allows them to use the store’s phone.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
Haid addresses this challenge through a partnership with a local smoke shop in MacArthur Park, where her clients can safely drop off their documents and use the store phone to contact her.
Using this approach, she has connected two people to residential substance use treatment, placed five people in permanent housing, put 25 people in touch with their parents and added about 50 to a housing waitlist. Another seven clients have matched with a housing voucher and Haid is working on finding them placements.
“It’s an infuriating life; it’s definitely all-consuming, and you don’t have time for anything else.”
Richard, who was formerly homeless
In September, Haid plans on opening a “homeless help desk” at a stand inside a MacArthur Park swap meet, where her clients can meet with her in a safe environment, fill out paper work, pick up supplies or simply rest for a moment.
Hernandez, the area councilmember, is also working on opening a “harm reduction center” by MacArthur Park that would offer sterile drug supplies, naloxone (a drug used to reverse opioid overdoses), a resting place, showers, food, clothes, injury care, and referrals to housing and substance use services. Her office is currently looking for both a lease and funding to launch the program.
“We are trying to keep people alive,” she said, “so that they have an opportunity to have the choice of getting into care or additional drug treatmen,”
Accessing treatment
For most people who use fentanyl, having stable housing is a prerequisite to decreasing use or entering treatment.
Alejandro, who is homeless in MacArthur Park, said fentanyl helps him survive on the street. It fights the cold of winter — and the heat of summer. It blunts the hunger. It tempers the depression, fear and pain.
Still, Alejandro said, he would like to stop using. But realistically, Alejandro said, he can’t see himself doing so until he’s free from the instability of life on the streets.
“There is no way I would have made it out here without drugs — no way,” he said.
Richard, meanwhile, said it’s been much easier to cut back on his use since getting housing in January.
“So much of my use was a survival mechanism,” he said. “Opiates are an extraordinary painkiller, for both physical and emotional pain, and I had it in droves because I was ashamed of myself, where I’d gotten to and what I’d become.”
Treatment for fentanyl use disorder, meanwhile, is similar to that for other opioids — but harder.
It typically begins with a medically supervised detox, followed by residential care and then outpatient care.

Matthew, 30, who uses fentanyl in an alley near MacArthur Park says he first got hooked on oxycodone at his Pennsylvania high school.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
“Once you’re on (methadone), you’re tethered to this place by an invisible chain. If you get too far away, you’re not going to make it the next day for your dose.”
Samuel Goslin, who uses methadone
Medication is essential to blunt pain and curb cravings during fentanyl detox, the week-long period after use ceases and withdrawal symptoms peak.
But administering it effectively is challenging.
Medication: key, but risky
Buprenorphine, for example, is commonly used during opioid detoxing and must be administered after the opioid has left a person’s system. Given too soon, buprenorphine can cause a rapid and intense onset of withdrawal symptoms, a phenomenon called “precipitated withdrawals.” But given too late, people will feel the full pain of natural withdrawals.
“With heroin, it was like clockwork; we could estimate when it would be out of the system and when we would not induce precipitated withdrawal,” said Heather Black-Coyne, chief clinical officer at New Directions for Women, a substance use treatment center in Costa Mesa. “Fentanyl is much more unpredictable.”
With fentanyl, she added, “it’s like Russian roulette.”
About one in five fentanyl patients, in fact, experience precipitated withdrawals during detox, Black-Coyne said. And when they do, they almost always leave the center and abandon their treatment plan.
“It doesn’t matter where their motivation was before,” said Rachel Rosenbaum, nursing supervisor at New Directions for Women. “They might truly want to be sober more than anything, but when your body and your mind is going through that immense pain, it is extremely difficult to convince yourself you should stay put.”
Another medication used to help people overcome fentanyl addiction is methadone, which doesn’t run the risk of precipitated withdrawals during detox, but is harder to access under current regulations.
It’s hard for rehab centers to get licensed to prescribe methadone, Black-Coyne said, so the medication is mostly used to help people stave off cravings after leaving residential treatment.
People are typically only given one dose of methadone at a time and must visit a clinic daily to pick it up.
“(Treating) fentanyl is much more unpredictable. It’s like Russian roulette.”
Heather Black-Coyne

Ralph enters the BAART Beverly Methadone Clinic by MacArthur Park for his daily dose of methadone. Methadone is used to treat opioid addiction including fentanyl.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
Joseph Friedman, drug researcher at UCLA’s David Geffen School of Medicine, is an advocate for changing regulations to make the medication more accessible.
Methadone, he said, is sometimes referred to as “liquid handcuffs.”
“People compare being on methadone to half of being in prison, because every single day you have to show up and wait in the line and people are not always nice to you,” he said. “It’s forcing you to interact with what often feels like a hostile institution on a daily basis.”
Solomon Goslin has been picking up methadone daily from the clinic in MacArthur Park for several years.
While the drug has helped him cope with chronic pain and opioid cravings, it also draws him back daily to a neighborhood with a high concentration of dealers and street drugs.

Solomon and Isis leave BAART Beverly Methadone Clinic after picking up their daily dose of methadone.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
“Once you’re on this stuff, you’re tethered to this place by an invisible chain,” he said. “If you get too far away, you’re not going to make it the next day for your dose.”
Methadone is heavily restricted because it’s an opioid and carries the risk of abuse and overdose. Those risks, however, are significantly less than those posed by more powerful opioids like fentanyl or heroin.
“Methadone is way safer than fentanyl,” said Bluthenthal, the USC professor. “Once someone has been established to have opiate use disorder, we should be making it ridiculously easy for them to get methadone.”
Less judgment, more love
Currently, the majority of people addicted to any substance, fentanyl included, do not get any treatment at all.
Of the estimated 40.1 million Americans with a substance use disorder, about 4 million – less than 10% – received any form of treatment in 2020, according to a survey by the federal Substance Abuse and Mental Health Services Administration.
“That means we’re not offering the right kinds of services,” UCLA drug researcher Friedman said, “because in reality, having a substance use disorder is not a fun event.”
Part of the resistance to seeking substance use treatment stems from the fact that medical settings can be unwelcoming environments for people with addiction, he added.
“There isn’t a place that we can pull up to and they go, ‘Come on in and we’ll take care of you’,” said Kevin, who was homeless for nine years before Haid helped him find housing. “Mostly, they kind of shun you. Hospitals will pick on you and go, ‘Oh, you’re a fentanyl user,’ and they’re just really rude.”
Dr. Gary Tsai, director of substance use prevention and control for LA County’s public health department, said there needs to be more non-judgmental spaces for people who use drugs to interact with medical services.
Councilmember Hernandez’s proposed harm reduction center is one example of this. Mobile medical vans, which bring health care directly to people experiencing homelessness, are another — and already periodically visit the MacArthur Park area.
Hernandez, for her part, is also currently seeking funding to launch a mobile team of medical professionals to stop overdoses in and around MacArthur Park.
“The most important thing is that you’re conveying a message that no matter where you are in terms of use or your recovery, our doors are open.”
Dr. Gary Tsai, with the LA County Department of Public Health

Dr. Adrian Mayo, of UCLA Health Homeless Healthcare Collaborative, checks the health of a homeless man at Casa Milagrosa’s community day resource center in the MacArthur Park neighborhood of Los Angeles.
Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG
All of these programs seek to provide compassionate care for people using drugs, and aim to increase the odds that they seek out substance use treatment in the future.
“The most important thing,” Tsai said, “is that you’re conveying a message that no matter where you are in terms of use or your recovery, our doors are open.”
Richard, the man who was homeless for a decade and still struggles with substance use at times, echoed that.
“One of the first things that happens to the addict is you lose family, friends and the feeling that you have people around you that love you,” he said. “It has always been the policy of the government to call you bad, call you wrong.
“I think we need more of a love-oriented approach.”


