Challenging Misconceptions About Dementia Among Chinese Immigrants
The story was co-published with World Journal as part of the 2024 Ethnic Media Collaborative, Healing California.

Image by Sabine van Erp from Pixabay
“My father, Xiaohong Wang, 70, was lost around 4:30 p.m. near Old Town La Puente. He can’t speak English, and his Mandarin has a Ningbo accent. No identification on him…”
It was10 p.m., when Angela Khang reported her father’s disappearance to a police officer at the Los Angeles County Sheriff’s station in Industry, California.
Three days later on June 7, Khang found her father in a hospital bed at the El Monte Community Hospital, about 10 miles away from their home. A Cantonese-speaking tire shop owner found her father in a desperate situation and called the police. Her father had been lying on the ground under a tree, wrapped in a plastic bag, and exposed to the elements at night. By the time he arrived at the hospital, he was severely dehydrated, which led to kidney damage and extreme weakness.
“He couldn’t remember my phone number, our home address, or even what neighborhood he was in. He had no idea how to ask for help,” Khang said. After hearing her father’s account of how he got lost, she sensed something was wrong with his thinking, so she took him for a brain health check.
Brain scans revealed that her father had mild brain atrophy, a sign of dementia.
"Crazy Seniors"
Before her father went missing, Khang had already noticed that her once-sharp father seemed to be “getting forgetful,” struggling to remember daily routines he had performed repeatedly. "I thought poor memory was a natural part of aging," Khang said.
She is not alone in believing this. A global survey revealed that 80% of the general public still incorrectly believes dementia is a normal part of aging rather than a medical condition. More than half of Asian Americans believe that significant loss of memory or cognitive ability is a normal part of aging.
“There are many misunderstandings. Most Chinese immigrants I have interacted with have a rather vague understanding of dementia; they are not sure about the difference between dementia and Alzheimer’s disease, which is a brain disorder requiring diagnosis and treatment,” said Benson Zhao, a Bay Area, California, community engagement manager at the Northern California and Northern Nevada Chapter of the Alzheimer’s Association.
According to the Alzheimer’s Society, “The main difference between Alzheimer’s and dementia is that Alzheimer’s is a disease in the brain, whereas dementia is a collection of symptoms. Alzheimer’s disease causes cognitive decline, eventually leading to dementia. It’s the most common reason why people get dementia.”
“Some people may even ask, ‘If this disease can’t be cured, why bother with diagnosis and treatment?’” he added.
Like most Chinese immigrants, Khang used the term "老年癡呆” to refer to dementia. Among Chinese, this term is quite common. Despite many years of articles pointing out that the literal meaning — crazy seniors — is discriminatory, it remains the term most frequently used by Chinese. Even the Google Translate function continues to use this outdated discriminatory term for dementia in Chinese, rather than its neutral, clinical translation.
A recent online survey conducted by the World Journal revealed that the commonly used and negative Mandarin term for “dementia” carries significant emotional weight for patients. 'Mocked,' 'despair,' 'sadness,' and 'fear' are the words respondents used to describe their feelings about this traditional term.
“This term is incorrect!” Zhao said, explaining that the disease not only affects the elderly; some middle-aged individuals can also suffer from dementia in their 40s and 50s. More importantly, dementia is a neurological or brain disease, not a psychiatric condition. The patients are not crazy.
“This misleading terminology deepens the stigma surrounding the disease, making those who are already inclined to avoid discussing family misfortunes even less willing to open up about it or seek diagnosis or treatment,” Zhao said.
“I feel many Chinese families are reluctant to admit a family member has this disease, as if acknowledging it means there’s a ‘crazy person’ in the family,” said Kristy Huang-Arai, Senior Manager of Education and Outreach at Alzheimer’s Los Angeles, a nonprofit that is capable of providing support in Mandarin for Chinese families in the greater Los Angeles region.
Huang also said that stigma hinders people from developing a correct understanding of the disease, which leads to a lack of empathy for patients and insufficient preparation for caregiving.
"If language doesn't change, neither do perceptions," Zhao said.
Persistent Barriers
“Education, education, education” is what Zhao sees as the top priority for outreach efforts in the Chinese community right now.
However, the response from the community is often “We don’t need your help.” Zhao said that when organizing outreach events, it’s common to encounter resistance; some senior communities have turned them away, especially during the holiday season when they are even less willing to host activities on themes perceived as unhappy or unfortunate.

An outreach event in the San Francisco Bay Area on October 25.
Courtesy of Benson Zhao
According to a 2021 report from the Alzheimer’s Association, among all ethnic groups, Asian caregivers were the least willing to consider access to a care navigator to guide them through the healthcare system, facilitating their medical and nonmedical needs. Only 38% believe that having access to a care navigator would influence their decision when selecting a dementia health care provider for the person they are caring for.
There could be other reasons for this phenomenon.
The report found Asian caregivers expressed the greatest challenges, with 7 in 10 (68%) indicating that they found dementia care somewhat or very challenging. Most Asian caregivers (9 in 10) believe it’s crucial for care navigators to be aware of the cultural background of the person they are caring for, but their confidence in the navigator's understanding of patients’ cultural background was the lowest among all ethnicities.
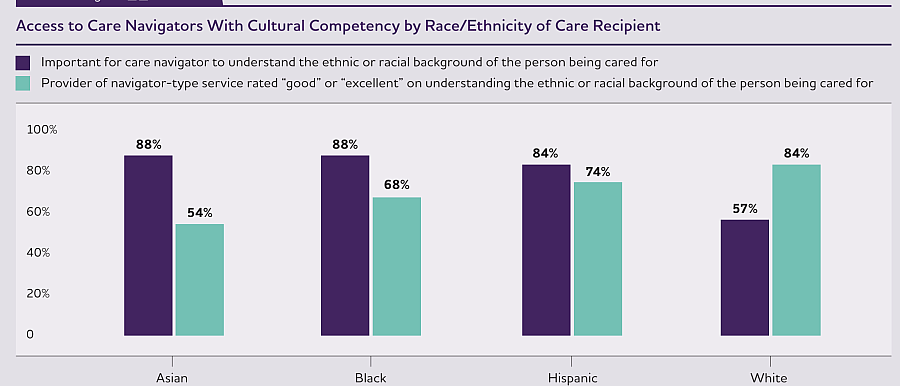
Courtesy of Alzheimer’s Association
Zhao emphasized when hosting outreach events on dementia and Alzheimer’s, cultural awareness and sensitivity is important. It’s important to address the stigma associated with this disease, and it helps to use positive words in describing the events, like “brain health,” and knowing how to communicate with Chinese seniors.
“You need to be proactive, but not too much,” Zhao shared, at outreach booths, collecting flyers and showing interest in learning more about the disease doesn’t necessarily mean they want your help. “If you, at this moment, ask whether their family or friends have experienced similar issues, many may feel anxious and walk away,” Zhao explained, by way of example.
In Khang’s house, she tried to avoid mentioning the disease in front of her father. “I worry about putting pressure on him, so I only ask the doctor when my father is not around.”
Missed or delayed diagnosis
As a minority group, Chinese Americans are at especially high risk for delayed diagnosis and suboptimal management of dementia. Chinese patients often delay seeking dementia care until the severe stages of neuropsychiatric symptoms when compared to white patients.
Attitudes toward dementia can lead to missed diagnoses and delayed detection,
However, patients and families may not be the only reason for delayed diagnoses.
A recent survey, revealed low confidence among primary care clinicians in diagnosing cognitive impairment, with many reporting that they felt only somewhat or not at all confident in diagnosing (70%) and managing care for (60%) cognitive impairment. Furthermore, among all ethnic groups, Asian American older adults had fewer diagnostic evaluation tests and assessments, and were least likely to receive a diagnostic work-up for cognitive impairment.
A number of studies identified communication problems, including perceived difficulty in disclosing or explaining the diagnosis of dementia, as barriers to accurate and timely diagnosis.
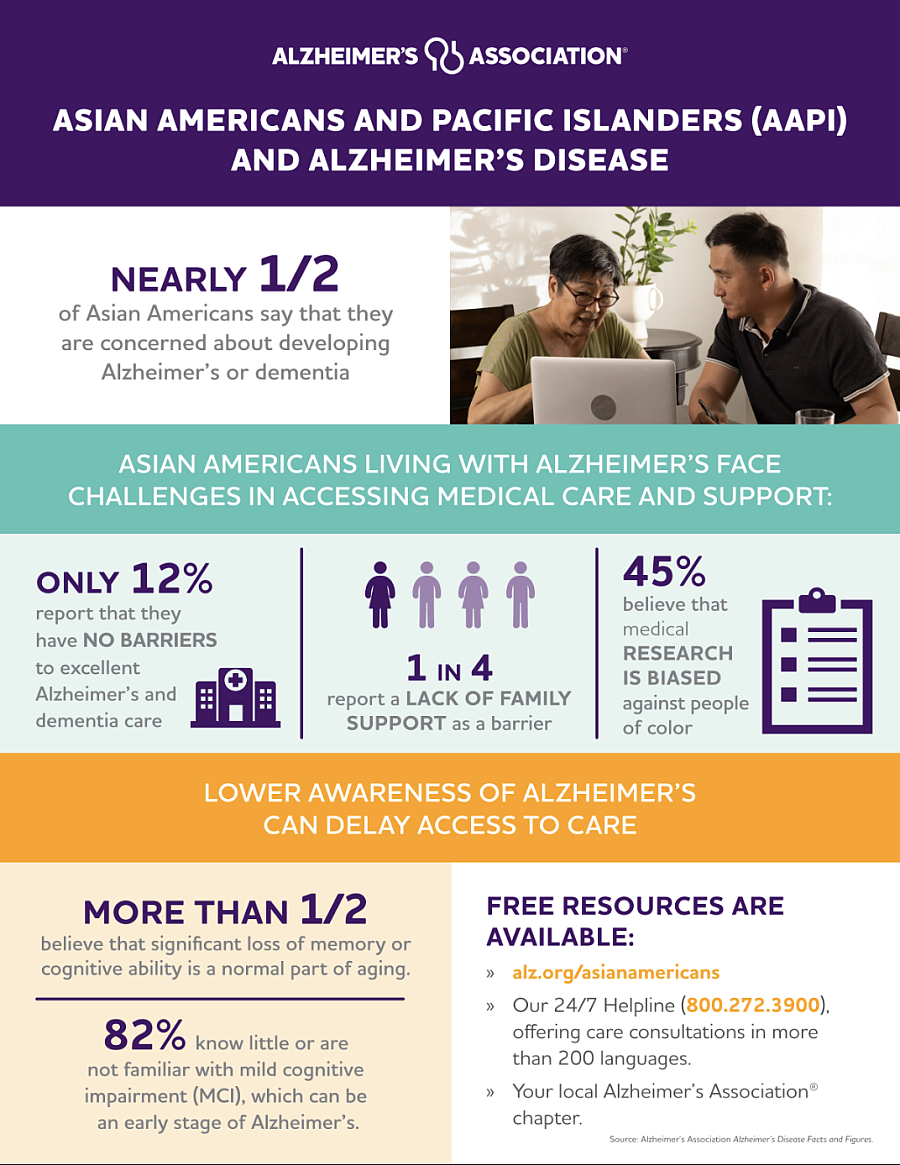
Infographic about AAPI group
Courtesy of Alzheimer’s Association
“Chinese-speaking neurologists are very rare. For patients and families who are non-native English speakers, understanding medical terminology can be a challenge, often resulting in them only comprehending half of the medical advice,” said Huang, citing feedback she has received from Chinese families. In the greater Los Angeles area, she knows only of two neurologists who speak Chinese.
World Journal’s survey , published in the November 4, found the most common reasons for not seeking medical treatment identified by respondents was ‘do not know what kind of help to seek’ (81.8%)and difficulty accessing medical resources(54.5%). The top resource they expressed a need for was information about the risks and treatment of the disease (75%), rather than financial assistance(25%).
Survey by Monica Vaughan and Jian Zhao
In Khang’s case, his daughter Angela had previously taken her father to see a doctor due to concerns about his forgetfulness and cognitive decline. However, the doctor did not recommend further brain examinations at that time, she said. Instead, the doctor suggested that the memory issues might be related to her father's heart problems, which could lead to insufficient oxygen making its way to the brain.
Zhao reminded family members that the early signs of dementia are often difficult to detect. When seeing a doctor, a patient’s first reaction might often be to deny the issue, which may occur unconsciously and is part of the symptoms of dementia. That’s one reason why it is essential for those around the person to remain attentive and not overlook these signs.
Doubled Risks and Challenges
The delays in diagnosing dementia can exacerbate disability, reduce treatment effectiveness, and increase healthcare costs. The negative health consequences among affected individuals can in turn impose caregiver burdens and reduce productivity, according to research based on 3,966 participants aged 70 and older.
"There's no cure for Alzheimer’s, but there are treatments that may slow disease progression and help manage symptoms," Zhao emphasized.
According to the Alzheimer's Association, Donanemab (Kisunla™) and Lecanemab (Leqembi®) both received traditional FDA approval to treat early Alzheimer's disease, including individuals with mild cognitive impairment or mild dementia due to Alzheimer's. The Alzheimer’s Association emphasizes that "it is important to seek a diagnosis as early as possible. The earlier you are diagnosed; the more treatment options will be available."
For Chinese patients, the dangers of delayed diagnosis are compounded.
On the second day after Khang's father went missing, a tipster who saw the missing poster called Khang reporting that her father had been seen riding a tricycle on the highway. After contacting the California Highway Patrol, Khang learned that an officer had spoken with her father on the highway. However, due to the language barrier and the absence of obvious signs of distress, the CHP officer escorted her father away from the highway but ultimately allowed him to leave.
“Many elderly Chinese have language barriers and have limited awareness of U.S. public services — some may not even know how to call or be able to call 911. This makes it extremely dangerous if they go missing,” Khang said.
“Wandering is like a ticking time bomb for families with dementia patients,” Huang said, "It's a common behavior in the early and middle stages of dementia, with over 60% of patients experiencing it, often without any prior warning. Therefore, advance preparation is crucial, such as upgrading door locks, using tracking devices, and keeping identification information in clothing pockets.
Since 2018, Los Angeles County has run the L.A. Found program, which provides free tracking wristbands for patients at risk of wandering, helping police locate them in emergencies.
(The public can apply online or call 833-569-7651 for more information.)
Free tracking wristbands for patients at risk of wandering.
Courtesy of L.A. Found
Huang mentioned that in some instances non-English-speaking patients can experience language regression. They may have spoken English, but as their condition worsened, their language abilities regressed to their native language.
This leads to another challenge: finding caregivers who speak Chinese. As the disease progresses, caregiving becomes more difficult, and many families require assistance. Huang noted, “There is already a shortage of caregivers for the elderly, and even fewer are equipped to handle the complex needs of dementia patients. Adding the requirement of speaking Chinese makes it even harder.” Families often ask her for help in finding care workers.
“If placed in a professional memory care unit, monthly costs can exceed $10,000 because such facilities require more staff and specialized design,” Huang said.
Navigating the Complexities of Dementia Care
Dementia is a progressive degenerative disease, with symptoms varying across its early, middle, and late stages. The timeline for progression is unpredictable and differs among patients.
“Caregivers need to be a detective,” Huang said, caring for someone with dementia is very different from caring for other illnesses. The goal of caregiving is not to help the patient recover but to improve their quality of life.”
Huang encouraged Chinese families to display empathy toward loved ones with dementia, viewing the world from their perspective. For instance, some Chinese families communicate with loved ones as if they are children, which may harm their self-esteem. Asking questions like “Who am I?” as a greeting or joke can further hurt their self-esteem by constantly reminding them of their condition.
Huang explained that caregivers’ behavior, responses, and words significantly impact the emotions of those they care for. Despite memory losses, the ability of those with dementia to perceive emotions remains intact.
In the later stages of dementia, patients often require 24-hour supervision. In many families, spouses and children are the primary caregivers. For low-income elders, In-Home Supportive Services (IHSS) can provide significant financial relief to families by covering the cost of caregiving needed, whether the care is provided by family members or care works.
However, for most families who do not qualify for government support, the burden is overwhelming. Statistic shows that 17% of caregivers for people diagnosed with dementia quit their jobs either before or after assuming caregiving responsibilities; 54% arrive late to work or leave early. The prevalence of suicidal ideation among dementia caregivers, with a mean age of 64, is 32%, compared to 2.7% in U.S. adults aged 56 and older.
World Journal’s survey findings shed light on the mental challenges of living with or caring for someone with memory loss. Participants reported difficulties such as an inability to communicate with the care recipients, lack of understanding from the care recipients, and feel emotional exhausted, among others.
Khang has personal experience — her grandmother was diagnosed with Alzheimer’s. “She would forget to turn off the stove or whether she had already taken her pills. Later on, my grandmother could not get out of bed, and everything needed to be taken care of. It was impossible to care for her alone; it required the whole family's effort.” Her grandmother passed away six years after the diagnosis.
Khang said she is still holding out hope, hoping her father’s condition is different from her grandmother’s, and hoping he’s just experiencing normal aging.

