‘We want people to live’: How San Antonio is trying to prevent deaths from blood loss
The story was originally published by the The Dallas Morning News with support from our 2022 National Fellowship.

San Antonio Fire Department medical officer Lt. Bill Bullock (center) and firefighter/paramedic Keith Eldard worked on a victim of an auto/pedestrian accident on the city's west side on Nov. 16, 2021. Bullock was instrumental in instituting the transfusion of whole blood to trauma victims along with the San Antonio Fire Department.
Jerry Lara / San Antonio Express-News
SAN ANTONIO — The way Dr. Donald Jenkins sees it, what saves lives on the battlefield could save lives on streets across America.
During nearly 25 years in the Air Force, Jenkins operated on troops with devastating wounds from bombs and bullets — ones not so different than those that ordinary people sustain from cars, gun violence and random accidents. Injuries he saw from rollover crashes in combat zones are similar to those from high-speed highway wrecks. Gunfire tears through tissues and vital organs the same if it comes from an enemy combatant or a licensed gun owner.
From his deployments, Jenkins knew that a single factor — bleeding, and how well it was controlled before patients landed on his operating table — dictated survival. Those who received blood quickly, especially on the way to the hospital, were more likely to remain stable during surgery and recover. Without it, death could come in a matter of minutes.
The same is true for everyday Americans, who regularly bleed to death before doctors can repair their injuries. But unlike in combat zones, where military medics usually have blood on hand, in the U.S. there haven’t been any broad or comprehensive efforts to give blood to hemorrhaging patients before they arrive at a hospital. The best most paramedics can offer their patients is saline and medications that slow bleeding.
Why not treat them the same, Jenkins wondered years ago, after he left the military and began a new medical career as a civilian. If patients needed blood when they arrived at the hospital, surely they needed it before then, too. Why not give patients blood as soon as possible, when they need it most?
Five years ago, in San Antonio, a city with strong military ties, Jenkins finally got the chance to test his idea to put blood on ambulances and helicopters across the region.
Today, Jenkins’ theory has turned into one of the country’s most innovative and pioneering models of advanced care, an example of how access to blood soon after a traumatic incident can save lives, some of the nation’s leading trauma researchers say. Across the U.S., a growing number of EMS providers have replicated parts of San Antonio’s blood program, helping critically injured patients in cities like Austin, New Orleans, Seattle, Oklahoma City and Pittsburgh and in South Florida — often with advice from San Antonio’s trauma leaders.
“We have very openly exported all of our ideas, our protocols and our data,” said Jenkins, a trauma surgeon with UT Health San Antonio and University Hospital. “We’re not looking for a patent. We’re not looking to make money off of this. We just want to see people live.”
Since the South Texas program’s start in 2018, more than 2,100 patients have received blood transfusions on the way to a hospital. Many were car crash and shooting victims, including a 37-year-old mother of two in San Antonio who was clinically dead after a car crash when blood revived her. There were also patients bleeding from pregnancy complications and other medical problems.
We’re not looking for a patent. We’re not looking to make money off of this. We just want to see people live.
Dr. Donald Jenkins
Early research from the program has found trauma patients who received transfusions before reaching a hospital were more likely to survive the immediate aftermath of their injury, which medical experts consider to be the most critical period.
Longer term survival rates remain the subject of study. Already, there have been remarkable success stories, lives that likely would have otherwise been lost, according to the paramedics who treated them. They include a South Texas man who severed arteries in his arm while working with a tool at home and an oil field worker in his early 20s who suffered a partial leg amputation while working with a malfunctioning drill.
“We’re providing the patients with what they need, when and where they need it,” Jenkins said.
Every day, trauma physicians and paramedics confront a deadly public health crisis. Traumatic injury is a major cause of premature death, killing around 150,000 Americans each year, including more children and adults under age 45 than any other cause. In 2021, Texas led the nation in deaths from motor vehicle crashes and guns, federal data shows.
A yearslong investigation by The Dallas Morning News and the San Antonio Express-News has found tens of thousands of these injured patients are dying from wounds they could have survived had they received crucial treatments sooner. Some of the nation’s most respected researchers estimate that, each year, 31,000 Americans bleed to death from survivable injuries, with lifesaving transfusions usually out of reach until patients arrive at a hospital.
In more than 140 interviews, the news organizations found paramedics are unequipped to fully treat severe internal bleeding and patients receive drastically different care depending on where they are injured.
After decades of inadequate federal funding for research and little attention by elected officials, outcomes for these patients remain poor and have stagnated over the past decade, the investigation found. Federal officials have failed to adopt major reforms that could save lives, even after being confronted in 2016 with growing evidence that large numbers of injured patients are needlessly dying every day.
‘LIQUID GOLD’
The idea for San Antonio’s blood program began in a war zone in October 2001, on Masirah Island off the coast of Oman.
There, Jenkins was the first surgeon to enter the combat zone, standing by as special forces parachuted into southern Afghanistan. Over the next two weeks, he treated dozens of injured troops.
Back home, hospitals had stockpiles of dozens of blood components — oxygen-carrying red blood cells, circulation-promoting plasma and clot-facilitating platelets.
Jenkins and the military medical team made do with what they had, tapping service members to give blood.
When he gave this fresh blood to wounded troops, he was stunned by how quickly it worked. Before his eyes, they came back to life. Within minutes, vital signs normalized, color returned to their skin and they regained consciousness.
This was both a departure from what Jenkins had learned in medical school and a return to the foundation of transfusion science.
Since World War I, military doctors have treated wounded soldiers in shock with whole blood, which is largely unmodified after it is collected from donors. The practice continued into the Vietnam War, with the military shipping hundreds of thousands of units overseas, where surgeons administered it to casualties with few complications.
The 1970s brought seismic changes to blood banking and medicine. Doctors increasingly treated medical conditions that only needed certain parts of blood — red blood cells for anemia or platelets for cancer patients. To accommodate doctors’ desire to tailor treatments, blood banks began separating blood into its three main components. With triple the number of products available to sell to medical providers, the industry also reached more patients with a single donation.
This made sense for nonemergency patients, but it was a drastic change for trauma patients who rapidly bled out, said Dr. Bryan Cotton, co-director of the shock-trauma intensive care unit at Memorial Hermann-Texas Medical Center in Houston. The simplest treatment was whole blood — which had largely disappeared from the supply.
“They did it with zero data saying it was safe for bleeding patients,” he said. “They could do it, but they didn’t really show if they should do it.”
Around the same time, emergency medicine specialists started relying more on another product for stabilizing bleeding patients: saline.
On ambulances, blood transfusions were impractical as each component had different storage requirements and expiration timelines. Saline was cheap, stored at room temperature and was disease-free.
Dr. G. Tom Shires, a surgeon with UT Southwestern Medical School in Dallas, had found limited amounts of salt water could help maintain the blood pressure of injured patients. But in his published papers, he cautioned saline should be given before blood was available, not as a replacement.
The medical community did not heed those warnings.
Paramedics began pumping patients with as much as 1 to 2 gallons of saline — so much that their blood turned pink. Dr. Mark Yazer, a professor of pathology at the University of Pittsburgh, said intensive care unit patients in the 1990s were often so swollen with saline, they resembled “the Michelin Man.”
By the time Jenkins began working as a surgeon, it was common to give hemorrhaging patients large amounts of red blood cells to restore oxygen and saline to stabilize blood pressure while minimizing plasma and platelets — a combination very different from blood in the body. Paramedics also avoided using tourniquets for fear they would lead to amputations.
During his deployments to Iraq and Afghanistan, Jenkins and other combat surgeons quickly became whole blood converts. A single bag neatly contained everything bleeding patients needed — oxygen, nutrients, proteins that help blood clot, fluids for circulation. It was also more potent than multiple units of components, which were diluted by more additives for storage.
It was like “liquid gold,” Air Force Col. Valerie Sams said.

Although many blood banks are hesitant about administering blood outside the regulated environment of hospitals, the South Texas Blood and Tissue Center wanted to expand the blood supply, not just redirect donations that normally went to hospital patients.
Bob Owen / San Antonio Express-News
“Once we start that whole blood resuscitation, you can see everything start to correct,” said Sams, who previously served as trauma director of the military hospital at Afghanistan’s Bagram Airfield.
Whole blood, and tourniquets, became staples in the wars. From 2003 to 2017, the U.S. military administered more than 10,000 units of blood, often as medics evacuated casualties.
In 2007, Jenkins was among a group of military doctors who introduced a new approach to control bleeding in severely injured troops. They recommended rapid transfusions of fresh whole blood and components, as long as they were given in the same amounts found in the body. Saline should only be given in small volumes.
Retrospective studies supported what Jenkins and Sams had observed: Transfusions of any kind before patients reached a hospital and giving fresh whole blood when they arrived were linked to better long-term survival rates.
Multiple deployments, including a stint overseeing all medical care in Iraq, made one thing clear to Jenkins. Much of his medical training had turned out to be wrong.
Forgoing tourniquets prioritized limbs over lives. Patients who received components that did not fully substitute whole blood fared worse. Too much saline, which contained no oxygen or blood-clotting elements, actually aggravated bleeding and inflammation in trauma patients.
None of it, Jenkins thought, made sense.
BUILDING A BLOOD PROGRAM
The power of whole blood on the battlefield stayed with Jenkins after he retired from the Air Force and entered academic medicine.
In 2013, as the medical trauma director at the Mayo Clinic’s Saint Marys Campus in Rochester, Minn., Jenkins asked the hospital’s transfusion division if it could provide whole blood for trauma patients. Lab workers conferred with trauma staff, federal regulators and accreditation bodies.
In 2016, the hospital rolled out type O whole blood in its trauma and critical care department and helicopter service.
Later that year, Jenkins moved to San Antonio and joined the faculty at University Hospital. The city was full of combat surgeons at Joint Base San Antonio, including at Brooke Army Medical Center, the Department of Defense’s only Level I trauma center. The hospital treated civilian trauma patients to train and maintain the readiness of military medical teams.
It was the type of place that would be receptive to his vision of providing military-caliber care to civilians, Jenkins believed.

Elizabeth Waltman, CEO of South Texas Blood and Tissue Center, spoke about how the use of whole blood transfusions is saving more lives in trauma cases on Dec. 11, 2019. As chief operating officer of blood services at the blood bank in San Antonio, she is responsible for maintaining the blood supply for injured patients across the region.
Bob Owen / San Antonio Express-News
That summer, he attended an international meeting in Norway of military experts who were interested in improving care for traumatic bleeding.
During the presentations, Elizabeth Waltman had an epiphany. As chief operating officer of blood services at South Texas Blood and Tissue, a blood bank in San Antonio, she was responsible for maintaining the blood supply for injured patients across the region. Just as Jenkins had realized years before, she considered how similar military injuries were to those in civilian patients.
We’re having the same problems back home, she thought. Shouldn’t the solutions be the same, too?
Later, she talked to one of the speakers seated behind her about what whole blood could do for American patients. That man was Jenkins.
I want to do this in San Antonio, she told him.
Well, I’m in San Antonio, he responded, to her surprise.
After returning to Texas, the pair had lunch with Eric Epley, executive director of the Southwest Texas Regional Advisory Council, which coordinates trauma systems in San Antonio and 22 South Texas counties.
Jenkins was adamant that the program include the region’s EMS providers.
After that, there were many details to iron out. Few emergency providers across the country carried blood because it was costly and supply was limited. Many blood banks were also hesitant about administering blood outside the regulated environment of hospitals.
The San Antonio group decided to use a form of O-positive whole blood that can be given to all patients. The blood bank would need money to pay for bags and testing and would need to create a pool of donors. They wanted to expand the blood supply, not just redirect donations that normally went to hospital patients.
To prevent the blood from spoiling, EMS providers would use portable coolers and several layers of monitoring to ensure the units stayed within the proper temperature range. Paramedics warmed the blood back up to avoid worsening patients’ shock.
Incidents of trauma and medical bleeding were impossible to predict, which posed another question. How would they ensure the blood on ambulances and helicopters would not go to waste?
The solution they found was as economical as it was elegant.
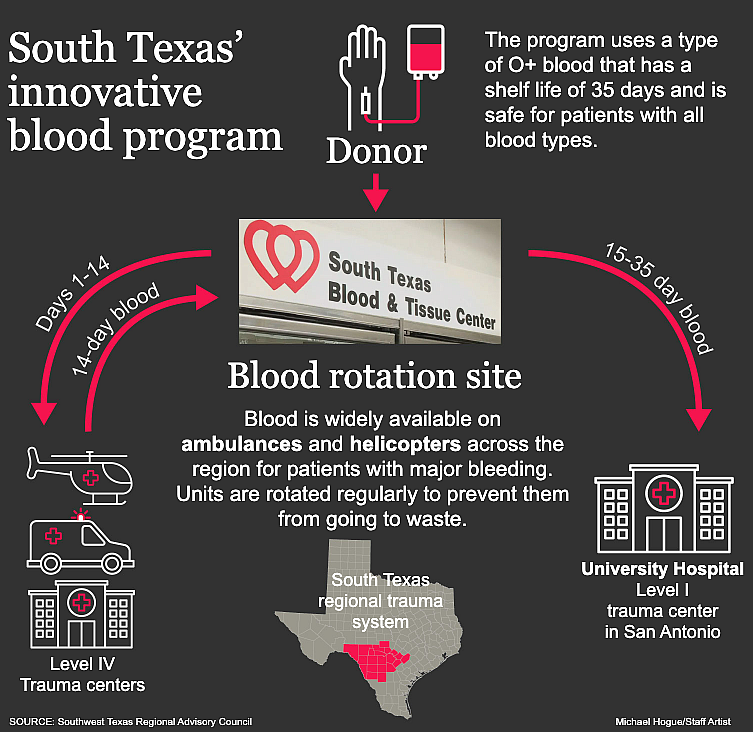
For two weeks, EMS providers would keep the blood on hand. Any units that remained unused would be returned at no cost and sent to University Hospital’s trauma bay, where there was always a need for blood. This rotation system allowed rural EMS providers to participate: They needed blood less frequently but their patients were at greater risk of dying during longer transports.
With a $150,000 grant from the San Antonio Medical Foundation, the program started in January 2018, first on regional helicopters. That October, San Antonio Fire Department supervisor vehicles and some ambulances began carrying blood to the most serious calls.
Dr. CJ Winckler, the department’s deputy medical director and an associate professor at UT Health San Antonio, said the program was intuitive. They were giving blood to the same patients who, if they were in a hospital, would immediately receive transfusions. All they were doing, he said, was bringing the hospital to the patient.
That standard of care was a radical change from when Winckler worked as a paramedic in Austin in the early 2000s. While Jenkins was administering whole blood overseas, Winckler was giving liter after liter of saline to hemorrhaging patients.
“I wish I would have known then what I know now,” he said.

San Antonio Fire Department Medical Officer Lt. Bill Bullock arrived at the scene of a shooting in 2021. A man was standing outside his residence when he was shot with an assault-style weapon. As he was transported to Brooke Army Medical Center, he was given an infusion of whole blood to stabilize his blood pressure.
Jerry Lara / San Antonio Express-News
Winckler is grateful that, at the request of fire Chief Charles Hood, the San Antonio City Council agreed to pay for the blood. At about $500 per bag, the fire department cannot recoup those costs through medical billing. Medicare and Medicaid, and most major insurers, do not pay for blood transfused outside of a hospital.
According to an analysis published in the journal Prehospital and Disaster Medicine in 2019, the projected average cost for San Antonio paramedics to “save a life” at year 10 of the blood program will be $5,244. By regularly moving unused blood from ambulances to hospitals, less than 1% goes to waste.
For longtime paramedics, the program has been invigorating.
“They say things like, ‘I’m excited about medicine again. We are saving lives, doc. I’m telling you, this is working,’” Winckler said.
BLOOD ONBOARD
The program was transformational for Lt. Bill Bullock, who for most of his two decades in EMS, could only do so much for patients with life-threatening bleeding.
The tools he had — tourniquets, blood clotting medications and wound dressings — could help slow some types of bleeding. What he didn’t have was the one thing that hemorrhaging patients, especially those with internal injuries, really needed.
That all changed when the San Antonio Fire Department began participating in the South Texas blood program. Supervisors like Bullock, who responded to the most urgent calls, carried coolers with a unit of blood wherever they went.
With that blood on his truck, Bullock has administered blood to dozens of patients — children who have been shot, a woman stabbed by her boyfriend and another who was eight months pregnant when she was found sitting in a pool of blood in her bathtub.
Each time, he knew he was giving them a better chance of making it to the hospital where their bleeding could be stopped. Sometimes when he dropped off patients, he crossed paths with Jenkins outside University Hospital’s trauma bay.
In late 2021, this reporter spent more than 40 hours shadowing Bullock as he responded to major trauma calls.
Late one night that November, Bullock and other medics entered a house littered with bullet casings. They walked over blood-smeared tiles to reach a man who had been shot in the chest and arm.
He and his colleagues sheared off the man’s white, blood-soaked shirt and tightened a tourniquet around his arm, where a bullet had blown apart his biceps muscle.
In the back of an ambulance, Bullock and two medics worked to keep the man conscious as they sped toward the hospital, sirens blaring. They administered the standard treatments for an injured patient, including fluids and medications for pain, as they worked to slow the bleeding.
Even so, the man’s eyes were glassy, expression dazed, skin coated in a sheen of sweat. He was there. Barely.
“All right, this is gonna hurt, man,” one paramedic warned the patient. “I believe that you got a collapsed lung.”
By the patient’s head, Bullock called out to the ambulance driver that they were about to insert a needle into the patient’s chest to release trapped air. It was a delicate procedure that required smooth driving. Then he glanced down.
“You OK?” Bullock asked. “Breathing, right? That’s your job.”
The patient half mumbled, half groaned an unintelligible response.
How many times had Bullock watched patients like this man slip away?
Not anymore.
Bullock reached for his cooler and pulled out a bag of blood. He handed it to Jose Cortinas, who had been on the job for only about six months and had never done a transfusion. Cortinas squeezed the bag with his hands to force the blood down the tubing.
“Blood pressure went up,” said Michael De La Rosa, another medic. “Went way up.”
“Beautiful,” Cortinas said.
The blood was still flowing as paramedics wheeled the man into Brooke Army Medical Center. They had bought him valuable time.
GALLERY: Go on a blood call with San Antonio paramedics

A gunshot victim was given whole blood as he was transported to Brooke Army Medical Center in San Antonio on Nov. 25, 2021. The San Antonio Fire Department participates in the South Texas blood program, and supervisors like medical officer Lt. Bill Bullock carry coolers with a unit of blood wherever they go.
Jerry Lara / San Antonio Express-News

A gunshot victim was given whole blood as he was transported to Brooke Army Medical Center in San Antonio on Nov. 25, 201.
Jerry Lara / San Antonio Express-News

San Antonio Fire Department medical officer Lt. Bill Bullock(right) talked with personnel at the scene of an accidental shooting on Nov. 17, 2021. Bullock was instrumental in instituting the transfusion of whole blood to trauma victims. The man had accidentally shot himself in the thigh and refused medical treatment.
Jerry Lara / San Antonio Express-News

San Antonio Fire Department medical officer Lt. Bill Bullock retrieved equipment at an auto/pedestrian accident during his shift on the city's west side on Nov. 18, 2021.
Jerry Lara / San Antonio Express-News

San Antonio Fire Department medical officer Lt. Bill Bullock filled out paperwork as he got whole blood from the South Texas Blood and Tissue Center on Nov. 17, 2021.
Jerry Lara / San Antonio Express-News
<--img-5,6,7,8,9-->
SAVING MORE LIVES
By the time San Antonio paramedics started carrying blood, nearby EMS providers were eager to participate in the program.
The year before the blood program began, a shooter had killed 26 churchgoers and wounded 22 others in the rural town of Sutherland Springs in neighboring Wilson County. Paramedics had faced a gruesome scene: dozens of bleeding patients who were 30 to 45 miles away from San Antonio’s trauma centers.
David Rice, a Wilson County paramedic who responded to the shooting, said having blood could have helped them save as many as half of the victims.
“They simply bled out,” said Rice, EMS director for the county’s Emergency Service District No. 3.
As San Antonio’s trauma leaders shared details about their program at conferences and in medical journals and EMS trade publications, paramedics from nearby counties and beyond came calling. They also heard from interested emergency providers across the country — so many that they began offering two-day bootcamps to share their practices.
The findings from San Antonio’s program add to a growing body of research linking early access to blood transfusions to better survival rates for seriously injured patients.
After a national randomized trial, researchers wrote in the New England Journal of Medicine in 2018 that transfusions of plasma during air medical transports cut the risk of death at 30 days by 39 percent. In 2021, the same research group found improved survival rates in helicopter patients who received a combination of red blood cells and plasma on the way to the hospital.
At Tulane University School of Medicine in Louisiana, Dr. Juan Duchesne had dedicated his career to improving the care of trauma patients. He led studies showing hospital advances in bleeding control, including a transition to whole blood and putting a blood refrigerator in the emergency department, were not enough to improve survival rates.
No matter how fast doctors and nurses treated hemorrhaging patients at the hospital, around half were still dying.
Like Jenkins, Duchesne did not understand why so many physicians could not see what was so clear to him. Something had to be done sooner, before patients got to him.
In 2019, he began talking with paramedics in New Orleans and San Antonio to plan for a mobile blood program in New Orleans.
In late 2021, paramedics there began field transfusions of red blood cells on the scene and in ambulances. They even transfused patients without a pulse on the chance they might get one back. In 15 cases, they did.
There are a few things in medicine where you can really make a big difference and save somebody’s life. Most of what we do is not as dramatic. But this is an area where we really can save someone’s life and send them back to their families.
Dr. Meg Marino
Dr. Meg Marino, medical director for New Orleans EMS, considers the program an invaluable asset in a community where gun violence and stabbings accounted for 85 percent of 204 transfusions by paramedics through early October of this year. At a conference in September, Duchesne presented preliminary data from the program showing the blood products, administered alongside medications that help slow bleeding, improved 24-hour and hospital survival rates for injured patients.
“There are a few things in medicine where you can really make a big difference and save somebody’s life. Most of what we do is not as dramatic,” said Marino, who previously worked as an emergency medicine physician at Texas Children’s Hospital in Houston. “But this is an area where we really can save someone’s life and send them back to their families.”
AT DEATH’S DOOR
In a water-filled ditch, off the side of a road on San Antonio’s Far West Side, Tiffany Kieschnick-Rivas was dead.
The 37-year-old mother of two was driving to a gas station in January 2019 to get an ICEE for her son when everything went dark.
Without warning, she suffered a stroke and her car careened into a concrete ditch. Bystanders found her contorted in the passenger seat.
From the outside, she appeared unharmed, aside from a cut on her face. Internally, her spleen was hemorrhaging, causing blood to pool in her abdomen.
As emergency responders rushed to extricate Tiffany, she stopped answering their questions and began gasping for air, her face pale.

Tiffany Kieschnick-Rivas (center), who nearly died after a stroke caused her to crash her car into a ditch, is embraced by her son, Ashton, and wife, Sandra, during a Jan. 30, 2020, visit to the crash site on Galm Road in San Antonio on the one-year anniversary of the crash. Transfusions of whole blood at the scene and during transport revived her. Pieces of her car still could be seen in the ditch a year later.
Billy Calzada / San Antonio Express-News
By the time they pulled her from the wreck about a half-hour after the crash, she had no pulse.
Over the next five minutes, paramedics intubated her and administered CPR with a machine. They regained a pulse, but her blood pressure remained dangerously low. They were on the verge of losing her again.
This time, they reached for something they had only begun carrying a few months earlier: a bag of whole blood.
Mid-transfusion, Tiffany began blinking and moving her limbs. The paramedics were shocked.
During the 11-minute flight to University Hospital, she received another pint of blood, and upon arrival, red blood cells and plasma.
In addition to her spleen injury, doctors determined Tiffany had suffered fractures to her face, multiple vertebrae and a rib. A radiologist stopped her bleeding with a catheter. She also needed surgeries to repair her spine, shoulder and knee. During her stay in the intensive care unit, Jenkins was one of the doctors who treated her.
Twelve days later, Tiffany went home to her family.
On the one-year anniversary of the crash, in January 2020, she revisited the site, where debris from her car was still strewn across the ditch. Her sons Austin and Ashton, 10 and 14, marked the spot with balloons and an oversized teddy bear.
That evening, Tiffany stood before friends and family at a barbecue restaurant to talk about how the crash had changed her life.
There, beaming, was Winckler, who oversaw the paramedics who saved her. He had visited her in the hospital and was publishing a case study about her remarkable recovery. There, too, were the good Samaritans who helped her, including a teenager who called for help and an Army sergeant who held her head above the ditch’s standing water. Two of the paramedics who treated her. And one of the donors whose blood ran through her veins.
For Winckler, Tiffany’s story is a testament that what they’re doing is important, despite skeptics in his field who want to see more robust evidence before investing in prehospital blood.
Few randomized trials exist in this area, and it can take years for researchers to gather enough data to show meaningful long-term mortality differences. While medical experts agree prehospital blood can save lives, they have differing opinions on which patients benefit the most and the type of blood products that should be used.
Winckler is confident that, with time, data will reflect what he and the department’s paramedics already know.
This is what’s best for patients.