How U.S. hospitals are defending themselves against the next big outbreak (Part 2)
Anna Almendrala’s reporting on Ebola’s impact on the U.S. was undertaken as a 2015 California Health Journalism Fellow at the University of Southern California's Annenberg School of Journalism. This is the second in a three-part series about the different ways the global Ebola outbreak has changed the United States.
Other stories in the series include:
If Ebola hits again, this state is doing everything right (Part 1)

Nurse Jody Walsh holds a bag of empty vials during a University of Minnesota Medical Center's Ebola preparedness drill on June 25, 2015.
MINNEAPOLIS — The patient was a toddler with a temperature of 105 degrees. About a week after returning from a vacation, he was coughing, vomiting and had diarrhea. His illness could have been any number of things: the common cold, the flu, or just plain exhaustion. At this time last year, Michelle Warren, the triage nurse answering the phone at the general pediatrics clinic of Children's Hospitals and Clinics of Minnesota, would have asked his mom to make an appointment at any one of the doctor’s offices in the network.
But because it was June 2015, one year after over 11,000 people died in an Ebola outbreak, she knew to ask one more crucial question: Did the family do any international travel recently? It turns out, they had — to a country on the Arabian peninsula, an area that has seen over 1,000 cases of the highly lethal Middle East Respiratory Syndrome since 2012.
Warren switched gears. Instead of asking the mother to go to her nearest clinic, Warren instructed her to meet staff outside the emergency room of the hospital’s main Minneapolis campus. Nurses met mother and son at the door, then led them straight to an isolation room with negative airflow -- a ventilation technique that prevents airborne cross-contamination between rooms -- to begin testing. There, a doctor wearing a hood, gown and gloves assessed the child, and a similarly dressed technician evaluated the boy with a portable X-ray machine in order to avoid potentially exposing more children to the disease.
It sounds dramatic, but this is what’s necessary for a cutting-edge hospital in a post-Ebola world, said Patsy Stinchfield, the hospital's director of pediatric infectious disease. And it demonstrates some of the many ways the Ebola outbreak of 2014 has dramatically changed hospitals and clinics across the U.S. Some hospitals, like CHCM's parent healthcare system, have evolved to become part of an elite, government-designated group of facilities trained and funded to safely assess Ebola patients. But experts across the country say that, even unofficially, protocols have changed everywhere else, too, and for the better. But will it be enough when the next pandemic hits?
While only a handful of Americans ever contracted Ebola, perhaps the most crucial lesson the country learned was that not all U.S. hospitals could effectively admit and treat a patient with a severe, highly infectious disease like Ebola. In response, the U.S. Department of Health and Human Services created a tiered national approach to Ebola care, appointing one hospital per region to specialize in highly infectious pathogens. Others were designated as assessment centers, capable of caring for a patient until a diagnosis is confirmed and the patient is transported to the regional hub.
But there are limitations to the new approach. Critics say there's a lack of basic training for all the hospitals that aren’t on the specialized care list, a problem because sick people initially go to the hospitals that are closest to them. And while the Centers for Disease Control and Prevention has issued new guidelines for these so-called “frontline facilities,” or hospitals that may one day have an Ebola patient walk through the door, the guidelines are unfunded and unenforceable because the CDC is not a regulatory agency. Even more troubling is that because of how difficult it is to prepare to become a regional Ebola center, some major areas of the country -- including the whole of California, the most populous state in the nation -- are left unrepresented in the network.
The Minnesota case
Staff at CHCM knew exactly what to do next if the toddler tested positive for MERS. They'd transport him 2.1 miles away to University of Minnesota Medical Center, which had just been designated as the Midwest region’s hospital for treating Ebola and other special pathogens.
There, he would be wheeled through a rear hospital hallway and moved via restricted elevator to UMMC’s brand new infectious disease ward, which sits gleaming and protected behind two different sets of badge entry systems.
Then hospital staff who have completed scores of drills on contagious virus protocol would don their MERS-specific protective gear and transfer the patient to one of their negative air pressure rooms, six feet away from a lab set up solely for this isolation ward. In his wake, a specially trained custodial team would deep clean the path the boy had taken from the rear entrance through the hallways, up the elevator to the ward.
It’s a far cry from what the response would have been almost a year ago, said Laura Reed, chief nurse executive for University of Minnesota Health. She still remembers the day she realized that the system wasn't ready for Ebola. Her heart sank on October 14 as she saw the news about Nina Pham, a nurse in Dallas who had contracted Ebola from her patient, a Liberian man named Thomas Eric Duncan who had recently flown to Texas from West Africa. Reed quickly went to her colleague, Deb Cathcart, vice president for patient care, to set up an incident command center for the hospital.
“I said, ‘You know what? This feels very different,'” said Reed, a soft-spoken woman with more than 35 years of nursing experience.
"This could have been any one of us,” Cathcart added.
Reed and Cathcart realized that if they were going to invest millions of un-budgeted hospital funds in preparedness, it would have to be for all exotic, deadly pathogens -- not just Ebola. “There are scarier and scarier bugs that we need to be aware of,” said Reed. "And it can’t be because of a crisis; This needs to be something that we’re prepared for.”
Reed, Cathcart, and hospital administrators moved forward on preparations before they knew they would be federally reimbursed, in part because of their mission-driven status as a public land-grant institution (a university given federally-controlled land to raise money), and also because Minnesota's Hennepin County, where the hospital is located, is home to one of the biggest Liberian populations in the U.S.
“It’s a huge financial investment for us, some of which we recouped from federal dollars,” said Reed. “But those dollars weren’t there when we made the decision to invest."
In October, a few weeks after Duncan was hospitalized in Dallas, University of Minnesota Health staff added the travel screening question to all of their electronic health records. They beefed up staffing levels so that they would be ready to take an Ebola patient at a moment’s notice. They relocated six beds from a little-used intensive care ward and began retrofitting it for use as isolation rooms, supply rooms and a dedicated lab.
Two months later, HHS announced a new network of hospitals that they had visited and deemed ready to care for Ebola patients. UMMC was one of the 55 hospitals to receive a minimum of $500,000 in reimbursements for the lengths they had gone to prepare.
But as the CDC studied the immense costs borne by the handful of U.S. hospitals that had successfully treated Ebola patients, the federal government realized a more specialized network was required. Nine regional medical centers out of a planned 10 were selected for funding to treat not only Ebola, but all other dangerous and exotic pathogens.
In June 2015, Minnesota beat out Illinois to represent the Midwest region in this new national approach to Ebola. As a member hospital, UMMC was required to be able to treat at least two Ebola patients, have negative airflow pressure systems installed in at least ten rooms, hold staff trainings at least once a quarter and be able to handle and dispose of Ebola-contaminated waste.
Big funding, big responsibility
With new responsibilities came even bigger grants: $2.25 million for the first year to cover the cost of the construction and personal protective equipment, and then $250,000 annually for the next four years. Most of the funding is to keep staff levels as high as they need to be in order to take a patient within eight hours.
"We’re not even expecting to break even, to be honest,” said Reed; it cost UMMC millions to create their special pathogens ward. But that’s how the regional approach is supposed to work: Funding and training for important but unusual conditions is concentrated where it can do the most good. It’s unrealistic and unnecessary to expect all hospitals — even major centers located in densely populated urban areas — to make these same investments, she said.
“You don’t want everyone to have to achieve this level of excellence either, because then you would have to disperse the materials, knowledge and the intensity of training,” she said.
But what happens when someone with Ebola or MERS walks into a clinic or hospital that isn’t in either of the tiered networks? That's what Jean Ross asks as president of the Minnesota Nurses Association, a union that represents over 20,000 nurses across the Midwest. Unlike treating a gunshot wound or a horrific burn, admitting a patient with Ebola -- even if they were to be transferred immediately -- puts untrained administrative staff, nurses and doctors at tremendous risk.
“We’re banking on these centers of excellence, and that’s not enough,” said Ross. “You need a single standard and it should be the best.”
The issue is critical, Ross explained, because for all the changes U.S. hospitals have made because of the Ebola threat, the outbreak didn’t change the fundamental structure of the American emergency room. They’re crowded, and have a triage system that prioritizes the worst injuries and illnesses over things that may, at first glance, seem like just a little cough or a simple case of traveler’s diarrhea.
'A lot of politics comes into play'
Melissa Harvey of HHS acknowledges the limits of the program. One alarming aspect of the preparedness model is that Region 9, which encompasses California, Nevada, Arizona and Hawaii, has no regional center for Ebola and special pathogens. None of these states applied, Harvey explained, and the reasons could be political.
(Image: NIEER 2013 Yearbook)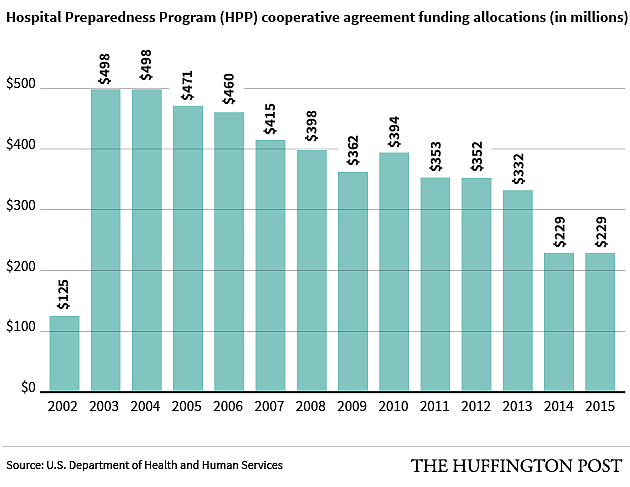
“We saw especially with Ebola, and we probably anticipate with other highly infectious diseases, that a lot of politics come into play,” she said. For instance, she explained, a medical center might be prepared to take a MERS or Ebola patient, but the governor of that state may block his or her travel across state lines. “In many cases there are laws that have to be looked at and reexamined, and it’s not as simple as getting a facility willing to do it."
Secondly, hospital regulation is handled on the state level. While HHS had always encouraged a core set of emergency preparedness and safety capabilities, there is often no way of knowing for sure what hospitals are doing to prepare for new and unknown infectious diseases, Harvey explained.
To make matters worse, federal funding for emergency preparedness in hospitals keeps getting smaller and smaller. Called the Hospital Preparedness Program, these federal grants have been awarded since 2002 to health departments and community health coalitions to enhance their response to public health emergencies. It has been steadily decreasing since 2003, when $498 million was awarded. In 2015, that was down to $229 million.
“[We] would have hoped that [HPP] worked for Ebola, but with limited preparedness funding, both state departments of health and the hospitals have to prioritize what they’re really going to spend that money on,” Harvey said. “And there’s simply just not enough to go around.”
Similarly, funding via the Public Health Emergency Preparedness cooperative agreement, which HHS has granted to state public health departments since 2001 to help prepare for infectious disease, natural disaster and “chemical, nuclear and radiological events,” went from a high of $1 billion in 2003, in reaction to the September 11 attacks and anthrax threats, to a projected $643 million in 2016.
‘That's always our downfall'
Ross is frustrated with the argument that there are a limited amount of resources to help hospitals prepare for the worst. She says that leaving preparedness to only the “official” Ebola hospitals risks the lives of countless nurses and other first-line workers, recreating the conditions that put nurses Nina Pham and Amber Vinson in danger.
After caring for Duncan, Pham and Vinson contracted Ebola from him and almost died. Pham is now suing Texas Health Resources, the parent company of Texas Health Presbyterian Hospital, for failing to provide adequate protective supplies and training to nurses.
“You start out with what you want to do and then you look for where the money is,” Ross said. “You don’t start out with, ‘We’ll try to do the best we can with what we think we can afford.' That’s always our downfall."
But hospitals and health clinics who aren’t part of HHS’s tiered approach to Ebola and other special pathogens simply don't have a choice when it comes to changing, and it has nothing to do with money, countered Dr. John Sellick, a professor of medicine at University at Buffalo.
In his role as an epidemiologist for both the VA Western New York Healthcare System and Kaleida Health system in New York, it’s Sellick’s job to keep hospitals free of infectious disease. None of the hospitals he works for are part of HHS’s Ebola preparedness networks, but Sellick said that the events of 2014 made changes like travel screening questions and proper isolation technique a nonnegotiable part of hospital life.
“In a perverse way, [the Ebola outbreak] had a positive impact on what we do,” said Sellick. “We all have to be prepared for at least the first line of triage, whether it’s Ebola, Marburg or MERS corona virus,” he continued. “You can’t just put a sign on the door that says, ‘No Ebola patients.’"
Dr. Ken Sands, senior vice president of health care quality and safety at Beth Israel Deaconess Medical Center in Boston, agrees. Initially, Sands’ hospital was listed as an Ebola assessment hospital in Massachusetts, but after discussion with the state’s health department, the institution surrendered the designation to other facilities better equipped for the task. However, that didn’t stop Beth Israel from continuing to build out an isolation unit at the hospital’s own expense.
"The very large majority of hospitals voluntarily stepped up and increased their capability and did an enormous amount of training, and equipment purchase and renovation, in order to be ready for Ebola response,” said Sands. "It was admirable."
And while Sands, who is also a spokesman for the American Hospital Association, agrees that there is “no way” to maintain even Ebola assessment capabilities at all hospitals, he called the 2014 outbreak a wakeup call about exotic pathogens in general.
“The predominant wisdom is that we should use the Ebola experience not to say, ‘Let’s make sure we’re good at Ebola,' but to make sure we’re good at highly contagious pathogens as a category,” said Sands. "The general awareness level has been increased, and the ability to follow those protocols successfully and consistently has probably improved."
‘You don't know what that cough is'
The Minnesota toddler’s MERS test results came back in less than 24 hours. The diagnosis: rhinovirus and parainfluenza, or, in other words, the common cold and the flu. But his ultimately ordinary case doesn’t mean staff had wasted time and resources to take extra precaution, said Stinchfield, CHCM's director of pediatric infectious disease.
On the contrary, the new protocol showed that the hospital staff had successfully increased their vigilance about ways to protect workers and other patients from potentially lethal contagion. And for emergency room vets who may think they’ve become immune to all manner of illness, the heightened awareness that came from Ebola has, at the very least, renewed their individual commitment to personal protective equipment.
"You can get a little lackadaisical wearing a mask with a coughing child, but you don’t know what that cough is,” said Stinchfield. "Is it whooping cough? Is it the common cold? Is it tuberculosis? It’s a cough, and we won’t know until we test the patient."
[This story was originally published by The Huffington Post. Graphics by Alissa Scheller and Abigail Williams.]

